Development of Extraembryonic membranes and
advertisement

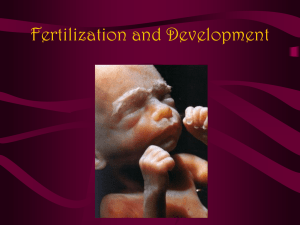
Development of Extraembryonic Membranes and Bilaminar Embryo Embryo: 1-8 wks-all organ systems have been established but not fully developed. Fetus: 9 wks-birth, growth and maturation, little continued anatomic development. Maturation of the lungs determines viability of the premature fetus. The umbilical cord attaches to the fetal placenta. Chorionic sac-outer membrane-becomes part of placenta Amnion-membrane that surrounds the embryo & fetus &contains amniotic fluid which is maternal tissue fluid that diffuses into the amniotic cavity and can diffuse back and forth into the endometrium. Fetal urine is added to the fluid as it develops. Fetal kidneys don’t concentrate the urine-same time this happens the fetus begins swallowing. This establishes a balance where the fetus adds & takes away from the fluid. Problem if fetus can’t swallow or urinate. Fetal cells that are exfoliated are in the amniotic fluid so that you can obtain a sample. AF has no nutritive value but serves to hydrate (b4 skin develops) and as a shock absorber. Chorion is outside the amnion. Cotyledons: lobules of the placental chorion-functional unit of the placenta. Maternal aspect of placenta is deep in the endometrium oriented away from the fetus. Original cotyledons enlarge and as the placenta enlarges it adds more peripheral cotyledons. The fetal surface of the placenta has blood vessels and the umbilical cord. The placenta is about 2” thick and 10-12” in diameter. The placenta will usually implant high on the posterior wall of the endometrium. Zona pellucida doesn’t allow cells to enlarge so as they divide they become smaller Morula: means mulberry-loose collection of cells Prefix: blast: formative structure Blastocyst-cystic in nature, contains blastoceol. Zona pellucida has dissolved and the blastocyst can implant. After ovulation the walls of the ovarian follicle are thrown into folds which develop a glandular structure called the corpus luteum which produces progesterone and some estrogen. 2wks after ovulation the corpus luteum degrades. It produces progesterone and when lost signals the loss of the endometrium (14 days after ovulation and shifts into menstrual period). A developing embryo’s cells will produce progesterone (even before implantation) to maintain and ripen the endometrium. This acts to signal the mother’s body that the embryo is present. The time between ovulation and menstruation is very consistent (14 days). The time between menstruation and ovulation is variable. Conceptus: products of fertilization-extraembryonic tissue and embryo proper Corona Radiata: follicular cells that are ovulated w/ the oocyte and helps cilia in the uterine tube transport more easily (larger). Irregular outer surface. Ovulated mass releases signals that act as directions for approaching sperm. Acrosomal vesicles release enzymes that digest the coronal radiata and allow sperm to reach the zona pellucida- docking receptors allow recognition and digestion of a path through ZP to the oocyte. Fuses with oocyte membrane and nuclear material enters triggering cortical reaction. Causing a chemical change w/in ZP and the oocyte retracts from the ZP (prevents polyspermy bc digestion of ZP3 receptors takes time). Zona pellucida is produced by the corona radiata and the oocyte. It is acellular and surrounds the oocyte within the follicle. It has oocyte processes extending into it as well as corona radiata processes. Moniters and controls environment that the oocyte is developing in. Later on it helps to aid spermatazoan in fertilization. Functions to hold the first cells of mitotic division together. Prevents implantation until the proper age then disappears. Endometrium: mucosal lining of the uterus composed of glandular epithelium, fibrous CT stroma, BVs Myometrium: muscular layer of the uterus. W/in ZP-morula-blastula: these cells have numerous villi and junctional complexes for communication 5-6 days after fertilization the conceptus moves into the uterine cavity and “hatches” from the ZP and it can swell up (small cells enlarge by uptake of fluid and blastoceol begins developing) 6-7 days it makes contact w/ endometrium and begins implantation Implantation: movement of the conceptus from the uterine cavity into the stroma of the endometrium-breaking through the epithelial lining. Interstitial implantation- w/in the stroma and looses contact with uterine cavity. Endometrium releases chemical that attract the conceptus which release substances that trigger changes w/in the endometrium. Both processes must occur for implantation to happen. Decidua: altered endometrial stroma (to fall away-deciduous) changes its nature and behavior after implantation (can’t recognize foreign matter), part of the after birth Basalis: between the conceptus & myometrium Capsularis: between the conceptus & uterine cavity (temporary) Parietalis: everything else “wall of uterine cavity” Ex: Decidua basalis is the myometrium basal to the conceptus. Decidua capsularis degenerates as the conceptus enlarges Inner cell mass: embryoblast-gives rise to the embryo proper and can be divided into epiblast (ecto- meso- & endoderm) &hypoblast (extraembryonic mesoderm-outside the embryo proper) Outer cell mass: trophoblast (tropho-to feed or support)-differentiates into cytotrophoblast (discrete cells and reserve-develop into something else and deplete in # as development proceeds) and then form the syncytiotrophoblast (differentiated syncytium)-releases hormones and comes in contact w/maternal blood and tissue. Lacuna (space)-membrane bound space w/in syncytiotrophoblast will coalesce and form the intervillous space w/in the placenta and will contain maternal blood (grows and eats into maternal BVs). Cytotrophoblast comes in contact w/ maternal tissue but not maternal blood. Syncytiotrophoblast (red). Cytotrophoblast (yellow external layer). Embryoblast (blue). Hypoblast forms second lining w/in trophoblast (CTB) over the embryoblast. Hypoblast proliferates to form EE mesoderm (btwn hypoblast and inner cell mass). Endometrial glands in yellow. CTB grow into the STB giving rise to more STB, extraembryonic mesoderm follows. Columns of CTB grow into STB and become hollow as extraembryonic mesoderm grows in. Extraembryonic blood vessels develop w/in the extraembryonic mesoderm that will link up with the circulatory system developing w/in the embryo proper. CTB cells migrate through the STB and come to the outside where they proliferate and spread along the interface of STB and decidua. Primary Chorionic Villi: consist of STB and CTB (developmental stage) Seconday chorionic villi: consist of STB, CTB and extraembryonic mesoderm Tertiary chorionic villi: core of ee mesoderm w/fetal blood vessels, surrounded by CTB and then STB. These vessels hang into the maternal blood filled chorionic villi space.