Valve surgery
advertisement
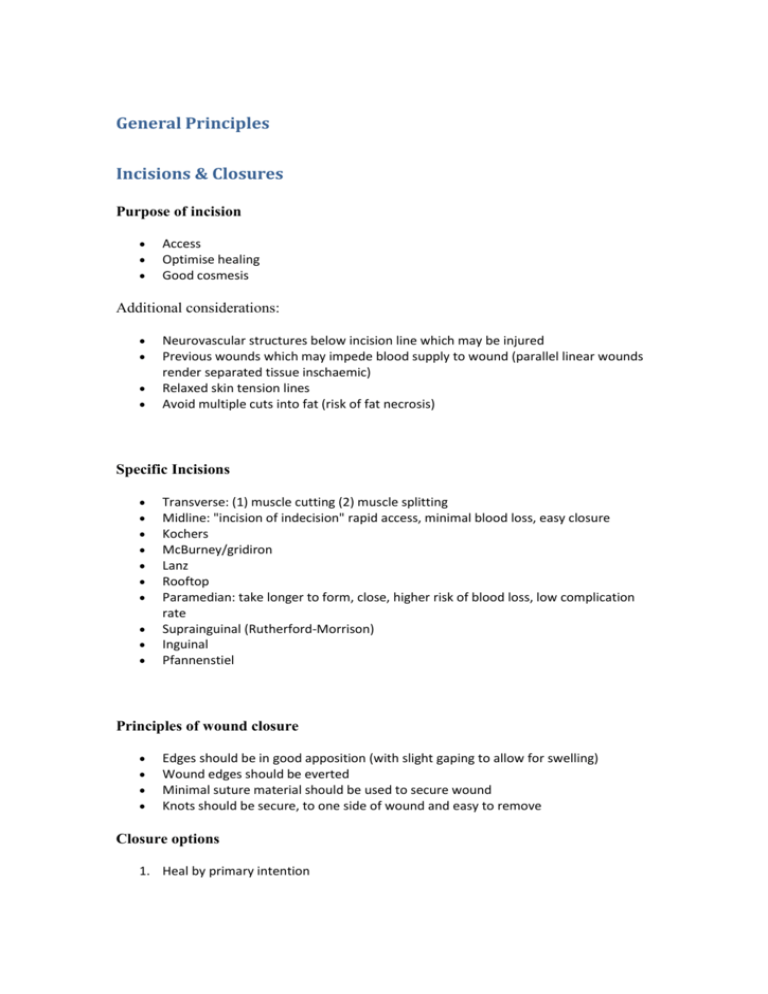
General Principles Incisions & Closures Purpose of incision Access Optimise healing Good cosmesis Additional considerations: Neurovascular structures below incision line which may be injured Previous wounds which may impede blood supply to wound (parallel linear wounds render separated tissue inschaemic) Relaxed skin tension lines Avoid multiple cuts into fat (risk of fat necrosis) Specific Incisions Transverse: (1) muscle cutting (2) muscle splitting Midline: "incision of indecision" rapid access, minimal blood loss, easy closure Kochers McBurney/gridiron Lanz Rooftop Paramedian: take longer to form, close, higher risk of blood loss, low complication rate Suprainguinal (Rutherford-Morrison) Inguinal Pfannenstiel Principles of wound closure Edges should be in good apposition (with slight gaping to allow for swelling) Wound edges should be everted Minimal suture material should be used to secure wound Knots should be secure, to one side of wound and easy to remove Closure options 1. Heal by primary intention 2. Heal by secondary intention +/- VAC, large surface area wounds, large cavitating wounds 3. Delayed primary closure 4. Steri-strips 5. Tissue glue 6. Skin staples 7. Sutures o Subcuticular - good cosmesis, suitable for clean linear wounds o Simple interrupted o Vertical mattress o Horizontal mattress Pre-operative preparation Pre-Induction Identify patient, operation, site, side, starved, allergies Check blood available Check investigations Check imaging Removal of body hair Remove from operative field Allow for clear surface for application of dressings Perform on morning of surgery Care to avoid cuts/abrasions Skin preparation Apply to operative field with wide margin (in case need to extend incision) Start at focus and move around 1. Chlorhexidine (0.5%) 2. Alcoholic betadine (1% povidine in 70% alcohol) Field Draping Sterile linen drapes Disposable fabrics (impermeable and waterproof), expensive Polyurethane incisible drapes (clear stuff) used in orthopaedics/vascular, general surgery - limited by cost Trauma / ATLS Management of Trauma Urgent and competent assessment of trauma Treat life-threatening injuries first Improve survival and outcome in "golden hour" 1. Primary Survery o Airway o Breathing o Circulation o Disability o Exposure, temperature control 2. Monitoring o ECG, Pulse oximetry, BP o Urinary catheter (unless contraindicated) o NGT 3. Radiology o CXR o Lateral C-spine o AP Pelvis 4. AMPLE history -Allergies, Medications, Past medical history, Last meals, Events surrounding injury 5. Secondary survey o Full head-to-toe assessment o Can be delayed until all life-threatening injuries have been dealth with Surgical Equipment Scalpel Blades 10 - General use 11 - Pointed, for arteriotomy 15 - Smaller minor ops 22 - Big mother 23 - Curved Scissors Mayo's: curved dissecting scissors McIndoe Pott's (for arteriotomy) Stitch cutter Clips Mosquito Dunhill Roberts (big ones) Spencer-Wells Forceps DeBakey's McIndoe's Babcock's Retractors West self-retaining Travers Norfolk & Norwich - Big self-retaining Langenbeck Devers retractor Senn retractor (cat's paw) Hohmann's Breast & Endocrine Adrenalectomy Indications Phaeochromocytoma Adrenal carcinoma / adenoma Non functioning incidentaloma > 4cm in diameters (risk of malignancy) Failure of medical therapy Considerations (if for phaeochromocytoma) - Alpha blockade (doxazosin) - Beta blockade (atenolol) Right adrenalectomy 1. Supine + GA + Prepare/drape 2. Transverse supra-umbilical incision made with upward convexity 3. Access adrenal gland o Mobilise right colic flexure, retract downwards, retract liver upwards o o Incise posterior peritoneum above level of upper pole of right kidney Expose IVC, right adrenal gland 4. Dissect / remove adrenal gland o Separate from kidney and perinephric fat / fascia o Dissect off IVC o ligate vessels o Dissect out 5. Ensure haemostasis 6. Close wound in layers Post-operative considerations 30mg po hydrocortisone/day Fludrocortisone 0.1mg/day Breast disorders Development / anatomy Modified sweat gland 2-6 ICS; sternum to AAL 2/3 on pectoralis major, 1/3 on serratus anterior (with axillary tail of spence) Condensation of fibrous tissue forms suspensory ligament of cooper (supportive framework) Blood supply 1. Axillary artery (2nd part, lateral thoracic arter) 2. Internal thoracic artery 3. Intercostal arteries Nerve supply 1. Intercostal nerves T4-T6 Lymph drainage Axillary nodes - 75% 1. Level 1: lateral to pectoralis minor (14 nodes) 2. Level 2: posterior to pectoralis minor (5 nodes) 3. Level 3: Medial to pectoralis minor (2-3 nodes) Internal mammary - 25% [Anatomy of axilla] Congenital / Developmental disroders Athelia / Polytheli: absence / many nipples Amastia: Absence of breast Polymastia: accessory breast Amazia: Absent of breast with nipple present = hypoplasia of breast (90% associated absent/hypoplastic pectoral muscles; ~Poland syndrome) Gynaecomastia Abnormal breast enlargement 1. Female 2. Male o o Physiological: neonatal, pubertal hormone imbalance Pathological: hypogonadism, neoplasms, drugs - cimetidine, spironalactone, ketoconazole, digitalis, oestrogens Aberrations of normal breast development and involution (ANDI) Tumour Fibroadenoma Pathology Features Aberation of development; Well circumscribed Management FNA/Biopsy Mammography / Phylloides Tumour Cystic disease Sclerosing leions Epithelial hyperplasia 15-25 years Develops from single lobule of breast (rather than single cell) Hormone dependance (lactating during pregnancy, involuting in peri-menopausal period) smooth firm lump May be multiple/bilat eral FNA / Biopsy Rx: Complete excision - risk of recurrence Discreet, smooth lump, may be fluctuant (like all cysts) Aspirate fluid Mammography if > 35years Rx: Excision biopsy Radial scars present via screening Potential underlying breast cancer Mammography + excision biopsy breast lump FNA / NCB Rx: Excision biopsy + screening (increased risk of breast cancer) Arise from peristromal tissue 40-50 years More common in African countries Common 35-55 years Macrocysts ~7% women in West Unknown cause Aberration of involution sclerosing adenosis, papillomatosis, duct adenoma Epithelial cell increase in terminal duct lobular unit Common premenopausal women If atypia plus hyperplasia increased risk of breast cancer Atypical ductal or lobular cells x4-5 greater risk of breast cancer ultrasonography Rx: Reassure / remove if large >2cm on request Breast pain / inflammatory lesions Pathology Features Treatment Mastalgi Cyclical Mastaliga a Young women (Any age up to menopause) 3-7 days pre menstrual cycle Improves at menstruation Usually lateral part of breast affected Non-Cyclical Mastalgia Older women (45+) Breast Lactating abscess Mastitis neonatorum - first few weeks of life Infected enlarged breast bud Caused by s.aureus / e.coli Non-Lactating 1. Peri-areolar o Complication of periductal mastitis o More common than lactating breast abscess o 35yrs 2. Peripheral o Ass: DM, RA, Steroids, trauma 3. Periductal mastitis o Bacterial / cigarette smoking / AI basis Complications of Abscess 1. Duct ectasia: dilatation without inflammation Nipple discharg Breast pain Retraction / inversion Weight loss Supportive bra Evening primrose oil NSAIDs Supporting bra Weight loss Rx: Antibiotics / I&D Antibiotics Aspiration I&DS 2. Duct fistula: - Benign Neoplasms Duct papilloma Common Single / multiple Soft lobulated radiolucent lesion Lipoma Usually small, symptomless Bloody discharge if duct involvement Mammography, ductography Rx: Microdochectomy Nipple discharge 1. 2. 3. 4. White = Milk: lactating breast (physiological / prolactinoma) Yellow = Exudate: abscess Green = Cellular debris: duct ectasia Red = Blood: ductal papilloma or carcinoma Determine whether single or multiduct (not usually pathological except in hormone producing endocrine tumours) Mangement 1. 2. 3. 4. Haemo-stix Cytology Mammography / USS Ductography / ductoscopy (washings can be taken for cytology) Breast Cancer: Aetiology & Clinical features Risk factors: OESTROGEN EXPOSURE 1. 2. 3. 4. Age Early menarche, late menopause, nulliparity Diet / obesity (fat turned into oestrogens/phyto-oestrogens) Drugs: OCP, HRT 5. Smoking 6. Family history + Genetics: BrCa1 (17q), BrCa2(13q) Linear increase with age Clinical features 1. From the lesion o Painless breast lump +/- lymph node involvment (I-III; relative to pec. minor) o Hard lump with poorly defined margins o Skin tethering or fixation to underlying structures o Pain / skin ulceration "peau d'orange" - due to involvement of suspensory ligaments of cooper o Nipple discharge / retraction 2. Systemic features o Weight loss o Ascities 3. Features of spread o Bone pain / pathological fractures 4. Paraneoplastic manifestations Diagnosis 1. History (including risk factors) 2. Examination - "Triple assessment" 3. Investigations: o Blood tests: Tumour markers Ca 15-3 (mucin marker) o Imaging: Mammography, Ultrasound (if young pair of titties) 4. Tissue diagnosis o FNA / NCB - 95% pre-operative diagnostic sensitivity FNA Cytology NCB Histology H1 C1 Normal Inadequate H2 C2 - Benign Benign C3 H3 Equivocal Equivocal C4 H4 Suspicious Suspicous C5 H5 Malignant Malignant o Excision biopsy Pathology 1. Epithelial cell origin 1. Non-invasive DCIS - cured by total mastectomy LCIS 2. Invasive Ductal carcinoma: 80-90% (NB Paget's disease of nipple = Ductal carcinoma involving epidermis; starts at nipple with some evidence of destruction) Lobular carcinoma: 1-10% Mucinous 5% Medullary 1-5% Metaplastic 2. Connective tissue origin Prognostic indicators 1. 2. 3. 4. 5. Node positive = <20% survival High Grade (1-well, 3-poor) Size Vascular invasion Oestrogen receptor: based on H (histochemical score) out of 300 o H Score > 50: Receptor positive o H Score < 50: Receptor negative Nottingham Prognostic Index (NPI) NPI = Size (in cm) x 0.2 + Grade (1 - 3) + Stage (Lymph node) NPI < 3.4 - excellent: 15y 90% survival NPI > 5.4 - poor: 15 8% survival Grading Bloom & Richardson grading system Based on tubule formation, nuclear pleomorphism ("many different forms"), and mitotic activity 1. Grade 1: Well differentiated 2. Grade 2 3. Grade 3: Poorly differentiated Tissue Staging TNM system T - Tumour N - Node MMetastasis 0 Subclinical No nodes No mets 1 <2cm Ipsilateral axillary (mobile) Distant mets 2 2-5 Ipsilateral axillary (fixed) 3 >5 Ipsilateral mammary 4 Any size with (a) chest wall or (b) skin extension Manchester system / Columbia system TNM Manchester - T1 - N0N1 Columbia Stage 1 o o Confined to breast < 5cm With or without skin involvement Stage A Stage 2 T2N1b o o Confined to breast <5cm Nodes involved but not fixed Stage B Stage 3 T3-T4 N2-N3 o o Locally advanced disease >5cm Affects underlying muscle/overlying skin or fixed lymph nodes Stage C Stage 4 M1 Stage D o Distant metastatic disease (lung, liver, brain, bone) Managment 1. Diagnose o Triple assessment: high positive predicitive value and prevents erros in diagnosis 2. Stage disease 3. Good cosmesis 1. Surgery o o o o WLE / Quadranetectomy / Segementectomy Remove tumour + adequate resection margins (>5mm margins) Adequate skin flaps for cover Breast reconstruction: pedicled flaps, free flaps (DIEP) 2. Axilla o Level II (up to medial border of pec minor) clearance accepted as best balance between adequate staging and morbidity o Sentinel node technique - finds first draining node (technetium + blue dye); contra-indicated in pregnancy [NB also has use in melanoma and penile cancer] o Morbidity: haematoma, wound infection, seroma, lymphoedema, intercostobrachial neuralgia, injury to thoracodorsal nerve, long thoracic nerve injury, axillary vein injury, brachial plexus injury, post-op frozen shoulder 3. Hormonal therapy o 1st Line: Tamoxifen (Selective oEstrogen Receptor Modulator (SERM)) reduce circulating oestradiol o 2nd Line: Aromatase inhibitors (Anastrazole[Arimadex], fromenstane, aminogluthethimide) - block oestrogen via aromatase pathway o LHRH antagonists (Goserelinp [Zoladex] - prevents oestrogen production by ovaries o 3rd Line: Progesterone 4. Chemotherapy 1. Antimetabolites (impair production of DNA):5-FU, Methotrexate 2. Vinca alkaloids (inhibit microtubule formation): Vincristine, vinblastine 3. Alkylating agents (bind to and disrupt DNA): Cyclophosphamide 4. Platinum-based agents Radiotherapy Follow up 1. Early detection + treatment of recurrence o Local recurrence: - single spot, o Regional recurrence: axilla, brachial plexus, supraclavicular nodes o Distant mets 2. Early detection of metastatic disease 3. Psychiatric morbidity Excision of a breast lump Indications Benign lump Possibly malignant lump Procedure 1. 2. 3. 4. 5. 6. Fix lump between finger and thumb Incision made circumferentially if close to nipple, radially if placed distally Grasp lump with forceps and retract out of wound Expose interior of cavity and diathermy bleeding points Obliterate cavity +/- suction drain Close skin with subcuticular stitch Complications Haematoma Distortion of breast architecture Recurrence of lump Fine Needle Aspiration (FNA) Procedure 1. 2. 3. 4. 5. 6. 7. 8. 