microbiology & infectious diseases journals
advertisement

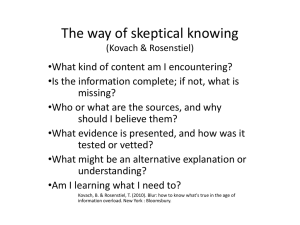
June/July 2015 - Microbiology/ID Pharmacists Journal Club (IDJC) UKCPA Pharmacy Infection Network: Micro/ID Pharmacists Journal Club June/July 2015 News of the Antibiotic World Headlines! Selected highlights from this month’s journal club* Multi-resistant TB! Sepsis and diet! Linezolid for XDR TB! Antibiotics for pancreatitis! *Health Warning – Click on the journal hyperlink in the table of contents to view full journal club reviews and consult original articles for details of caveats and disclaimers! Editorial Welcome to the UKCPA Pharmacy Infection Network’s journal club! Our aim is to signpost specialist microbiology/ID pharmacists to important new research published in the microbiology/ID, general medical and pharmacy literature and to summarise the need-to-know messages. Journals have been selected on the basis of impact factor and must carry new original research (review journals are excluded). We are immensely grateful to the pharmacists who give freely of their precious time to perform this vital service on behalf of their colleagues and strongly encourage new reviewers to come forward and contact us to share the burden as many hands make light work. Note: there is no need for expert critical appraisal skills. As an incentive to get involved, reviewers receive their copy of the report as soon as it is prepared and 1-2 months before publication on the UKCPA website. Jon Urch (North Bristol) & Kieran Hand (Southampton) Table of Contents (hyperlinks) News of the Antibiotic World Headlines! ................................................................................................ 1 Editorial ................................................................................................................................................... 1 Table of Contents (hyperlinks) ............................................................................................................ 1 MICROBIOLOGY & INFECTIOUS DISEASES JOURNALS............................................................................. 2 Lancet Infectious Diseases .................................................................................................................. 2 Clinical Infectious Diseases ................................................................................................................. 2 Journal of Infectious Diseases ............................................................................................................. 2 Emerging Infectious Diseases ............................................................................................................. 2 Journal of Antimicrobial Chemotherapy ............................................................................................. 3 1 June/July 2015 - Microbiology/ID Pharmacists Journal Club (IDJC) Antimicrobial Agents and Chemotherapy........................................................................................... 3 Clinical Microbiology and Infection .................................................................................................... 4 Journal of Clinical Microbiology .......................................................................................................... 4 International Journal of Antimicrobial Agents .................................................................................... 5 Journal of Hospital Infection ............................................................................................................... 5 BMC Infectious Diseases ..................................................................................................................... 3 European Journal of Clinical Microbiology ......................................................................................... 5 GENERAL MEDICAL JOURNALS................................................................................................................ 7 New England Journal of Medicine ...................................................................................................... 7 The Lancet ........................................................................................................................................... 8 JAMA – Journal of the American Medical Association........................................................................ 9 Annals of Internal Medicine ................................................................................................................ 