Impact of clinical decision support guidelines on gentamicin TDM in
advertisement

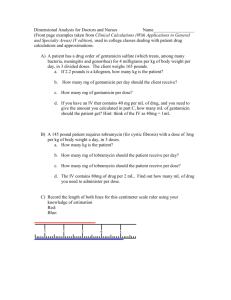
Impact of clinical decision support guidelines on gentamicin TDM in newborns Authors Caroline Fonzo-Christe MSc PhD1, Bertrand Guignard MSc PhD1, Claudia Zaugg MSc1, Ana Coehlo MSc1, Klara M. Posfay-Barbe MD2, Alain Gervaix MD PhD2, Jules Desmeules MD PhD3,6, Victoria Rollason MSc PhD3,6, Christophe Combescure PhD4, Regula Corbelli MD5, Peter Rimensberger MD PhD5, Riccardo Pfister MD PhD5, Pascal Bonnabry MSc PhD1,6 Author Affiliations 1Service of Pharmacy, 2Pediatric Infectious Diseases Unit, 3Service of Clinical Pharmacology and Toxicology, 4Clinical Research Center and Division of Clinical Epidemiology, 5 Neonatology and Pediatric Intensive Care Unit, Geneva University Hospitals, Geneva, Switzerland 6School of pharmaceutical sciences, University of Geneva/University of Lausanne, Switzerland Correspondence to Caroline Fonzo-Christe Service of Pharmacy, Geneva University Hospitals (HUG), Rue Gabrielle-PerretGentil 4, CH-1211 Geneva 14, Switzerland Tel: +4122/382.39.89, Fax: +4122/382.39.90 caroline.fonzo-christe@hcuge.ch APPENDIX – Guidelines for gentamicin therapeutic drug monitoring Dose regimen and administration of gentamicin in newborns ODD: once-daily dosing (interval: 24 hours) or EID: extended-interval dosing (interval > 24h) GENTAMICIN Targeted troughlevel ≈ 1 mg/L Gestational age (GA) [weeks] ≤ 29 30 – 34 ≥ 35 Postnatal age (PNA) [days] ≤7 8-28 ≥ 29 ≤7 ≥8 all Dose [mg/kg/dose] Interval [hours] 5 4–5 4–5 4–5 4–5 4–5 48 36 24 36 24 24 IV infusion over 30 min. Dilution with G5% or NaCl 0.9%, final concentration 0.1-2 mg/mL, (maximal concentration 10 mg/mL) TDM (therapeutic drug monitoring) Renal immaturity is considered in the dose regimen. Trough-level should be measured before the 3rd dose only when the treatment duration >48h. In case of renal dysfunction at the beginning of treatment, the “first-dose protocol” has to be applied. This protocol takes into account the accumulation of gentamicin that will occur. In the case of very high or very low measured levels, be sure that there was no overdosing, that intervals were neither too short nor too long, and that blood sampling was not inappropriate. If the treatment duration >10 days, repeat the TDM and consult an infectious diseases specialist. Peak level should not be monitored routinely. Indication: prescription of an unusual dose, isotonic dehydration, poor response. Monitor level after the 3rd dose, 30 min after the end of the IV infusion. STANDARD REGIMEN, MONITORING AT STEADY STATE Targeted trough-level ≈ 1 mg/L Troughlevel < 0.5 mg/L > 2 mg/L > 3 mg/L Peak level < 5 mg/L > 10 mg/L Current interval Management 24 hours If dose is correct, continue treatment without any change 36 hours Reduce interval to 24 hours, and check level after two doses 48 hours Reduce interval to 36 hours, and check level after two doses 24 hours Increase interval to 36 hours, and check level after two doses 36 hours Increase interval to 48 hours, and check level after two doses 48 hours Do not give the next dose, and check level after 24 hours (correct for age) Do not give the next dose, and check level after 24 hours To monitor only if indicated: targeted peak level 5-10 mg/L or 8-10x MIC Management Increase dose proportionally to the desired peak level increase; if trough-level >0.5 mg/L : increase also the interval of about one-half life (estimated). Reduce dose proportionally to the desired peak level decrease FIRST-DOSE PROTOCOL – suspicion of renal dysfunction (diuresis < 1.0 mL/kg/h at two days of life and more) Give the first dose in accordance with the dose regimen, check level 24 hours after the first dose < 1.1 mg/L Give the next dose, and continue with a 24 hours interval 1.2 - 2.3 mg/L Give the next dose in 12 hours, and continue with a 36 hours interval 2.4 - 3.2 mg/L Give the next dose in 24 hours, and go on with interval of 48 hours > 3.3 mg/L Do not give the next dose, and monitor level after 24 hours