9. Explain to patient Sterile field 21G needle, syring + 2ml of air (for explusion of contents) Prepare slides Fix breast lump Pass needle through lesion in several directions maintaining suction Release suction, withdraw needle Air used to blow out cells to slides Label slides and send to your friendly histopathologist Microdochectomy Indications Persistent blood-stained discharge from single duct opening on nipple Procedure 1. GA/LA 2. Identify duct o Squeeze breast until drop of discharge seen 3. Cannulate duct o Use lacrimal probe and secure in place 4. Incise skin along line of probe, encircling duct orifice 5. Dissect skin of areola away from breast tissue (for 1cm) 6. Excise breast segment 7. Secure haemostasis with diathermy + approximate breast tissue with interrupted absorbable sutures. Modified Patey Mastectomy Indications Cytologically proven breast carcinoma Preparation GA DVT prophylaxis Supine position + arm on armboard Procedure 1. Mark boundaries for skin incision o At least 3cm from tumour o Anatomical markers - medially: sternum / laterally: lat dorsi / superiorly: 2cm below clavicle / inferiorly: 1-2cm below infra-mammary fold o ?? Excision should include nipple/areolar complex 2. Dissect lump o Incise skin o Develop flaps (use clips/retractors) in plane corresponding to Scarpa's fascia between the subcutaneous fat and mammry fat - aim for thickness of 34mm medially increasing to 6-8mm laterally o Approaching clavicle superiorly, dissect more deeply to pectoral fascia o Raise inferior flap 3. Dissect axilla: - obtains regional control of disease, establishes prognostic information o peel breast laterally until border of lat dorsi o retract pec major to expose pec minor o divide pec minor (close to point of insertion onto coracoid process) o Identify Long thoracic nerve of Bell, thoracodorsal nerve (and intercostobrachial nerve) o Ligate all venous tributaries from axillary vein 4. Remove lump + axillary contents en-masse o Place stitch on most proximal node for pathological orientation 5. Place one suction drain on breast bed + one in axilla 6. Washout with antiseptic 7. Close + Can be combined with flap reconstruction TRAM - transverse rectus abdominis DIEP Complications Bleeding / infected haematoma Buttonholing of skin flaps Nerve injury - LT nerve (serratus anterior - winged scapula); thoracodorsal nerve (lat dorsi) Thyroid disease Thyroid disease spectrum 1. Arteries: o superior thyroid (external carotid) o inferior thyroid (thyrocervical trunk of subclavian) o Accessory thyroid ima 2. Veins: o Superior o Middle o Inferior 3. Nerves: o Recurrent laryngeal (cricoarytenoids - supply vocal cords) o Superior laryngeal [Thyroid hormone physiology & disease spectrum] Thyroid Neoplasms 1. 2. 3. 4. 5. Papillary 70% - younger population, good prognosis, TSH-dependent Follicular 20% Anaplastic 5% - older population Medullary 5% - from parafollicular C-cells Lymphoma - rare Management of thyroid disease 1. History o o o o Thyroid symptoms Medications Previous radiation exposure Familial history 2. Examination o Neck o General examination: signs of thyroid disease - hands, eyes, cardiovascular system 3. Investigations o TSH, T4, thyroid autoantibody screen o USS: sensitive for detecting thyroid nodules, used to guide FNA o FNAC: Most reliable test for thyroid nodules o Radio-isotope scans no longer routinely used ("hot" nodules were benign and "cold" nodules were not) Hemithyroidectomy procedure 1. GA + Supine + head-up tilt of 15' 2. Head rests on ring, sandbag in interscapular position 3. Dissect down to thyroid o Transverse collar incision approximately 2finger breadths above suprasternal notch o Divide skin and platysma o Extend superior flap to thyroid, inferior flap to suprasternal notch o Expose strap muscles o Divide cervical fascia in midline and retract strap muscles laterally 4. Dead with surrounding structures o Ligate and divide middle and inferior thyroid veins o Inferior thyroid artery identified and ligated in continuity as inferiorly as possible o Identify recurrent laryngeal nerve in its groove between trachea and oesophagus (and protect) o Identify parathyroid glands and preserve 5. Remove thyroid o Superior vascular pedicle is ligated and divided o thyroid lobe mobilised and excised o oversew isthmus with absorbable sutures 6. Close o Haemostasis completed o Suction drain placed in subfascial space o Fascia closed in midline with absorbable sutures o Skin + platysma closed o Skin closed with non-absorbable subcuticular suture Complications 1. Haematoma - may cause respiratory embarassment 2. Recurrent laryngeal nerve palsy 1% o Single nerve paresis results in hoarse voice o Both nerves leads to paralysis 3. Superior laryngeal nerve palsy 4. Hypothyroidism 5. Hypoparathyroidism - causes hypocalcaemia - check calcium level post-operatively 6. Scarring Post-op: radio-iodine scan can demonstrate remnants of thyroid tissue or distant metastases Remaining tissue can be ablated Serial thyroglobulin measurement 6-12 month intervals (acts as marker for tumour recurrence) Wide local excision & axillary clearance Indications Tumours < 4cm Mammogram excluding multifocal disease Axillary clearance 1. Level I: Lateral to pectoralis minor 2. Level II: Up to medial border of pectoralis minor 3. Level III: Beyond medial border of pectoralis minor Procedure 1. 2. 3. 4. 5. 6. 7. Curvilinear incision (including previous biopsy sites) Incise around segment and deepen incision (maintain >1cm tumour clearance) Separate breast tissue from pectoralis fascia Remove tumour (insert silk sutures to identify parts of tumour) Haemostasis + suction drains Obliterate cavity Close skin Axillary clearance 1. 2. 3. 4. 5. 6. 7. 8. Incise skin + elevate flaps superiorly/inferiorly Identify lateral border of pectoralis major and anterior border of latissimus dorsi Identify and divide pectoralis minor. Preserve thoracodorsal (lat dorsi) and long thoracic nerve of bell (to serratus anterior). Preserve intercostobrachial nerve (axillary sensation) Upper limit of dissection is axillary vein Dissect contents away from vital structures, remove en masse. Drain axilla with suction drain Wash wound with antiseptic betadine + close subcutaneous tissues. Complications Nerve injury (esp intercostobrachial nerve) Secondary lymphoedema Haematoma (avoided by diathermy + drains) Wire-guided localisation biopsy Indications Radiological microcalcification suspicious of DCIS Impalpable lesion Workup Radiologically guided localisation (USS/X-ray) Barbed wire inserted Procedure 1. Incise skin transversely over wire 2. Follow wire to substance of breast 3. Excise around wire with good margin + frozen section to identify that whole of lesion has been taken 4. When adequate excision confirmed, ensure adequate haemostasis 5. Obliterate cavity 6. Close with subcuticular stitches Cardiothoracic Surgery Aortic dissection Classification 1. Stanford o Type A: ascending aorta only o Type B: descending aorta with or without ascending aorta 2. BeBakey o Type I: ascending aorta + descending o Type II: confined to ascending aorta o Type III: confined to descening aorta, beyond origin of subclavian artery Pathology Myxoid degeneration - loss of elastic fibres and replacement of musculo-elastic tissue with proteoglycan-rich matrix Cystic medial necrosis: may be associated with injury or occlusion of vasa vasorum Intimal tear - dissection propagates along plane that runs between inner 2/3 and outer 1/3 of media Predisposing factors 1. 2. 3. 4. 5. Hypertension - leads to increased shearing forces across intima Traumatic injury to aorta Iatrogenic - cardiac catheterisation, aortic cannulation, AV replacement Pregnancy Inherited defects o o o Marfan's - 15q fibrillin defect Ehlers-Danlos - procollagen formation Pseudoxanthoma elasticum - fragmentation of elastic fibres in media Effects of dissection 1. Propagation o Aortic ring - acute aortic regurgitation o Coronary arteries - Angina / MI o Carotid arteries - stroke o Abdominal aorta - gut ischaemia (if mesenteric vessels involved) o Renal artery - ARF o Intercostal / lumbar vessels - spinal cord ischaemia (loss of supply from arteria radicularis magna - great spinal artery of Adamkewicz) 2. Rupture o Pericardium - tamponade o Pleura - haemothorax 3. Compression o Trachea / oesophagus / SVC 4. Double-barrelled lumen (if re-enters lumen through another intimal tear) Clinical features Shock New Murmur Tamponade Asymmetrical pulses Neurological signs - stroke, cord features Investigations ECG: MI / exclude cardiac differentials CXR: 80% widened mediastinum Angiography: Gold standard - visualisation of ventricular valve function, permits assessment of coronary anatomy CT/MRI: 85-90% sensitivity + specificity TOE: >95%; can be used at bedside Management 1. 2. 3. 4. Resuscitate: fluids, maintain cardiac index (CO/BSA) and renal function Bloods Central line: monitor filling pressures Pharmacological o Labetalol - control ejection fraction and arterial pressure o Sodium nitroprusside (can cause reflex tachycardia) 5. Transfer to cardiothoracic unit o o Type A: Replacement of diseased segment of aorta with interpositional graft and re-implantation of coronary arteries if root involved +/- valve replacement Type B: Conservative managment (surgery confers no additional benefit) Cardiopulmonary bypass Cardiopulmonary Bypass 1. 1. Expose great vessels 2. 2. Purse string inserted into ascending aorta (adventitia) + aortic perfusion cannula + connect to bypass circuit o Impracticalities: Aortic root surgery, dissection, severe adhesions - fem-fem bypass can be employed 3. Purse string inserted into Rt atrium by appendage Cardiopulmonary bypass machine takes over circulation + ventilation o Pumped from venous reservoir o Oxygenated in membrane oxygenator (gas exchange across silicone membrane) o Heat exchanger o Filtered: remove particulate emboli o Infused via roller pump (achieves even arterial pressure) Post cardiopulmonary bypass Air excluded from cardiac chambers Restore beat is VF present Epicardial wires for post-op bradycardia/heart block Warm Correct acidosis Correct K When BP acceptable, CPB discontinued + Protamine to reverse effects of heparinisation +/- inotropic support +/- intra-aortic balloon pump Myocardial protection 1. 1. Cardioplegic arrest o Topical cooling + cardioplegic (intentional + temporary cessation of cardiac activity) solution o K+ - containing (arrests heart in diastole by membrane depolarisation) o Cold isotonic crystalloid - reduce metabolic rate o Safe cardiac arrest can be maintained for 2hours 2. Intermittent cross-clamp fibrillation o Induce VF (by electrical voltage) o Cross clamp aorta to render heart ischaemic o Allow perfusion (10-20minutes) by intermittently releasing cross-clamped aorta + electrical cardioversion 3. 3. Total circulatory arrest Complications 1. Access o Infection, pulmonary injury, vascular injury 2. Bypass o o Embolism Bleeding disorder (from heparin) 3. Stress/consequences o Tamponade o Emboli - heart: infarction, brain: stroke, gut: ischaemia Chest drains / Tube Thoracostomy Indications Diagnostic: effusion/blood/pus/lymph Therapeutic: drainage of air/fluid (effusion, blood, pus, lymph) Sizes French gauge (20-32F) = external circumference in millimetres 32F used to prevent clot obstruction of tube Technique 1. Adequately prepared / consented 2. Clinical examination + inspection of CXR: confirm side of insertion 3. Position: (1) supine + arm abducted (2) seated leaning forwards + arms outstretched o Skin cleaned w iodine + draped o 5th ICS / 3rd ICS (Anterior) anterior to MAL by palpation of ribs o LA wheal w 1-2% lignocaine + deep infiltration 4. Insert over rib (avoids neurovascular bundle) o 1.5-2cm incision w scalpel (11 blade) 5. Blunt dissection down to pleura using finger + Roberts forceps à finger sweep to clear adhesions + widen tract 6. Drain guided into intercostal space o Aim apically for air / basally for fluid o Secure with drain stitch + apply dressing/tape 7. Attach to underwater seal +/- suction o Drain bottle below level of patient at all times o Minimise resistance: chest tube should be sufficiently wide o End of drainage tube should not be > 5cm below level of water otherwise resistance encountered will prevent air from escaping chest tube 8. Check CXR: accurate position + re-expansion 9. Analgesia Complications Laceration/puncture intrathoracic/abdominal organs (prevented by finger sweep) Infection Damage to intercostal nerve/artery/vein Subcutaneous emphysema Indications for removal Full lung expansion Drain no longer functioning (air/fluid ceased to drain) No longer swinging (can flush drain - remove obstruction with normal saline) Procedure in removal X-ray after 1. Off suction 2. With tube clamped Remove drain in inspiration Coronary Artery Bypass Graft Surgery (CABG) Operative Technique Surgical Anatomy of the Heart Access to heart Harvesting of Long saphenous vein chest opened via sternotomy + LIMA dissected from chest wall Heart cannulated via ascending aorta + right atrium before cardiopulmonary Longitudinal arteriotomy made beyond narrowing of coronary vessel + distal Venous Grafts: o Long saphenous vein (10 year patency rate 50-60%) o short saphenous vein o cephalic vein Arterial Grafts: o Left internal mammary artery (internal thoracic artery) - conduit of choice for LAD (10 year patency rate 90%) o Radial artery -NB Allen's test to ascertain collateral circulation Pre-operative workup ECG Echocardiography Carotid duplex study Pulmonary function tests Angiography FBC, U+Es, LFTs, Clotting, G+S Antibiotics: Cefuroxime 1.5g +/- Vancomycin Post-op management Prophylactic chest drain External cardiac pacing Complications Bleeding 3-5% of patients. May develop tamponade / hypotension Medical management first May require emergency re-sternotomy Management of Bleeding: Check coagulation profile Fibrinogen Platelets Specific treatments: 1. Protamine sulphate o Directly binds to heparin and inactivates 2. Trasylol / Aprotin 2MU iv o (Bovine) serine protease inhibitor (specifically trypsin, chymotrypsin, plasmin, kallikrein) o Effect on Kallikrein: inhibits formation of factor XIIa and plasmin - slows down fibrinolysis 3. Tranexamic acid o Inhibits activation of plasminogen into plasmin Arrythmias Common to develop ST / AF Management of Tachyarrythmias 1. Correct potassium >4.5mmol/l - Potassium chloride 2. Correct magnesium: 8/10-20mmol MgSO4 IV Atrial Flutter 1. 2. 3. 