9 PLOS Medicine .................................................................................................................................... 9 British Medical Journal........................................................................................................................ 9 JAMA Internal Medicine (formerly Archives of Internal Medicine) .................................................... 9 BMC Medicine ................................................................................................................................... 10 Cochrane Database of Systematic Reviews ...................................................................................... 10 MICROBIOLOGY & INFECTIOUS DISEASES JOURNALS Lancet Infectious Diseases No submission Clinical Infectious Diseases No submission Journal of Infectious Diseases No submission Emerging Infectious Diseases Article citation: Owusu-Edusei Jr K, Chesson HW, Gift TL, Brunham RC, Bolan G. Costeffectiveness of chlamydia vaccination programs for young women. Emerg Infect Dis. 2015 Jun http://dx.doi.org/10.3201/eid2106.141270 Comments: this research looks at the cost effectiveness of a chlamydia vaccination in young women aged 14 – 24 years; there is currently no vaccination available but a similar model was used during the development of the HPV vaccination. Chlamydia remains a major public health problem; there were ≈105.7 million new cases of this disease among adults 15–49 years of age worldwide in 2008. The researchers used a compartmental heterosexual transmission model that looked at several possible scenarios and found that a highperformance vaccine could potentially eliminate chlamydia infection when coverage was 2 June/July 2015 - Microbiology/ID Pharmacists Journal Club (IDJC) high (>75%) among susceptible persons before their sexual debut. A highly efficacious chlamydia vaccine with long duration of immunity would cost <$10,000/QALY saved. Article citation: Kempker RR, Kipiani M, Mirtskhulava V, Tukvadze N, Magee MJ, Blumberg HM. Acquired drug resistance in Mycobacterium tuberculosis and poor outcomes among patients with multidrug-resistant tuberculosis. Emerg Infect Dis. 2015 Jun http://dx.doi.org/10.3201/eid2106.141873 Comments: This small study carried out in Georgia looked at 141 patients with multi drug resistant TB. Drug susceptibility testing to second line drugs was carried out at baseline and every 3rd month. Acquired resistance was observed in 14% of patients with a rate of 9.1% for ofloxacin and 9.8% for capreomycin. Baseline cavity disease and resistance to >6 drugs were associated with acquired resistance. Patients with TB that had acquired resistance were at significantly increased risk for poor treatment outcome compared with patients without these isolates (89% vs. 36%; p<0.01). The authors conclude that acquired resistance occurs commonly among patients with MDR TB and impedes successful treatment outcomes. Article citation: Smith SE, Ershova J, Vlasova N, Nikishova E, Tarasova I, Eliseev P, et al. Risk factors for acquisition of drug resistance during multidrug-resistant tuberculosis treatment, Arkhangelsk Oblast, Russia, 2005–2010. Emerg Infect Dis. 2015 Jun http://dx.doi.org/10.3201/eid2106.141907 Comments: Another small study looking at 202 patients with MDR-TB. WHO estimates that almost half of all TB cases in countries of the former Soviet Union involve resistance to >1 drug and that 1 in 5 TB patients has MDR TB. Data was collected prospectively between 2005 and 2008. Acquisition of resistance to capreomycin and of extensively drug-resistant TB were more likely among patients who received <3 effective drugs than among patients who received >3 effective drugs (9.4% vs. 0% and 8.6% vs. 0.8%). Poor outcomes were more likely among patients with acquired capreomycin resistance (100% vs. 25.9%), acquired ofloxacin resistance (83.6% vs. 22.7%), or acquired extensive drug resistance (100% vs. 24.4%). The authors conclude that to prevent acquired drug resistance and poor outcomes, baseline susceptibility to first- and second-line drugs should be determined quickly, and treatment should be adjusted to contain >3 effective drugs. Journal of Antimicrobial Chemotherapy No submission Antimicrobial Agents and Chemotherapy Article citation: Schmitz et al, Determination of Appropriate Weight-Based Cut-offs for Empiric Cefazolin Dosing Using Data from a Phase 1 Pharmacokinetics and Safety Study of Cefazolin Administered for Surgical Prophylaxis in Paediatric Patients Aged 10 to 12 Years. Antimicrobial Agents and Chemotherapy (July 2015), Vol 59, No.7, Pg 4173-4180. 