4. Vagal manoeuvres Adenosine 6mg/12mg/12mg B-blocker rate control DC synchronised cardioversion Atrial Fibrillation 1. B-blocker iv / Digoxin 500mg iv/12' 2. Amiodarone 300mg iv/1' + 900mg iv/23' 3. DC synchronised cardioversion Management of Bradyarrythmias 1. Atropine 500mcg iv bolus (repeat to maximum of 3mg) 2. Adrenaline 2-10mcg/min 3. Cardiac pacing Flail chest Flail chest injury 3 or more ribs fractured at 2 or more places on the rib shaft - results in area with loss of continuity with rest of rib cage and has potential to move independently during respiratory cycle Implications of flail chest 1. High mechanism injury (one rib = 150mls blood loss) o Possible underlying pulmonary contusion 2. Can lead to respiratory embarassement o Exhibit paradoxical movement during respiratory cycle - moves inwards on inspiration o Pain from fracture leads to reduced TV o Type II (mechanical) failure can result 3. Late complications: pneumonia, septicaemia, atelectasis o Reduced ventilation increases risk of retained secretions and sequlae Managment According to ATLS principles 1. Manage flail chest o Humified oxygen o Analgesia - paracetamol / NSAIDS / Opiates / intercostal block / thoracic epidural (up to T4) + splinting of injury o Intubation / mechanical ventilation - if worsening fatigue and RR 2. Identify underlying injury 3. Prevention of secondary complications Sucking Chest wound Occurs when wall defect 2/3 size of trachea diameter Air enters chest through hole rather than trachea Can lead to tension pneumo Rx: 3-sided dressing acting as flutter valve Lung surgery Requirements Double lumen ETT (allows selective collapse of lung) Pneumonectomy Lobectomy 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Right/left posterio-lateral thoracotomy Spread ribs Get anaesthetist to collapse one side of lungs Enter pleural cavity Define anatomy (dissect through fissues) to hilum Dissect vein (superior), artery (inferior) and bronchus (posterior) Ligate all three Divide lung Check for air leak (fill cavity with water and ask anaesthetis to blow on lung) Insert apical chest drain Close Mediastinitis Inflammation of the mediastium - ie. the cavity within the thorax between the pleural cavities. Causes Direct mediastinal access o Sternotomy / cardiothoracic surgery o Mediastinoscopy o Penetrating trauma Per trachea o Intubation / failed percutaneous tracheostomy o Bronchoscopy Per oesophagus o Boerhaave's o Iatrogenic oesophageal perforation Direct extension o Infection from lung, pleura Organisms: anaerobic oral flora, respiratory flora - or multi-resistant strains if cardiothoracic surgery Features (of general inflammation) Pyrexia Rigors Surgical emphysema Hamman's sign (crunching sound in systole) Management Bloods: Inflammatory markers, FBC, CRP Imaging: CXR (enlarged mediastinum) + CT Treatment: Surgical drainage/debridement + Antibiotics Pericardectomy Indications Operative considerations Should release both ventricles at the same time - premature release of the right ventricle leads to increase blood flow to the lungs (with unreleased left ventriculat outflow) Result is increased pooling of blood in the lungs - pulmonary oedema! Pneumothorax Types 1. Simple: air in pleural space 2. Tension: one-way valve effect 3. Open: Sucking chest wound Causes 1. Spontaneous: rupture of blebs - asthmatics, skinny lanky 2. Trauma 3. Iatrogenic Recognition 1. Conscious o Tachycardia, tachypnoea, decreased sats o Tracheal deviation, hyper-resonance o Surgical emphysema 2. Unconcious / ventilated o Sudden hypoxia o Sudden increase in ventilatory pressures o Sudden hypotension or rising CVP o New arrythmia Management 1. 2. 3. 4. Early recognition (esp tension) 100% O2 Tension - needle decompression (2ICS) Chest drain Pleurodesis Performed endoscopically (VATS - video assisted thoracoscopic surgery) Chemical Physical - by abrasive pads: used for younger patients as chemical pleurodesis carries theoretical risk of increasing malignancy Indications for Thoracotomy in Haemopneumothorax (Persistent bleeding - usually from chest wall ~80%) Loss of >1500mls immediately into drain Loss of >200mls/hr for 2-4 hours Requirement for persistent blood transfusion Surgical Access to the Heart Median Sternotomy 1. Incision from suprasternal notch to lower end of xiphisternum o Sternum covered by fat + pectoral muscles o Superiorly: Suprasternal ligament from SCJ to other o Inferiorly: rectus abdominis fibres 2. Sternum divided + retracted o Superiorly:Thymus o Inferiorly: Pericardium 3. Thymus divided in midline o Highly vascular o Care because lies anterior to innominate/brachiocephalic vein 4. Pleura dissected from pericardium laterally 5. Pericardium opened +/- cannulation (with full heparisation) Closure of Sternotomy Ensure haemostasis Insert pairs of stainless steel wires (usually 6) through sternal body Inspect for bleeding from internal thoracic vein/artery Twist wires Cross wires Suture fascia to pectoral fibres Close skin with subcuticular stitch Thoracotomy 1. Median Sternotomy Posterio-lateral thoracotomy Access to hilum and pleural cavity 1. 2. 3. 4. 5. 6. Curved incision 2cm below scapula Dissect through skin, fat Divide latissimus dorsi fibres Spread off serratus anterior Divide through intercostal muscles (at level of 5th rib - count from second rib) Enter pleural cavity Closure 1. 2. 3. 4. 5. Appose ribs Sew deep fascia onto intercostal muscles Close serratus anterior layer Sew latissimus dorsi Close skin Emergency Thoracotomy Indications Penetrating injury with cardiac arrest Massive thoracic bleeding Procedure 1. 2. 3. 4. 5. Positioned obliquely with ipsilateral hip and shoulder supported on sandbags Submammary incision made starting near midline and extending into axilla Pass through all layers to enter chest in 5th ICS Ribs separated with spreader Pericardium can be opened anteriorly and parallel to phrenic nerve - decompress tamponade Valve surgery Heart valves maintain pressure gradients between cardiac chambers to ensure unidirectional flow. Valve leaflets supported by chordae tendinae + papillary muscles Valve Cusps Description Aortic 3 Semilunar leaflets Attached at annulus Coronary arteries arise from (1) Left = Left posterior sinus (2) Right = Anterior sinus Mitral 2 Anterior/Posterior cusps Pulmonary 3 Tricuspid 3 Stenosis Aortic Mitral Rheumatic heart disease Calcification Congenital Rheumatic heart disease Calcification of valve/chordae Congenital Regurgitation Rheumatic heart disease Endocarditis Congenital Inflammatory - SLE, Ank spond Dilation of aortic root - Marfan's, dissection Systemic disease - UC, syphilis Rheumatic heart disease Valve prolapse LV dilation Ischaemia / papillary muscle disruption Bacterial endocarditis Technique of Aortic Valve replacement Transverse incision across valve Dissect out / remove diseased valve Insert + secure new valve Close aorta (full thickness continous sutures) Apply tissue glue Add pro-coagulant covering Indications for Mitral Valve replacement Severe symptoms (as classified by NYHA functional classification) Progressive increase in LV volume leading to ventricular impairment (Ejection fraction, end-diastolic volume) Endocarditis Prosthetic Valves Type Mechanical Biological Example 1. Ball & Cage o Starr-Edwards o Barium-impregnated silastic ball retained in cage 2. Tilting valve disc o Bjork-Shiley o Single disc opens and closes with blood flow 3. Bileaflet o St Jude Medical valve o Two disc occluders Complications Structural Valve failure Prosthetic valve endocarditis Paravalvular leak Related to endocarditis episode Leaflet degeneration Autografts Harvest patient's own pulmonary valve into aortic position (Ross procedure) Excellent haemodynamic function (but technically demanding) Autologous pericardial valves Homografts/Allografts - Removed from Thrombosis / Thromboembolism Mechanical 2.5 - 3.5 Tissue 1.5 - 2.5 cadavers Antibiotic sterilised Short supply Technically difficult Xenografts - Prepared from animal tissue Porcine-valve Pericardium mounted Appendicitis / Appendicectomy Appendicitis Inflammation of the vermiform appendix Most cases are idiopathic. 1. Lumen: mucosal appendicitis o Foreign material o Faeces o Worms: strongyloides, ascaris lumbricoides o Parasites: oesophagostomiasis 2. Wall: transmural appendicitis o Infection: Viral (CMV, adenovirus), bacterial (TB, yersinia), amoebae, schistosomes o Inflammation: UC, crohn's, pseudomembranous colitis o Ischaemia: ischaemic colitis, congenital stricture, iatrogeni 3. Outside wall: Serosal appendicitis o Ovaries - salpingitis/oophritis o Endometriosis o Diverticular disease Presentation 1. Clinical findings o Periumbilical colicky pain (visceral peritoeneum) o Migrates to RIF (parietal peritoneum) 2. Specific features o McBurney's point pain o Rosving's sign: Deep palpation of RIF causes pain in RIF - confused visceral peritoneum (also positive in bladder, uterus, descending colon, fallopian tubes, ovaries inflammation) o Psoas sign: flexed right hip where appendix is lying over psoas muscle o Rectal tenderness: from pelvic appendix Indications Emergency - acute appendicitis Elective - "interval" appendiciectomy after intial conservative treatment (of appendix mass) Open Procedure 1. GA + Antibiotics + supine position 2. Access appendix o McBurney's incision (90' to imarginary line) / Lanz incision (cosmetically better) / High up in RUQ in children o Skin, fat (campers fascia), scarpa's fascia o Incise external oblique aponeurosis in line of fibres, expose internal oblique (if too medial will see rectus sheath) o Split internal oblique fibres transversely, enlarge defect o Pick up peritoneum between 2 clips, incise with scalpel - turbid fluid indicates appendicitis (send this off to microbiology) o Identify caecum (has teniae) and deliver into wound [enlarge incision if difficult/impossible to deliver] 3. Remove appendix o Hold appendix with 2 tissue forceps (Babcocks) o Divide mesoappendix (hold up to light to see blood vessels) o Apply purse string (buries appendix stump) with 2/O o Crush appendix base (facilitates secure knot tying) and ligate proximally with O suture. o Remove appendix, bury stump by tightening purse string o Suck out free fluid, wash out peritoneal cavity 4. Close wound in layers Laproscopic Appendicectomy Especially young female patients - where diagnosis uncertain, imaging has failed to exclude gynaecological cause. 1. GA / Possible conversion to open 2. Establish pneumoperitoneum o Trendelburg position o Infraumbilical incision o Open peritoneum under direct vision o Insert trochar o Insufflate gas 3. Inspect appendix o o o o 5mm port RIF under direct vision 5mm port LIF Grasp caecum and move towards spleen Aspirate free fluid (send for cytology) 4. Remove appendix o Grasp appendix with forceps o Dissect from mesentry using hook diathermy introduced through right port o Ligate at base using pre-tied Vicryl ligature + second distal to first one o Divide and remove under direct vision 5. Peritoneal lavage 6. Close fascial defects with absorbable sutures + steri-strips to skin If appendix normal - look for other causes: Gynae: ovaries, fallopian tubes, ectopic pregnancy Gut: meckel's, sigmoid diverticulitis Paediatric: look for mesenteric adenitis Insert drain if abscess present Complications Increased risk of right hernia Bowel obstruction Features 1. Pain: colicky o Epigastrium / umbilical = small bowel o Suprapubic = large bowel 2. Vomiting o Consequences: dehydration, metabolic alkalosis/respiratory acidosis hypoxia o More distal lesions, later the vomiting o Contents: pyloric = watery; high = bilious; low = faeculent 3. Distension o Depends on level of obstruction 4. Constipation 5. Pyrexia, septicaemia Causes 1. Luminal o 2. Mural Intussuception o o Malignancy Inflammatory bowel disease 3. Extra-mural o Hernia o Adhesions Frequency of causes 1. 2. 3. 4. 5. Adhesions - 60% Herniae - 15% Malignancy - 6% IBD Ischaemic bowel Pathophysiology 1. Bowel dilatation proximal to obstruction o Results in gas / fluid accumulation with bowel wall and lumen (proximally) o Impairs resorption 2. Mucosal oedema impairs venous / arterial flow o Bowel becomes strangulated 3. Ischaemia leads to haemorrhagic infarction o Further dilation leads to bowel perforation 4. Bacterial translocation leads to sepsis Principles of Management 1. History o o o Previous operations Abdominal diseases Previous obstruction 2. Examination o Previous scars o Presence of hernia o Bowel sounds: tinkling / hyperactive 3. Investigations o Plain AXR - distended bowel loops (and level of obstruction) - small plicae circulares; large haustrae o Plain CXR - exclude free air o FBC: WCC, anaemia o Electrolytes o ABG: Lactate / acidosis 4. Resuscitation o IV crystalloid o Correct acid-base o NGT o Catherise o Analgesia Indications for surgery 1. Absolute o Peritonitis o Perforation o Incarcerated hernia 2. Relative o Palpable mass o Virgin abdomen o Failure of conservative treatment Surgical options in Large bowel disease 1. One stage (medially optimised patient) o resection of tumour/lesion, decompression of bowe, lavage with primary anastamosis 2. Two stage (unwell patients who may be optimised) o Hartmann's procedure with resection of tumour o Later reversal of colostomy 3. Three stage (sick patients/moribund/advanced disease) o Emergency defunctioning colostomy (until patient fit for further operation) o resection of tumour and anastamosis in 2nd operation o Final closure Cholecystectomy Indications Symptomatic gallstones: biliary colic, pancreatitis Cholecystitis Empyema of gallbladder Mucocoele of gallbladder Laproscopic Procedure 1. Consent + permission to convert to open 5-10% cases 2. Establish pneumoperitoneum (open method) - 1cm incision under umbilicus, introduce trochar, insufflate air, then laproscope 3. Insert ports 10mm epigastrium; 5mm MCL; 5mm AAL 4. Identify Calot's triangle (Liver, cystic duct, hepatic duct) - contains cystic artery 5. Dissect cystic duct, artery and GB 6. Apply x3 clips on either side of structures, divide leaving 2 clips 7. Divide gallbladder from hepatic bed using diathermy hook to maintain haemostasis 8. Remove gallbadder (collect in endobag to prevent leakage) 9. Release pneumoperitoneum, close wounds Open Procedure 1. Upper right transver incision (over lateral border or rectus muscle) 2. Skin, campers fat, scarpas fascia, anterior rectus sheath, rectus, posterior rectus sheath, transversalis fasicia, extraperitoneal fat, peritoneum Complications 1. 2. 3. 4. 5. Bile duct injury Haemorrhage - slipping of clips Retained stone Biliary stricture Duodenal injury Colorectal cancer Management 1. History o o o o Characteristics of PR bleeding Change bowel habit Weight loss Family history: HNPCC, p53, APC 2. Examination o DRE: 90% palpable o Inspect glove for blood or mucous o Abdomen for masses 3. Investigations o Proctoscopy: visualisation, confirmation and biopsy of any lesion o Barium enema - identify suspicious lesions 4. Staging o Local spread: Endoluminal USS, CT, MRI o Metastatic spread: CXR, USS, CT Chest / Abdomen o 2cm adequate / 5cm preferred o Ensure tension free anastamosis by adequate mobilisation o Consider protecting anastasmosis by proximal defunctioning loop ileostomy Right Hemicolectomy + Primary anastamosis 1. Enter peritoneum o Midline incision / transverse incision (less painful, slimmer patients) 2. Mobilise caecum and terminal ileum o dividing lateral peritoneum clockwise and upwards o Dissect off right colon o Identify and protect the gonadal vessels, right ureter and duodenum 3. Divide bowel o Transilluminate the mesentry; ligate vessels close to origin (as close as possible really) o Place non-crushing clamps on transverse colon and ileum and divide bowel between crushing clamps 4. Form end to side anastamosis (along taeniae) o Close distal end of colon (by hand) or stapling device o Approximate ileum with colon and commence posterior wall by inserting seromuscular (Lembert suture) o Open colon along taeniae and insert full thickness absorbable suture o Continue to midline anteriorly and tie off sutures 5. Close mesenteric defects (prevents herniaetion) 6. Close wound (mass closure etc) Left Hemicolectomy + Primary anastamosis 1. Enter peritoneum 2. Mobilise colon o Divide along white line of "Toldt" o Push sigmoid mesentry medially o Identify and protect gonadal vessels and left ureter as it crosses pelvic brim 3. Divide bowel o Transilluminate mesentery and identify and ligate vessels close to origin o Distally ligate vessels at bowel wall o Place non-crushing clamps across rectum and proximal bowel o Protect wound edges from contamination using abdominal swabs o Excise colon 4. Form anastamosis o Single-layer technique o Stapled gun 5. Close mesenteric defect 6. Washout + close Hartmann's operation / End colostomy Indications Obstructing lesion in sigmoid colon Perforated lesion in sigmoid colon Volvulus of sigmoid colon Pre-op: marking by stoma nurse 1. Enter peritoneum o Midline incision 2. Mobilise bowel o o o 3. 4. 5. 6. Divide along white line (avascular plane) Sweep sigmoid off mesentry Identify and protect gonadal vessels and left ureter Divide bowel o Transilluminate mesentry, identify and ligate vessels o Place non-crushing clamps across distal and proximal bowel o Excise diseased segment Close distal colon with two layers of continous sutures o Hitch bowel to presacral fascia making it easier for reversa Formation of stoma o Bring out proximal colon o Circular skin incision 2cm in diameter and deepen to rectus sheath (palpate inferior epigastric vessels to avoid damage at this stage) o Make cruciate incision into sheat, bluntly dissect through muscle into peritoneal cavity o Place clamp through stoma site and capture proximal colon: manipulate bowel through abdominal wall o Approximate skin and bowel edge with interrupted sutures at regular intervals (x6-8 deep: external oblique aponeurosis + superficial: skin) o Good practice to pass colon through peritoneum at point lateral to intended stoma site as this creates a tunnel which should reduce the incidence of stomal herniation Washout peritoneal cavity with tetracycline throughout procedure (very high risk of wound infection) Reversal of Hartmann's Only attempt once patient has fully recovered + stoma has matured (3-6 months) ~60% are reversed due to persisting morbidity in the patient Anterior Resection + defunctioning ileostomy Indications Carcinoma of mid-rectum 1. 2. 3. 4. 5. GA + Lloyd-Davies position + Catheter Enter peritoneum Mobilise bowel Colorectal anastamosis Defunctioning ileostomy Abdomino-Perineal resection Indications Carcinoma of lower 1/3 of rectum Anal carcinoma Pre-op: irreversible colostomy 1. GA + Lloyd-Davis position + catheter 2. Abdominal component o Sigmoid mobilised o Protect other structures (ureter, gonadal vessels) o Rectum mobilised - identify and protect pre-sacral plexus o Divide fascia of Denonvilliers anteriorly (protect seminal vesicles) 3. Perineal component o Elliptical incision from coccyx passing lateral to anal verge and finishing at perineal body o Deepen to mesorectum to meet abdominal access o Divide posterior edge of levator ani 4. Rectum freed and delivered through perineal wound 5. Form stoma from remaining colon 6. Close abdomen 7. Close perineum Complications Reactionary haemorrhage Infection - wound, pelvic abscess Renal tract injury Sexual dysfunction and impotence Complications of colostomy - retraction, prolapse, herniation, stenosis, ulceration, ischaemia/necrosis Compartment syndrome / Fasciotomy Compartment syndrome Raised pressure in osteofascial compartment Elevation of pressure prevents tissue capillary perfusion: causes muscle and nerve damage Features: severe pain out of proportion to injury aggravate by muscle stretch and parasthesia Causes: trauma, reperfusion, burns, exercise Complications of missed compartment: muscle necrosis, myoglobinuria, renal failure, infection, amputation, foot drop from peroneal nerve palsy, volkmann's ischaemic contracture Management 1. History 2. Examination 3. Investigations o Classic symptoms need no further investigations o Unclear diagnosis: compartment pressures ?30mmHg over diastolic 4. Treatment o Double incision fasciotomy o Daily dressings of wound o Prophylactic antibiotics o Re-examine in 24-48hours to debride necrotic tissue and cover wounds Tibial Compartment fasciotomy Compartments of the lower leg Anterior compartment Tibialis anterior Extensor digitorum longus Extensior hallucis longus Lateral compartment Peroneus Longus Peroneus brevis Posterior compartment Tom-Dick-Harry Tibialis posterior Flexor digitorum Flexor hallucus Plantaris Soleus Gastrocnemiu s Indication Extensive soft tissue injury of lower leg Compartment syndrome Measurement of compartment pressures 1. Prepare / sterilise skin 2. Infiltrate LA 3. Insert catheter into compartment, inject small amount of saline into cannula to fill dead space 4. Fill manometer tubing with saline + connect to catheter + pressure monitor (ensure no bubbles/other dampening influence) 10-30mmHg < diastolic: Impending ischaemia >30mmHg < diastolic: Impending/established compartment syndrome - Need urgent fasciotomy Procedure 1. Full length longitudinal anterolateral skin incision 2cm lateral to crest of mid-tibia from level of tibial tuberosity to just proximal to ankle o Anterior compartment: Incise fascia covering tibialis anterior + extend proximally/distally o Identify and protect superifical peroneal nerve (lies deep to intermuscular septum) o Lateral compartment: undermine skin to get to lateral compartment (avoid superficial peroneal nerve) 2. Single longitudinal 1-2cm posterio-medial incision just medial to posteriomedial border of tibia o Identify and retract long saphenous vein o Incise deep fascia proximally to level of tibial tuberosity and distally to 5cm proximal to medial malleolus o Should be anterior to posterior tibial artery to avoid damage to perforating vessels used for later cutaneous flaps Closure of fasciotomy 1. Wound should be left open + VAC dressing 2. Suture skin 3-5 days later (when swelling subsided) +/- split skin grafts 3. Keep leg elevated Complications Disruption of venous muscle pump Poor healing Excision of lymph node Indications Confirm diagnosis of lymphadenopathy Procedure 1. 2. 3. 4. 5. 6. Incision should be able to convert to a radical procedure should this be necessary Deepen incision Identify lymph node Dissect node (+ vascular pedicle) Diathermy / tie pedicle, excise node Ensure haemostasis, close wound Excision of sebaceous cyst Indications Cosmetic Recurrent infections, sebaceous horn Procedure 1. 2. 3. 4. LA Elliptical incision over cyst (include punctum) Grasp cyst and free from base Close with interrupted non-absorbable sutures Excision of toenail Indications Ingrowing toenail Onychogryphosis Nail infections Procedure (Zadik's operation) 1. 2. 3. 4. 5. LA ring block Apply rubber tourniquet Incise nail bed (transversely) + elevate flaps Remove nail plate with heavy scissors Cut across nail bed down to bone and continue to nail fold, remove nail bed (get all of germinal matrix) 6. Suture skin flaps at side Exicision of Skin lesions Indications Malignancy Cosmesis Procedure 1. Use small scalpel blade (10/15) 2. Make elliptical incision around lesion (along langer's lines to ensure good cosmesis)# o BCC/SCC: excise whole of lesion o Malignant melanoma: 1cm margin for 1mm / 2cm margin for 2mm / 3cm margin for 3mm 3. Incise under lesion to remove 4. Close skin with undyed subcutaneous non-absorbable suture Femoral Hernia repair Indications All femoral hernias (high risk of strangulation) Landmarks: inguinal ligament (anteriorly), pectineal ligament (posteriorly), lacunar ligament (medially), femoral vein Procedure: Low / crural approach If any doubt as to bowel viability, laparotomy recommended 1. Dissect down to hernia o Groin incision directly over inguinal ligament o Identify, dissect superficial fascia down to sac o Expose neck of hernia 2. Open hernia, inspect, reduce hernial contents o If necrotic bowel, resect and perform laparotomy 3. Close hernie defect o Carefully retract femoral vein o close defect (suture inguinal ligament to pectineal ligament - use J-shaped needle) 4. Close subcutaneous tissue with interrupted sutures + skin with subcuticular High inguinal approach Extraperitoneal approach Useful if unsure hernia is inguinal or femoral 1. Dissect down to hernia o Supra inguinal incision (Pfannenstiel, midline) o Skin, blunt dissect superficial tissues to gain access to hernial sac o Open rectus sheath + retract rectus o Open up pre-peritoneal space with blunt dissection o Continue process down towards inguinal ligament + identify hernia 2. Identify and reduce hernia o If sac empty, reduce back to abdomen: pull above, push below o If bowel present, stretch femoral ring (with haemostat), transfix sac + excise tissue o If irreducible, open peritoneum from above + inspect contents +/- bowel resection 3. Close femoral canal with interrupted non-absorbable sutures between pectineal + inguinal ligament Intestinal Stenosis of Garre Strangulated hernia causes mucosal ulcer Intestinal mucosa more vulnerable to ischaemia rather than overlying seromuscular layer - heals by fibrosis Annular stenotic stricture of small bowel Causes small bowel obstruction Gut surgery Preparation 1. 2. 3. 4. 5. 6. Adequate bowel prep - fluid restriction 48 hours prior + picolax 24 hours prior DVT prophylaxis IV antibiotic prophylaxis - metronidazole / cefotaxime Catherise NGT Seen by stoma nurse / "stomatherapist" - marks stoma in 3 positions of standing, sitting and lying 7. Consent Principle 1. Perform full laparotomy - inspect everything 2. Assess *tumour for resectability + clearance margins (2cm acceptable; 5cm desired) 3. If Metastases found, should continue surgery as best "palliative" measure - resection margins can be reduced Complications 1. 2. 3. 4. Surgery Stoma "General" Metabolic / nutritional consequences Haemarrhoidectomy Haemorrhoids 1. Cushions of dilated vascular tissue at anal verge 2. Anal cushions are required for full continence 3. Straining causes the cushions to slide down and become engorged - results in symptomatic haemarrhoids Classification 1. First degre: small non-prolapsing 2. Second degree : prolapsing but reduce spontaneously 3. Third degre: prolapse that cannot be reduced Treatment options 1. Asymptomatic o No treatment required 2. First degree o Stool-bulking agents o Injection sclerotherapy 3. Second degree o Banding 4. Third degree o Haemarrhoidectomy Haemarrhoidectomy procedure 1. 2. 3. 4. 5. 6. 7. 8. 9. Prepared + consented + phosphate enema Lithotomy position + GA Skin or anus/perineum prepared + Parkes proctoscope passed PR Gently draw haemorrhoid towards surgeon and then make V-shaped incision in anal skin at base of haemorrhoid Raise haemorrhoid towards lumen away from sphincter fibres + transfixed and ligated with vicryl suture Divide haemorrhoid 5mm distal to ligation and removed Repeat for other haemorrhoids (3,7,11 position) Pack anal canal with gauze or spone to keep mucocutaneous bridges flat against the internal sphincter (prevents an anal stricture forming) Apply perineal pad and firm T-bandage Post-op care daily bulking agents glycerin suppositories for faecal retnetion Analgesia 30 minutes before bowel movements and change of dressings External wounds managed with twice daily baths, irrigation and dressings 4 week outpatient review complications 1. 2. 3. 4. 5. 6. 7. Bleeding Constipation Anal stenosis Faecal incontinence due to damage of sphincter mechanism Anal fissure Recurrence Perianal fistula Incisional Hernia repair Risk factors for developing incisional herniae 1. Surgical o o Careless suturing Inappropriate material 2. Local o o Haematoma Infection 3. Patient o o o o Malnutrition Obesity Jaundice Immunosuppression Procedure for repair 1. Optimise patient pre-operatively (repair often fails) 2. GA + supine 3. Dissect down to hernia o Incision made over hernia o Hernia sac dissected out o Incision deepened around margins og hernia until healthy aponeurosis identified 4. Reduce hernia o Sac opened o Contents returned to peritoneal cavity 5. Close defect o if < 4cm can be closed with interrupted nylon o If large: close with tension-free Prolene mesh repair sutured to anterior rectus sheath with interrupted absorable sutures at 2cm intervals 6. Finish Inguinal hernia repair Indications Symptomatic herniae Irreducible herniae Patent processus vaginalis Landmarks: Inguinal Ligament (Gimbernaut): Formed from reflection of the aponeurosis of the external oblique muscle Runs from the Anterior Superial Iliac Spine (ASIS) to the pubic tubercle Deep Ring: Midpoint of inguinal ligament Superficial Ring: Above pubic tubercle Ilioinguinal nerve Position: Prone Procedure 1. 2. 3. 4. 5. 6. 7. 8. Incise skin 2cm above inguinal ligament from deep ring to superficial ring Pass through superficial fascia/fat (Camper's) Pass through deep fascia (Scarpa's) Expose extern oblique apneurosis Enter inguinal canal, identify and protect ilioinguinal nerve Identify and protect the spermatic cord Dissect hernia sac (anterior + superior to cord) Open sac, inspect contents (may contain ovary in female), reduce hernia, close defect o If bowel present, check viability (wrap in warm saline-soaked abdominal pack) o If necrotic, must be resected 9. Reinforce wall with mesh o In children, repair is usually satisfactory, and don't need mes o Tension-free repair: Liechtenstein (lateralises cord) o Bassini repair o Shouldice repair 10. Ensure haemostasis, ensure testis in scrotum. Laparoscopy Advantages Smaller incisions, reduced tissue trauma Disadvantages Absent tactile feedback Difficult haemorrhage control Reduced post-op pain Decreased incidence of wound complications Decreased physiological insult to patient Reduced inpatient stay Improved cosmesis Learning curve May need consersion to open Contraindications (things that really need open procedures being done) 1. General o o Coagulopathy Shock 2. Specific o o Peritonitis Obstruction Essential components 1. 2. 3. 4. Establish pneumoperitoneum Insertion of trocar Inpection of cavity Removal of trocar and closure of wounds Pneumoperitoneum 1. Trendelenburg position (head down) - position bowel away from pelvis 2. 1-2cm infraumbilical incision (transverse or vertical), deepen down to rectus sheath o Closed laparoscopy - Veress needle 1. Hold up abdominal wall, insert Veress needle perpendicular to skin until "give", then point needle towards pelvis at 45' 2. Confirm satisfactory insertion - saline drop test or aspiration o Open laparoscopy - Hassan cannula 1. Pick up / incise rectus sheath. Place sutures on each side of linea alba 2. Incise peritoneum and enter peritoneal cavity under direct vision 3. Insert finger, sweep away adhesions 4. Insert port + stay sutures 3. CO2 insufflation (aim pressure 0-5mmHg) 4. Percuss abdomen to ensure symmetrical abdominal distension 5. Maintain pressures of 13-15mmHg, volume of gas 4-5L Insertion of trochar 1. Introduce cannula using corkscrew technique (aim towards pelvis) - check position by releasing gas tap/vavle (hearing air) 2. Attach camera 3. (Bleeding can be controlled by inserting a foley catheter to achieve compression) Insert other ports under direct vision Position of ports 1. Infra-umbilical pneumoperitoneum (veress/hassan) 2. Epigastric trochar / camera 3. Epigastric cannula Finishing 1. 2. 3. 4. 5. Remove under direct vision Check port site for haemostasis Umbilical/epigastric ports should be closed formally Skin closure by tapes/sutures + wound infiltration with bupivacaine for analgesia Common complications 1. Rectus sheath insufflation, gives high pressures - stop 2. Misting of equipment (if not adequately pre-warmed) 3. Blood on lens can be wiped on omentum Laparotomy Midline incision Closure of Midline Laparotomy 1. Divide skin in midline, divide Jenkin's rule: decreases the risk of subcutaneous tissue dehiscence 2. Divide linea alba for full length of skin incision Mass closure technique (include 3. Pick up peritoneum between clips, peritoneum + rectus sheath in confirm no bowel adherent, nick closure) peritoneum between clips Continous suture (0 or 1 loop PDS) on 4. Insert finger beneath wound to a blunt needle ensure no underlying adhesions, then Suture should be FOUR times the divide peritoneum with scissors for full lenght of incision 5. Ensure no adherent viscera, avoid bladder in lower midline lenght of the incision and bites should be taken 1cm from the wound edge at 1cm intervals Exploratory laparotomy Oesophageal hiatus > stomach > duodenum Palpate liver, GB, Rt kidney Right colon > caecum Pelvis Sigmoid > ascending colon, spleen, left kidney Transverse colon, pancreas, aorta Small bowel, (from ligament of Treitz) to jejunum, ileum and caecum Paramedian incision 1. Incise skin 4cm from midline (over rectus) 2. Incise anterior rectus sheath 3. Divide sheath from muscle at points of intersections 4. Reflect rectus laterally to expose posterior sheath 5. Incise posterior sheath for full length of wound and then divide peritoneum Subcostal incision 1. Keep parallel + 2cm from costal margin 2. Divide anterior rectus sheath 3. Pass long forceps underneath meuscle to emerge in midline 4. Pull swab back under muscle to protect underlying structures from cutting diathermy (superior epigastric artery br. int thoracic) as muscle is being divided 5. Small incision made into peritoneum, allows protection of viscera as transversus abdominis muscle is divided Closure of Paramedian incision Close peritoneum using over and over technique Anterior rectus sheath closed as for midline incision (applying Jenkins' rule) Management of Abdominal wound dehiscence Surgical emergency with 30-40% mortality Resuscitation with IV fluids Protection abdominal contents with sterile soaked towels (saline/betadine) Immediate closure in theatre with deep tension sutures ITU backup for post-op management Oesophagus disorders Hiatus Hernia Acquired form of diaphragmatic hernia Types: 1. Sliding: GOJ slides through the oesophageal opening of the diaphragm 2. Rolling / paraoesophageal: GOJ remains in position but area of stomachad peritoneum rolls up alongside oesophagus into thorax Gastro-Oesophageal Reflux Disease Management 1. History o Burning pain 2. Examination 3. Investigations o Upper GI endoscopy + biopsy to detect oesophagitis and Barrett's oesophagus o 24h pH manometry 4. Treatment o Lifestyle changes: weight loss, avoid alcohol and smoking, avoid large meals at night o Medical: antacids, H2 antagonists, PPIs o Surgery in: severe persistent regurgitation, severe reflux symptoms, patient choice Nissen Fundoplication Other options - Belsey Mark IV: fundoplication through thoracotomy - Hill gastropexy (securing cardia to pre-aortic fascia 1. Laparscopic / Midline incision 2. GA + elevate head end of table 3. Create pneumoperitoneum / access oesophagus o Divide lesser omentum o Retract right lobe of liver o Dissect oesophageal hiatus 4. Repair crural defect o Identify crura o Dissect 3-4cm of abdominal oesophagus and mobilise o Retract oesophagus to right o Repair crural defect with interrupted non-absorbable sutures 5. Free fundus and greater curvature o Divide short gastric vessels o Freed fundus passed behind and then to the left of the oesophagus 6. Fundoplicate o Fundal wrap held with 3 interrupted non-absorbable sutures, taking bites of both fundal folds and the oesophagus 7. Finish o Irrigate operative field + ensure haemostasis o Close fascial defects Paraumbilical hernia repair Indications Procedure (Mayo repair) 1. GA + Supine 2. Dissect down to hernia sac o curved infraumbilical incisio o Dissect subcutaneous tissue, dissect from rectus sheath o identify hernia sac 3. Excise hernia o open sac, reduce contents (usually omentum) o Ligate sac and excise to level of fascia 4. Close defect o Grab edges of fascia with Allis clamps o Superior fold of fascia overlapped on top of inferior fold (double breasted manner) using non-absorbable interrupted mattress sutures 5. Close o Close in layers Peptic ulcers [Peptic ulcer disease] Perforated peptic ulcer Indications Acute duodenal perforation - prevents sepsis and shit like that Procedure: Oversew 1. 2. 3. 4. GA + NGT + Antibiotics + DVT prophylaxis + Urinary catheter + supine position Upper midline laparotomy Identify stomach + work distally to duodenum Identify perforation o Usually found on anterior surface of 1st part of duodenum o If not present there - look on posterior surface of stomach - if perforated stomach ulcer is found biospy it cause it's probably going to be a fat cancer, innit? If ulcer is large and friable, will need partial gastrectomy (as omentum just isn't man enough to do it) 5. Close perforation o Insert x3 absorbable sutures through duodenum on each side of perforation o Find mobile piece of omentum that can be mobilised into position o Lay across perforation and loosely tie stures over the top of omentum (do not tie tightly - may necrose omentum) 6. Wash out peritoneal cavity (remove food and shit) 7. Close as for laparotomy Laproscopic procedure 1. Pneumoperitoneum via open method (1cm infra-umbilical incision), enter peritoneum under direct vision 2. Introduce trochar, insufflate CO2, introduce laproscope 3. 11mm port under xiphisternum 4. 5mm port in MCL R hypochondrium 5. 5mm port AAL R hypochondrium 6. Irrigate / suction peritoneal cavity 7. Repair as above 8. Close port sites Post-op care 1. Proton-pump inhibitor 2. H.pylori eradication - (urease breath test C13): Metronidazole + clarithromycin + PPI 3. Oral fluids once flatus passed Bleeding peptic ulcer: Under-running Indications Bleeding from an ulcer that has failed to respond to conservative managment (prevents bleeding to death and shit like that) - including endoscopy + injection of sclerosants or adrenaline Haemorrhage requiring more than 6 units blood/24hours Haemorrhage unresponsive to intensive resuscitation High risk of re-bleeding: (1) spurting/oozing vessel on endoscopy (2) visible vessel at base of ulcer on endoscopy (3) fresh or adherent clot on endoscopy Procedure 1. 2. 3. 4. 5. 6. 7. 8. 9. GA + NGT + Antibiotics + DVT prophylaxis + Urinary catheter + Supine position Upper midline laparotomy Identify stomach (distended with blood) with grey small bowel (cause of blood) Insert two stay sutures on duodenum and open duodenum longitudinally (will be closed transversely - prevents stenosis) Identify point of bleeding o Pass sucker into duodenam lumen to identify bleeding point (usually posterior wall) o Stuff swab into pylorus to prevent blood from being expelled from stomach o If cannot find blood in duodenum, look in the stomach - gastic ulcer, erosions, varices Under-run gastroduodenal artery as it passess behind duodenum using 1/O absorbable suture o Take good bites (can miss artery otherwise) o Don't go too deep as will hit CBD o Tie sutures firmly Remove swabs, evacuate blood from stomach Depending on degree of ulcer-related duodenal scarring proceed to o pyloroplasty (close duodenum transversely with interrupted sutures) o gastroenterostomy Close wound Perianal abscess / fistula / fissure in ano / Pilonidal sinus Peri-anal abscess Usually painful in anal region Swinging pyrexia Treatment is drainage with appropriate antibiotics Classification of Perianal abscess 1. Peri-anal 60%- suppuration of anal gland (can also occur as result of thrombosed external pile) 2. Ischio-rectal 30% (IR fossa communicates with opposite side via the post-sphincteric space; involvement of contralateral fossa not uncommon) 3. Sub-mucous 5%; usually resolves (result of injection of haemarrhoids) 4. Pelvi-rectal 5% (supralevator) - usually secondary to appendicitis, salpingitis, diverticulitis, parametritis Procedure 1. Cruciate incision over abscess + excise skin over abscess (de-roof) 2. (Take microbiological cultures - if enteroccocci, high incidence of fistula; up to 40% risk) 3. As soon as infection subsided, wound explored under anaesthesia + careful search for fistulous opening 4. If no fistula found, cavity should be lightly packed with gauze + apply T-bandage Fistula in Ano Track lined by granulation tissue that connects deeply in anal canal/rectum and superficially on the skin around the anus Usually results from an anorectal abscess which bursts spontaneously Associated with underlying diseases - eg TB, Crohns Gives recurrent discharge Goodsall's rule: fistulae with external opening anterior to anus have a direct (straight) opening. Fistulae with posterior opening have curved tracks. Classification of Perianal fistula 1. Simple or complex - associated or not with abscess cavity 2. High or Low - above or below anorectal (puborectalis) ring o Subcutaneous o Submucous o Low anal o High anal o Pelvirectal 3. Park's Classification - by origin of fistula track o o o o Intersphincteric (between internal/external sphincters) 70% Transphincteric (across external sphincters) 25% Suprasphincteric (over sphincters) Extrasphincteric (above and through levator ani) Procedure 1. Decide whether fistula is low or high 2. Proctoscopy - reveals internal opening 3. Endoluminal ultrasonography / MRI to map complex fistulae (may have multiple openings) o Low: Lay open 1. Prep cleaning enema 2. Lithotomy position 3. Identify the fistula: protoscopy + retrograde probe + dilute methylene blue dye 4. Track opened along director and bleeding controlled 5. Trim edges of track o High: (risk of incontinence if laid open) - staged procedure + protective diverting colostomy to prevent septic complications and to shorten healing time between procedures 1. Treat the cause: TB, Crohns 2. Insertion of a seton 1. (a heavy ligature of silk, nylon, silastic or linen) used when internal opening near anorectal ring 2. acts as wick/drain to allow acute inflammatory reaction around track to subside 3. Can be serially tightened to cut through sphincter (allows healing) to maintain sphincter integrity 4. Acts to drain fistula 3. + Covering colostomy [Levator ani = Pubo-rectalis + Pubo-coccygeus + Ilio-coccygeus] Fissure in Ano Longitudinal tear in anal canal (90% posterior midline) ?Constipation / large stools primary cause or result of them Combination of local trauma to epithelium + ischaemia preventing adequate healing Also seen in STDs and IBD Symptoms: pain, bleeding, itching, pruritis ani Treatment 1. Conservative o High fibre diet, stool bulking o Topical LA o Topical GTN (controls anal spasm) 2. Surgical o Lateral sphincterotomy: divide distal internal sphincter to dentate line with incision lateral and away from fissure (complications - transient flatus incontinence) Ramstedt's pyloromyotomy Indications Pyloric stenosis Procedure 1. GA 2. Access pylorus o 3-4cm transverse incision made in right upper quadrant over palpable pyloric tumour o advanced through rectus sheath, sheath, into peritoneum o Deliver greater curvature of stomach into woun 3. Split pyloric muscles o Rotate pylorus o Incise visceral peritoneum over lenght of tumour o Using blunt forceps, longitudinal and circular muscles are split down to submucosa 4. Finish o Identify any inadvertant leaks (and repair with omental patch) o Close abdominal wound with interrupted absorbable sutures o Close skin with subcuticular sutures Peritonitis Causes 1. Upper GI o Perforated peptic ulcer 2. Lower GI o Appendicitis o Perforation sigmoid diverticulitis o Perforation 3. Hepatobiliary o Perforation of Gallbladder o Acute pancreatitis 4. Gynaecological o Rupture ectopic pregancy Organisms: Bacteroides, E.coli, clostridium, pseudomonas, klebsiella Peritonism 1. 2. 3. 4. 5. 6. Guarding / rebound suggests strangulation or perforation Continous pain (rather than colic) Tachycardia Dehydration WCC Pyrexia Rectal prolapse Predisposition 1. Anatomy - continence maintained by 120' pubo-rectalis sling o Children; direct downward course of rectum (undeveloped sacral curve) o Maldevelopment of pelvis o Female - torn perineum (pregnancy) o Weak pelvic floor 2. Constipation / straining o Diarrhoea (in children) o Straining o Haemarrhoids Classification Pathology Complete Full thickness prolapse of rectum through anus Weakness of levator ani Starts at weak anterior wall Protrudes 1015cm in lenght Contains pouch of peritoneum anteriorly (which can sometimes contain small intestine) Incomplete/partial Mucous membrane + Treatment 1. Perineal approach o Delorme's operation - rectal mucosa removed circumferentially from prolapsed rectum; sutured in "concertina" fashion to reduce prolapse and create ring of muscle within anal canal narrows orifice and prevents recurrence 2. Abdominal approach o Wells operation - rectum fixed firmly to sacrum by inserting sheet of polypropelene mesh between them o Suture rectopexy - 4-6 interrupted sutures used to fix rectum to sacrum 1. Digital repositioning (mucosal) submucosa of rectum protrude outside of anus 2. Phenol submucous injections 3. Excision of prolapsed mucosa Concealed Intersusseption of upper anus into rectum 1. Laxatives / stool bulking agents 2. Dietary modifications Small bowel resection Small bowel resection Indications Ischaemia, infarction, necrosis Tumour Procedure 1. GA + NGT + Antibiotics / Supine position 2. Midline incision 3. Deliver diseased segment into wound o Protect wound edges (with swabs - minimise sepsis) o Apply 2 non-crushing clamps to occlude bowel either side of disease segment 4. Incise peritoneum of mesentery along chosen line for division of vessels (transilluminate, then tie with absorbable sutures) 5. Place crushing clamps at 30' angle to bowel and divide close to clamp - allows better perfusion of anti-mesenteric border o Cut across bowel with knife, remove diseased section o Cover cut ends with antiseptic soaked swabs o If bowel ends do not bleed (usually poor blood supply) - resect until health tissue reached 6. Perform anastamosis (two layers - inner including submucosa + outer lembert stitch) o Posterior wall first: seromuscular continous o Full thickness suture (double ended) o Check anastamosis - if looks dusky; wait, observe 7. Close defect (including mesentry - prevents gut herniation) with interrupted sutrues 8. Close abdominal wal Splenectomy Indications 1. Elective o o o o Haematological disorders Part of radical upper abdominal surgery Splenic tumours (Previously - staging of lymphoma) 2. Emergency o Trauma Preparation 1. 2. 3. 4. 5. 6. GA NGT Antibiotics DVT prophylaxis Supine position Vaccination against streptococcus pneumoniae 6/52 before elective surgery and ASAP post-operatively in emergency splenectomy 7. + Long-term prophylaxis against pneumococcal sepsis (with PenV - 250mg bd) Elective Procedure (remove spleen and look for speniculi) 1. Incision o o o o 2. 3. 4. 5. 6. 7. Left paramedian Midline: for trauma Transverse Left subcostal Divide lienorenal ligament - attaches spleen to kidney o (stand on right of patient) o Pass hand over spleen onto lienorenal ligament o Retract spleen and divide - start from lower end and move towards apex/upper pole using long scissors (obviously!) o Deliver spleen up into wound (sweep away peritoneum with swab on a stick) Detach omentum from lower pole of spleen o Divide left gastroepiploic vessles between artey forceps + ligation with ties Ligate main splenic vessels o Pass fingers around hilum and palpate branches of splenic artery as they pass into spleen; clip + divide branches o Remove artery before the vein (if you don't - blood can enter but not leave and you end up in a bloody mess from an exploded spleen) - removing artery "deflates" the spleen o (Protect tail of pancreas), left colic flexure and diaphragm Detach gastrosplenic ligament Remove spleen + place suction drain in subphrenic space Close abdominal wall in layers Emergency splenectomy (Aim to preserve spleen if possible - prevents post op splenic sepsis) IV access, resuscitate Correct coagulopathy Cross match lots of blood (4+ units) 1. Evacuate clots (manually + suction) 2. Pass hand down to hilum to control bleeding 3. Assess degree of splenic damage o Minor decapsulating injury - managed by application of topical haemostatic agents + wrapping spleen in absorbable mesh o Single laceration: suture (splenorrhapy) o Complete/partial avulsed fragment: partial splenectomy - divide splenic vessels supplying pole in question, resect the fragment and oversew edge with absorbable mattress sutures o Massive irreprable damage: splenectomy 4. Close abdomen Complications of splenectomy 1. General o o o o o Bleeding Atelectasis of lower lobe Ischaemic perforation of greater curvature of stomach Wound infection / subphrenic abscess Damage to organs causing gastric fistula, pancreatitis, pancreatic fistula 2. Specific o o Thromobcythaemia (strokes, clots) + leucocytosis - commence aspirin 300mg daily if platelets >750 Infection from encapsulated organisms Umbilical hernia repair Indication Symptomatic hernia (rare) Procedure 1. 2. 3. 4. 5. 6. Stab incision below umbilicus Develop plane Identify hernia sac Divide sac from skin, open sac, reduce hernia Close defect transversely Close defect with interrupted absorbable sutures Orthopaedic Surgery Anatomy of Walking 1. 2. 3. 4. Heel strike Stance phase Push off Swing Ankle fractures Weber classification Carpal Tunnel syndrome The Carpal Tunnel Attachments of flexor retinaculum (palmaris longus inserts into it; proximal edge is at distal wrist crease) 1. 2. 3. 4. tubercle of Scaphoid ridge of Trapezium Hook of hamate Pisiform Superficial: Ulnar nerve and artery (runs in Guyon's canal) Deep structures: 4FDS, 4FDP, FPL Median nerve (Flexor carpi radialis runs underneath the flexor retinaculum but lies outside the carpal tunnel Causes 1. 2. 3. 4. 5. Idiopathic Pregnancy Obesity Trauma Systemic disease: myxodema, rheumatoid arthritis, acromegaly, diabetes Management 1. History o Risk factors (above) 2. Examination o Tinels tap test positive o Phalen's test 3. Investigations o Nerve conduction studies 4. Surgical decompression Surgical decompression procedure 1. 2. 3. 4. Informed consent, mark correct side LA / Regional / GA Limb exsanguinated + tourniquet, note inflation time Exposure of flexor retinaculum o 3cm incision from distal flexor crease (from line ring finger ------) o expose flexor retinaculum 5. Cut retinaculum o Place MacDonald's elevator underneath retinaculum o Incise longitudinally down to instrument o Median nerve identified (paler in colour, has visible blood vessels called vasa vasorum on surface) o Protect motor branch to thenar muscles / palmar cutaneous branch that provides sensation to skin [by staying medially...] 6. Close skin with interrupted nylon sutures 7. Apply light splint Dislocations Shoulder Elbow Hip Anterior Posterior Knee Femoral Neck fractures Considerations in Hip anatomy 1. Femoral neck anteverted 10-15', angled approximately 125' 2. Coxa valga > 125; Coxa vara <125' Blood supply to Femoral head 1. Nutrient artery (profunda femoris) 2. Artery of ligamentum teres (from obturator artery) 3. Retinacular branches of medial (most important) and lateral circumflex femoral arteries (from profunda) Attachments of femoral capsule Femoral Musculature Movements of the Hip 1. Flexion o o Psoas, iliacus (femoral nerve) Assisted by rectus femoris, sartorius, pectineus 2. Extension o Gluteus maximus [inserts iliotibial tract, into gluteal tuberosity of femur // inferior gluteal nerve] o Hamstrings (semimembranosus, semitendinosis, biceps femoris // tibial nerve) 3. Abduction o Gluteus medius, gluteus minimus (superior gluteal nerve) 4. Adduction o Adductor longus, magnus, brevis (obturator nerve) 5. Internal rotation o Anterior fibres of gluteus medius and minimus (Weakest) 6. External rotation o Gluteus maximus o Obturators o Gemelli o Pyriformis o Quadratus femoris Classification 1. Intracapsular / extracapsular o Intracapsular - Garden: based on AP of hip o 2. 3. 4. 5. Extracapsular - intertrochanteric, pertrochanteric, subtrochanteric Angulation / alignment o Oblique / spiral / transverse Displacement Parts o Comminuted Aetiology: trauma, pathological Complications of fractures 1. From fracture o Avascular necrosis o Non-union o Malunion o Secondary osteoarthritis 2. Damage to surrounding tissues o Bleeding - can loose 1-2litres of blood o Nerve injury 3. Loss of function o DVT / PE o Chest infection o Pressure sores Surgical Treatment options 1. Intracapsular o Aim to preserve femoral head if undisplaced, otherwise remove o Internal fixation - cannulated screws o Replacement of femoral head - hemiarthroplasty 2. Extracapsular o Internal fixation Surgical Approaches to the Hip 1. Lateral approach o Split tensor fascia lata, gluteus medius, gluteus minimus o Detaching greater trochanter [ends up with really bad trendelenburg!] 2. Anterior approach o Passess between gluteus medius and minimus laterally + sartorius medially o Divide reflected head of rectus femoris to expose anterior aspect of hip joint o More room may be provided by detaching gluteii 3. Posterior approach o Angled incision commencing at posterior superior iliac spine to greater trochanter o split gluteus maximus o Detach gluteus medius and minimus from insertion at greater trochanter (or trochanter detached and then re-wired into place) Dynamic Hip screw Fixation Indications: Extracapsular fractures of #NOF, Garden I-II 1. Mark, consent, X-rays, Image intensifer // GA or regional block 2. Traction table, ensure adequate reduction of fracture (traction + internal rotation) 3. Access bone o 15cm incision 2cm from greater trochanter o Split fascia lata o Expose vastus lateralis; retract or split fibres + lift from bone with periosteal elevator 4. Insert internal fixation o o o o o Use 135' guide to place guidewire into femoral neck (aim to get into femoral head, just "inferiorly") - tip of wire should sit in subchondral bone of femoral head Measure lenght of insertion Ream with reamer -5mm of measured Insert screw + 4-hole plate to femoral shaft Confirm position with image intensifier 5. Finish o o o Close fascia lata with absorbable sutures Clips to skin Check X-rays post-operatively Trendelenburg sign / gait Failure of contralateral pelvis to rise when weight is taken on the the affected side Causes: 1. Mechanical o Short femoral neck o Medial migration of femoral head 2. Neuromuscular o Pain o Neuropathy o Myopathy Eponymous fractures Fracture X-ray Mechanism Treatment Bennett's Intra-articular fracture dislocation of base of thumb Monteggia Fracture proximal ulna + dislocation of radial head Galeazzi Fracture distal radius + dislocation of ulna Colles' Fracture distal radius through metaphysis (4cm proximal to articular surface Distal dorsal angulation Ulna styloid Jones' Open fractures Open Fracture Base of 5th MT (insertion of peroneus tertius) Fracture (discontinuity in bone) that is in communication with an epithelial-lined surface Skin GIT Gustilo-Anderson Classification 1. Type I: <1cm (inside-out mechanism) wound 2. Type II: <10cm; no soft tissue loss, no periosteal stripping 3. Type III >10cm or with contamination o IIIa: extensive soft tissue damage / gross contamination irrespective of wound size (farmyard, GSW) o IIIb: soft tissue loss resulting in inadequate amounts of tissue to cover the bone o IIIc: neurovascular injury that requires repair to maintain limb viability Managment 1. ATLS principles o Airway o Breathing o Circulation 2. Assess limb o Assess neurological function of limb o Assess vascular status o Examine wound o Photograph wound prior to dressing it and attach photo to notes 3. Treatment o Cover wound with betadine-soaked dressing o Immobilise limb (in POP, gutter splint, cricket pad splint) +/- manipulation of fracture o Systemic antibiotics with broad-spectrum cover + tetanus prophylaxis o Adequate analgesia o Debride within 6-8 hours; should never be closed primarily; re-examine 48h after; close wound when clean with no evidence of necrotic tissue (primary suture, second intention or flaps Replacement Arthroplasty Features of an ideal replacement arthroplasty 1. Patient o Good range of movement o Complete pain relief 2. Implant o o o o Mechanical stability Low coefficient of friction Low wear Biocompatible 3. Surgery o o Secure fixation to skeleton Revisable in event of component failure Materials used for manufacturing hip joint prostheses Ultra high molecular weight polyethylene Cobalt-chromium-molybdenum alloys Cobalt-chromium alloys Ceramic Surgical Options 1. Total hip replacement 2. Hip resurfacing Complications 1. Infection o Minimised by pre-operative antibiotics o Anti-microbial loaded cememnt o Laminar airflow ventilation in operating room o Thorough scrubbing, use of disposable gowns, changing gloves and good skin preparation o Gentle handling of tissues, adequate haemostasis and good suturing techniques o Optimisation of tissue oxygenation 2. Component failure 3. Dislocation 4. Mechanical loosening o Minimised by dry operative field with adequate haemostasis o Pressurised cement (tighter fit) o Cement restrictors o Lavage systems 5. Aseptic loosening o Microfracture of components o Leads to small particulate matter in joint o Incites inflammatory reaction leading to cysts and loosening 6. Metal sensitivity Plastic Surgery Reconstructive surgery Surgical reconstructive ladder 1. 2. 3. 4. 5. Secondary intention Direct closure Skin graft Flap: local / distant / composite / island flaps Tissue transfer Factors affecting reconstruction 1. Patient o o o o Motivation Health Healing factors - nutrition, vitamins Donor site cost vs benefit 2. Wound / defect o Size and complexity o Anatomy and blood supply/vascularity o Availability of local tissue o Timeframe (ie. open tibias should be closed pretty quickly - innit?) Skin graft Skin transferred from one location to another on same individual Consists of epidermis + variable amounts of dermis "Takes" by acquiring blood supply from health donor bed Independent of blood supply (see skin graft - which needs it's blood supply) Split thickness (STSG) Anatomy Advantages Disadvantages Full thickness (FTSG) Epidermis + variable amount Epidermis + dermis of dermis Preserved skin Harvested using dermatome characteristics (more (Watson & braithwaite collagen content, dermal modifications of Humby knife) vascular plexuses, epithelial or gas-powered dermatomes appendages) Epidermis regenerates from "adnexal elements of skin" - (Skin cannot grow back and donor hair follicles, sebacous glands site needs to be closed primarily) and sweat glands Dermis does not regenerate Large areas can be covered (skin can be put through mesh) Less likely to fail Increased graft contraction at donor site Less contraction at graft site (important for hands and joints - that need movement) Better cosmesis Donor site must be primarily closed Recipient sites Donor site Poor cosmesis Creates second wound at donor site which needs caring for Any large wound Line cavities Resurface mucosal defects Close flap donor sites Resurface muscle flaps More likely to fail because of greater amount of tissue requiring vascularisation Any part of body but in particular areas Easily concealed by clothing Position of easy postoperative care Capable of providing adequate tissue Upper thigh, upper inner arm, scalp, buttock Skin Flap Tissue/tissues transferred from one site to another maintaining a vascular pedicle Classification of skin flaps 1. Site o o Local Distant: Free flap 2. Contents o Tissue capable of transfer 3. Random / axial o Not based on an artery o Based on an artery Renal transplant Indications Types Cadaveric Live-donor Needs HLA matching (as does pancreas) Procedure 1. Curved muscle-splitting incision in contralateral iliac fossa where donor kidney is implanted 2. Donor vein anastamosed to external iliac vein (end to side) 3. Donor artery anastamosed to external iliac artery (end to side) including patch of donor aorta (Carrel patch) 4. Ureter anastamosed to dome of bladder + JJ stent Complications 90-95% survival rate for living related donors 85% for cadaveric donor kidneys at 12 months 75% total graft survival rate at 5 years Liver transplant Indications Procedure 1. Bilateral subcostal incision madef with upward extension to xiphoid process 2. Diseased liver mobilised, IVC clamped and liver removed 3. (Patient on veno-venous bypass - IVC blood directed back to heart via cannula in axillary/internal jugular vein) 4. Portal veins anastamosed end to end 5. Common hepatic arteries anastamosed end to end 6. CBD anastamosed end to end Urology Circumcision Indications 1. Medical o Phimosis (intractable foreskin) - congential adhesions, poor hygeine, balanitis causing foreskin to become thickened and tight o Paraphimosis (trapped foreskin behing the glans) o Recurrent UTIs 2. Non-medical Contraindications Hypospadius Procedure 1. 2. 3. 4. 5. 6. 7. 8. 9. Informed consent, prepared Supine position, GA / LA dorsal penile block Free foreskin from glans with forceps Pull foreskin down over glans; apply straight forceps, divide between forceps to ~5mm of corona Incise laterally, circumferentially towards frenulum Excise Transfix frenulum Two layers of skin brought together with interrupted absorbable sutures Loose vaseline dressing + "sporan" Plastibell (Hollister) technique Complications 1. Immediate o Bleeding / haematoma o Infection o Urine retention o Glans injury o Ischaemia / necrosis of penis 2. Late o Poor cosmesis o Urethrocutaneous fistula o Meatal stenosis o Psychological morbidity Hydrocoele (Canal of Nuck = female equivalent of processus vaginalis, projecting into labium majora) Indications Symptomatic swelling in adults Procedure 1. GA + supine position 2. Access tunica o Stretch scrotal skin o Incise between visible vessels using either knife or cutting diathermy 3. Evacuate fluid o Make small incision in tunica vaginalis o Evacuate the fluid 4. Repair hydrocoele o Jaboulay [tie off sac at apex]: using absorbable sutures, stitch edges of tunica behind cord and subsequently return testis to scrotum o Lords [tie off sac around testis]: using series of interrupted catgut sutures bunching up remaining sac around testis before tying sutures and returning the testis to the scrotum. 5. Close wound with interrupted absorbable sutures Nephrectomy Indications Malignancy [renal cell carcinoma] TCC of ureter requiring nephro-ureterectomy Non-functioning kidney Chronic pyelonephritis Possible approaches 1. Open o o Anterior/Transperitoneal Posterio-lateral/Retroperitoneal 2. Laparoscopic o Transperitoneal o Retroperitoneal Procedure (Right nephrectomy - Anterior/peritoneal approach) 1. CT scan + confirm presence of opposite kidney (otherwise you're in big shit) + mark side + consent 2. GA + supine 3. Kocher's subcostal incision o identify hepatic flexure, duodenum, gonadal vessels o Mobilise colon medially: display perinephric fat 4. Identify kidney (surrounded by paranephric fat), ligate vascular pedicle (prevents dislodging of tumour cells into circulation) o Identify vascular pedicle o Clamp renal artery o Palpate renal vein; ligate and divide o Divide renal artery 5. Mobilise kidney within fascia (Gerota's, surrounds perinephric fat) 6. Divide ureter at accessible point 7. Remove kidney with perinephric fascia intact 8. Place suction drain 9. Close wound in layers Procedure - Posterio-lateral approach 1. Lateral decubitus position + renal bridge on operating table under contralateral loin. 2. Subcostal incision along line of 12th rib: Midline -> posterior axillary line (ie, quite large) 3. Divide layers: skin / lat dorsi / ext obl / int obl / quad lumb / > kidney Laproscopic nephrectomy Dissect out Bring to surface Make skin incision to deliver Complications 1. Early o o o o Wound infection Bleeding Haemorrhage General - DVT, Chest infection, PE 2. Late o Tumour reccurrence Orchidectomy Indications Malignancy Suspected malignancy Orchidectomy Procedure 1. Consent + marked + GA 2. Access testicle via inguinal route (reduced risk of scrotal seeding) o Inguinal incision 2cm above and parallel to medial 2/3 of inguinal ligament o Incise through campers fatty fascia, scarpa's fascia to external oblique o Split external oblique o Free spermatic cord o Apply 2 artery forceps to cord at deep ring (to prevent tumour dissemination) 3. Remove testicle o Divide cord between clamps, tie with non-absorbable sutures o Manipulate testis into inguinal region,free from gaubernaculum by blunt dissection o Remove and send for histological analysis 4. Finish o Close external oblique aponeurosis with absorbable sutures o Close skin with subcuticular suture o Apply scrotal support Prostate Treatment options for prostatic hypertrophy 1. Conservative measures: fluid restriction, reduction caffeine intake 2. Pharmacotherapy: o alpha blockers (alfuzosin, doxzosin) - inhibit smooth muscle contraction o 5-alpha-reductase inhibitor (finasteride) - block conversion of testosterone to DHT which limits size of prostate 3. Surgical intervention o Transurethral resection of the prostate (TURP) o Transurethral incision of prostate for BOO o Open retropubic prostatectomy - prostates > 80g in weight o Transurethral microwave thermotherapy (TUMT) o Transurethral needle ablation of the prostate (TUNA) Indications for prostatic surgery Acute retention (where there is no other cause) / Chronic retention with evidence of renal failure Recurrent haematuria, urinary tract infection Voiding difficulties (hesitancy, poor flow, dribbling, incontinence) instability (frequency, urgency, incontinence) Principles of Prostate surgery Prostatectomy = removal of hyperplastic mass of glandular tissue from surrounding prostatic gland which is compressed into a thin rim around it Approaches: (1) transvesically across bladder (2) retropubically through prostatic capsule (3) transurethrally in TURP, surgeon keeps proximal to verumontanum (colliculus seminalis) in order not to damage the urethral sphincter mechanism Complications 90% success rate 1/6 require re-operation in 6 years Retrograde ejaculation (70%), impotence 20%, erectile dysfunction 5-10% Urethral strictures may be secondary to prolonged catheterisation / infection Incontinence normally up to 3 months Bleeding / infection common TUR syndrome - dilutional hyponatraemia secondary to excessive absorption of irrigation fluid intra-operatively TUR syndrome Pathogenesis: 20ml/minute fluid (isotonic glycine) can be absorbed with 1/3 absorbed into venous system directly (from exposed ends) Risk factors (1) large prostate (2) long operation (3) high pressure irrigation (4) preoperative hyponatraemia Features: (hyponatraemia - swollen brain cells) - confusion, nausea, vomiting Fluid overload - pulmonary oedema Convulsions, coma Symptoms occur generally when Na < 125 mmol/l Up to 50% mortality rate Treatment: support - O2, IV access, oral diuretics, fluid restrict Suprapubic catheter / cystotomy Indications Procedure Testicular Torsion Differential Diagnosis 1. 2. 3. 4. 5. Testicular torsion Torsion of testicular/epididymal appendage Orchitis - mumps / epididymoIncarcerated hernia Hydrocoele Management 1. History 2. Examination 3. Investigations o Scrotal USS: can demonstrate flow of blood in testicular artery. Poor negative predictive value 4. Treatment o When suspected immediate exploration is indicated within 8 hours (after 8 hours, infarcted testis is unlikely to recover Surgical Approach 1. Access scrotum o Skin, dartos, external spermatic fascia, cremasteric fascia, internal spermatic fascia, tunica vaginalis/albuingea, testis ("Some damn Englishman called it the testis") 2. Assess testicle for viability o Release torted testis o Wrap in warm soaked gauze for 10minutes 3. Fix other testicle o Explore contralateral hemiscrotum o Insert 3point fixation for testis to tunica vaginalis o Close with non-absorable sutures 4. If viable, fix; if not viable clamp, ligate and remove Ureter Repair of damaged ureter Direct spatulated ends (plus JJ stent insertion) Implant onto contralateral ureter Boari procedure Varicocoele Varicocoele Acute onset often due to left renal vein compression from renal cell tumour More common on the left Associated with oligospermia Indications 1. Male infertility 2. Scrotal discomfort Treatment options 1. Radiological embolisation 2. Laproscopic division of varicocole from within peritoneal cavity 3. Surgical approach at level of internal ring Surgical Procedure 1. GA + supine 2. Dissect down to testicular vein o Make incision over internal ring parallel to inguinal ligament o Divide external oblique aponeurosis, visualise cord and split spermatic fascia longitudinally to expose testicular veins (from pampiniform plexus) 3. Isolate and divide vein o Separate vein from vas and testicular artery o Ligate and divide with absorbable sutures 4. Close o Repair external oblique aponeurosis with absorbable subcuticular suture o close skin incision with subcuticular non-absorbable suture Vasectomy Indications Male sterilisation (between 28-45) with stable marriage with family of 2+ children Considerations 1. Irreversible (reversal can be attempted in first 5 years but cannot always restore fertility - production of antisperm autoantibodies) 2. Sterilisation not immediate - must provide x2 post op negative counts (at 3 and 4 months), so must continue with barrier contraceptives 3. Recanalisation can occur; unpredictable fertility 1/1000 cases [Contents of spermatic Cord] 3 Nerves: genitofemoral, autonomics, cremasteric [NB ilioinguinal nerve lies on outside] 3 Arteries: Testicular, ductus, cremasteric 3 Other: Vas, pampinoform plexus, lymphatics Procedure 1. 2. 3. 4. 5. 6. 7. 8. LA, supine position Locate and fix vas (grab scrotum and roll between fingers) Infiltrate local anaesthetic 1cm incision into scrotum (Skin, Dartos, ExtSpFasc, Cremaster, IntSpFasc, Tunica, Testis) in direction of vas Dissect out vas with tissue forceps, pass forceps under vas to separate from coverings Divide vas, turn ends backwards and tie ends Bury lower end deep in scrotum to minimise risk of re-joining Close with interrupted stitches Vascular Surgery Amputations Indications Dead: ischaemia (atherosclerosis), gangrene, infection (clostridium), trauma Deadly: tumours of bone (osteosarcoma) / soft tissue (malignant melanoma) Dead weight (excess fingers/toes) Aim is to produce most practical/functional limb for prosthetics - therefore through knee (Gritti-stokes) are not favoured. Through knee - when previous orthopaedic surgery precludes it (ie, long intramedullary femoral nail) Can be performed under GA / LA Double check side of operation Isolate areas of gangrene Generous flaps can be trimmed later If tissue does not bleed (it will not heal properly) - therefore move proximally with amputation Mobilise early to avoid contractures Workup 1. Patient o o o Condition and mobility of patient (AKA more easy to transfer bed-bound patient) Ability for patient to be rehabilitated Psychological counselling 2. Disease o o Pathology / severity of disease Viability of flaps 3. Health-care related o OT / Physiotherapy o Limb fitting / prosthetics (end-bearing amputation may be suitable to allow simple prosthesis) Deciding level of amputation 1. Joint contractures - AKA 2. Severely reduced mobility - AKA affords better transfer, less risk of stump pressure sores 3. Knee OA - AKA 4. Infection 5. Viability of distal limb Types of Amputation 1. Upper limb o Upper arm o Supracondylar (above elbow) o Extraarticulation (thorugh elbow) o Proximal forearm (below elbow) o Distal forearm o Wrist o Metacarpophalangeal o Proximal interphalangeal o Distal interphalangeal 2. Lower limb o Hindquarter o Above knee - equal anterior-posterior flap o Supracondylar o Through knee (Gritti-stokes) o Below knee - long posterior flap o Symes (Tibia/Talus) o Chopart (Talus/Navicular) o Lisfranc (Navicular/Metatarsal) - posterior plantar flap o Transmetatarsal o Ray Above knee amputation One hand's breadth (8-10cm) above upper border or patella: site of femur division Equal length flaps 1. Divide skin + tissues along planned lines 2. Divide soft tissue o Ligate veins using2/O absorbable suture o Deepen incision to bone o Divide quadriceps tendon (to patella) o Divide hamstrings posteriorly o Double-Ligate femoral artery o Apply tension to nerves before ligating so they retract (femoral/sciatic) o Retract thigh muscles 3. Divide Bone o Divide femur, remove lower leg, place clean towel under stsump o Smooth edges of femur using a rasp + bone wax (stop bleeding) 4. Close defect o Bring anterior-posterior muscles together using 1/O interrupted sutures o Place suction drain under muscle layer o Place second layer of sutures in superfical muscles o Suture skin edges with interrupted 2/O sutures 5. Cover stump with gauze + crepe bandage Below knee amputation 14cm from tibial plateau: tibial division / 12cm from tibial plateau: fibular division 2cm proximal Burgess Long posterior myocutaneous gastrocnemius flap (extending down to achilles tendon) Robinson skew flap when posterior flap area compromised 1. Incise along marked lines 2. Divide soft tissue o Divide achilles tendon posteriorly o Divide posterior muscles o Ligate vessels, divide (ie. don't tie them) nerves 3. Divide Bone o Cut fibula obliquely (with Gigli saw) + divide tibia 2cm distal to this o Clear muscle off bone with periosteal elevator 4. Close defects o Oppose muscle flaps + suture o Unite skin edges with 2/O interrupted o Trim edges 5. Apply crepe/cotton-wool bandaging Allows for pressure to be put on stump with smaller risk of dehiscence Complications 1. Early o o o o o Haematoma Wound infection Dehiscence, flap necrosis DVT / PE Phantom limb pain 2. Late o o o o Neuroma Bone spurs Stump ulceration Psychological distress Aneurysm Aneurysm D: Abnormal localised dilation of a blood vessel Classification 1. Congenital / Acquired: o Berry aneurysm (art. circle of Willis) o hypertension 2. True / False: o Full thickness (all three layers) o partial (outpouching of intima) 3. Shape: o Fusiform (entire circumference) o saccular (part of circumference) o dissecting 4. Cause: Atheroma, syphillis, trauma, inflammatory (PAN, Ank Spond), Iatrogenic, ischaemic, congenital, mycotic (following low grade infection), hypertension (Charcot-Bouchard aneurysm) 5. Anatomy: o Ascending aortic aneurysm o Descending - supra-renal (blood supply to gut, spinal cord), infra-renal Complications 1. 2. 3. 4. 5. Thrombosis Embolus Haemorhage Pressure effects - nerve, vertebral column Fistulation Indications for screening 1. All patients with risk factors should have USS at 65 years 2. Small aneurysms (4-5.5cm) should undergo ultrasound surveillance at 6 month intervals Indications for surgery 1. Emergency o Rupture 2. Elective o Symptomatic aneurysm o Rapidly expanding o > 5.5cm Elective mortality is 2-5% Management of Ruptured aneurysm 1. Resuscitation / stabilisation o Large bore cannulae, IV crystalloid, maintain relative hypotension (90-100 systolic) o Urinary catheter - UO o Adequate analgesia o Bloods: FBC, U/Es, LFTs, Amylase, Cross match 8 units of blood + FFP + platelets 2. Contact most senior surgeon / dedicated vascular team + anaesthetist 3. Arrange ITU bed 4. Surgery if unstable, imaging if stable (CT) o Risk of death - 50% survive to hospital, 25% die before operation o Operative complications - limb loss, ischaemic gut, renal failure Aneurysm repair procedure 1. GA, supine, exposed groins (for embolectomy) 2. Access aorta o Long midline incision from xiphisternum to pubis, skirt left of umbilicus o Omentum, large bowel displaced superiorly o Pack small bowel to right o Duodenum displaced o Peritoneum dissected off aorta 3. Give IV heparin 4. Repair aneurysm o Clamp across neck and lower end of aneurysm sac o Incise sac longitudinally o Scoop out thrombus, atheromatous material o End-to-end anastamosis with prosthetic graft using prolene sutures 5. Test repair o Soft clamp applied below sleeve, release upper clamp o Repair lower end of anastamosis 6. Closure o Remove clamps (warn anaesthesist - may get hypotension) o o o o o Ensure haemostasis Close aneurysm sac around repair Close posterior peritoneum (avoids fistulation) Mass closure of wound using looped 0-nylon/PDS Close skin with clips 7. Go to intensive care - watch for complications o Vascular: haemorrahge, graft thrombosis, false aneurysm, distal embolism o Neurological: CVA, spinal ischaemia o GIT: ischaemic gut, aorto-enteric fistula, pancreatitis o Renal: ARF o Respiratory: ARDS o Cardiovascular: MI o Haematological: DIC Endovascular stenting 1. Minimally invasive interventional radiology 2. Catheter places metal stent inside aorta 3. Indications: o Patients unsuitable for open surgery o Infra-renal aneurysms o Anatomy: proximal and distal neck of arteries must allow complete exclusion of aneurysm Endovascular stenting procedure 1. 2. 3. 4. GA / regional Access femoral artery Pass graft over guidewire Deploy graft once in position o Graft achieves final shape through elasticity / thermal memory Complications Infection Leakage Fracture of graft Graft migration Graft occlusion Arterial bypass surgery Examples Femoral-popliteal Femoral-distal Axillo-femoral Femoral-femoral Types of graft 1. Native o o Reverese autologous long saphenous vein graft Insitu long saphenous vein graft (disrupted with valvulotome) 2. Synthetic o PTFE o Dacron Complications 1. 2. 3. 4. Bleeding Infection: wound, graft Suture line aneurysm Graft failure: thrombosis Carotid endarterectomy Indications TIAs in distribution of artery (middle/anterior cerebral territory) Preparation Carotid duplex: extent of stenosis Carotid angiogram Echo, cholesterol, ECG, CT brain (previous CVA) Procedure 1. Local anaesthetic block / intercostal block (allows monitoring of neurological status intra-operatively) - enables operation without a shunt 2. GA allows for better airway control, requires shunt + EEG 3. 4. 5. 6. 7. 8. Incision over sternocleidomastoid (oblique) Dissect down to common carotid, external, internal carotid Tape looped around external carotid for control Heparin infused, longitudinal arteriotomy into carotid distal to site of stenosis Plaque removed distal to proximal in one piece Close arteriotomy with graft/patch (avoid problems of stenosis) with full thickness sutures (+ removal of shunt) + irrigate with heparinised saline Complications Nerve injury - recurrent laryngeal, hyoglossal (12) nerve Haematoma Hypertension / hypotension (carotid body effects) Stroke (1-5%) Follow up 6 month surveillance scans Femoral Embolectomy Indications Acute limb ischaemia Workup Coagulation screen Test foley catheter beforehand Performed under LA/GA Procedure 1. 2. 3. 4. 5. 6. Palpate femoral artery (mid inguinal point) Longitudinal incision over skin Deepen down to femoral artery Sling around CFA, SFA, Profunda Angled vascular clamp on each of three main vessels Transverse (risk of dissection) or Longitudinal (risk of stenosis) arteriotomy into femoral artery 7. Pass catheter proximally up aortic bifurcation; inflate balloon (avoid overdistension damages intima), withdraw any clot (assistant tightens tape to prevent bleeding) o Send clot / embolus for histology - never know what is is! 8. When good inflow, inject heparinized saline up vessel + reapply clamp o If unable to achieve good back bleeding - do on-table angiogram o If unable to achieve good inflow - get help 9. Repeat on SFA, PFA 10. 11. 12. 13. 14. Repair arteriotomy (5/O non-absorbable) Remove clamps, tapes, check haemostasis Insert suction drain Close wound Check + document pulse / clinical condition of limb Complications Dissection Perforation of vessel Amputation Varicose vein Indications Symptomatic veins Cosmesis Varicose ulceration Lipodermatosclerosis Pre-operative workup Hand-held doppler - confirm superficial reflux Venous duplex imaging +/- junction marking - demonstrates incompetent perforators, deep veins Mark veins pre-operatively with indelible marker Tributaries Superficial inferior epigastric Superficial circumflex iliac Superficial / deep external pudendal Lateral / anterior cutaneous vein of thigh Risk factors - any cause of obstruction: DVT, pregnancy, running, malignancy, smoker Trendelenburg operation 1. GA, supine 2. 1.5cm incision lateral and below pubic tubercle (site of SFJ) - 4cm in groin crease 3. Dissect tributaries of SFJ (superficial inferior epigastric, superficial circumflex iliac, deep/superficial external pudendal) 4. Ligate and divide tributarie 5. Ligate SFJ 6. 7. 8. 9. 10. 11. Pass stripper down LSV to knee Stab incision over stripper and deliver Strip vein back to groin Close incision Avulse local varicosities in lower calf Apply compression bandaging Complications Haematoma Recurrence (up to 20%) Saphenous nerve injury - loss of sensation medial thigh Short saphenous vein 1. Transverse skin crease incision 2. Dissect down to SSVJ 3. Tie off junction (avoid sural nerve lateral to SPJ) Other surgical options 1. Endovenous laser ablation 2. Ultrasound guided foam sclerotherapy (risk of thrombosis Parotid gland surgery Indications Benign tumours confined to superifical part of parotid gland Superficial parotidectomy Procedure 1. GA + supine + slight head-up tilt 2. Dissect down to parotid o S-shaped pre-auricular incision (as close to ear as possible to avoid facial nerve) extending unde the ear and down anterior border of SCM o Incision curved around ear lobe to extend for 2-3cm into postauricular groove o Angled acutely over mastoid to be continous with cervical part of incision o Deepen incision down to bony external auditory meatus o Deepen through subcutaneous fat, platysma to stylohyoid muscle o (anterior branch of great auricular nerve usually sacrificed - causes parasthesia of earlobe) 3. Identify branches of facial nerve o Reflect parotid forwards o Dissect divisions and branches of facial nerve (TZBMC) 4. Dissect out parotid duct, ligate o Raise skin flaps superiorly to just above zygomatic arch, anteriorly to anterior border of masseter muscle and inferiorly to anterior border of SCM o Parotid duct dissected forwards as far as anterior border of masseter muscle, then ligate and divide [normally opens 2nd molar] 5. Remove superficial parotid 6. Close o Ensure haemostasis o Close skin with subcuticular suture Complications 1. 2. 3. 4. 5. Bleeding / haematoma Infection Damage to facial nerve Salivary fistula Frey's syndrome: gustatory sweating, hyperhidrosis, pain, flushing in distribution of auriculotemporal nerve. Thought to be due to disorganised post-ganglionic sympathetic fibres and preganglionic parasympathetic fibres following trauma Parotid duct stomatoplasty Indications Obstructive parotitis 1. GA + supine position 2. Nasophryngeal ETT 3. Mouth kept open with dental prop, tongue retracted to contralateral side by assistant 4. Identify parotid papilla (opposite upper 2nd molar) 5. Insert 2 stay sutures above and below papilla 6. Pass dilator through parotid duct and then incise longitudinally down to dilator Surgical airway Tracheostomy Indication Airways obstruction Protection from aspiration (decreased consciousness, GBS, tetanus) Prolonged intubation / long-term ventilation Facilitate airways suction Types of Tubing Metal / plastic Cuffed (reduces risk of aspiration) / uncuffed (used in children - as risk of mucosal ulceration) Windowed - permits speech Open Procedure 1. ETT intubation + GA 2. 3. 4. 5. 6. Sandbag beneath shoulders to maintain neck extension Transverse skin incision midway between cricoid cartilate and suprasternal notch Separate pretracheal muscles Divide thyroid isthmus between clamps + oversew Tracheostomy between 2nd and 4th rings: (1) Bjork flap opens inferiorly (2) vertical slit 7. Insert tube, secure Percutaneous procedure More rapid, less traumatic, doesn't need surgeon/anaethestist 1. 2. 3. 4. 5. 6. 7. 8. LA + fibre-optic bronchscopy to aid insertion Small skin incision between cricoid / sternal notch 14G cannula Guide wire through Remove cannula Ram Rhino dilator over guidewire to make a big hole Pass tracheostomy over guidewire Secure in place, get a CXR Complications: Nerve, vessel damage, pleural injury Stenosis if incision too high Tracheo-inominate fistula if too low Bleeding Displacement Blockage Infection Mucosal ulceration