3 June/July 2015 - Microbiology/ID Pharmacists Journal Club (IDJC) Comments: A small number (N=12) of paediatric patients were given either a 1g or 2g STAT dose depending on their weight for surgical prophylaxis. The pharmacokinetic data gathered gave a mean terminal elimination half-life of 1.95hrs and clearance as 0.804ml/min/kg. The results showed that a cut of point of 60kg should be used when using the higher dose. Article citation: Schroeck et al, Factors Associated with Antibiotic Misuse in Outpatient Treatment for Upper Respiratory Tract Infections. Antimicrobial Agents and Chemotherapy (July 2015);Vol 59, No.7, Pg 3848-3852. Comments: Antibiotic prescribing for URTIs was reviewed from 2009 to 2011 in primary care and in one hospital’s A+E department. The study found that 64.2% of the antibiotics were prescribed inappropriately and that there was poor compliance with the American Get Smart Campaign. Article citation: Bouillaut et al, Effects of Surotomycin on Clostridium difficile Viability and Toxin Production In Vitro. Antimicrobial Agents and Chemotherapy (July 2015), Vol 59, No.7, Pg 4199-4204. Comments: The results from this study showed that Surotomycin killed C.diff cells that are growing out of germinated spores, exponential-phase cells, and stationary-phase cells of strain UK1 more rapidly than does metronidazole or vancomycin. Surotomycins mode of action is causing a loss of proton gradient but it does so by depolarising the membrane without causing permeability of large molecules. Article citation: Justo et al, Pharmacokinetics of Ceftaroline in Normal Body Weight and Obese (Classes I, II and III) Healthy Adult Subjects. Antimicrobial Agents and Chemotherapy (July 2015), Vol 59, No.7, Pg 3956-3965. Comments: The pharmacokinetics of Ceftaroline was studied in patients weighing 50kg to 180kg (N=32). Each patient was given a STAT dose of 600mg. The maximum concentration and area under the curve were approximately 30% lower in subjects with a BMI of >40kg/m2. There was not much difference in the half-life between the study groups; however the Vd was significantly higher in the obese patients. Clinical Microbiology and Infection No submission Journal of Clinical Microbiology Article citation: J. Clin. Microbiol. 2015, 53(7): 2022-2029 Rapid Detection of Emerging Pathogens and Loss of Microbial Diversity Associated with Severe Lung Disease in Cystic Fibrosis Flight WG et al Comments Ribosomal intergenic spacer analysis (RISA) is a simple, single stop PCR based method for profiling microbial diversity that detects the variation in size of the intergenic transcribed spacer (ITS) region between 16S and 23S rRNA genes. It was used as a routine PCR diagnostic to detect microbial diversity in adult CF patients in a large observational study and compared with 16S rRNA gene pyrosequencing and conventional culture. 200 paired sputum samples from 93 adult CF patients underwent RISA and 179 were successfully cultured. 59 samples underwent 16S rRNA gene 4 June/July 2015 - Microbiology/ID Pharmacists Journal Club (IDJC) pyrosequencing which represented overall microbial diversity and displayed the same profile groups as for RISA. There were 2 major group profiles identified: emerging non-fermenting Gram negative organisms (eNFGN) and Pseudomonas groups. The eNFGN’s were mainly Burkholderia, Achromobacter, Ralstonia or Stenotrophomonas. The main organism within the Pseudomonas group was Pseudomonas aeruginosa. 11.8% of cases where no CF pathogens were cultured, had a pathogen identified by RISA and confirmed by 16S gene pyrosequencing. There was significantly lower diversity seen when Burkholderia was the dominant strain in the sample. Low diversity was associated with poor lung function. The absence of Streptococcus was significantly reduced in patients with lung function in the lowest quartile. Therefore high pathogen abundance and low microbial diversity correlate with severe lung disease in CF. RISA is able to rapidly differentiate sputum samples dominated by Pseudomonas and eNFGN, identify these pathogens further and report on whether the samples are diverse of pathogen dominated in CF sputum samples. Article citation: J. Clin. Microbiol. 2015, 53(6): 1947-1950 Colonization with Escherichia coli Strains among Female Sex Partners of Men with Febrile Urinary Tract Infection Ulleryd P et al Comments: Strain sharing between men with an E coli UTI and his healthy female sexual partner (FSP) was studied for their frequency and characteristics of any shared strains. 10 men and their FSP participated. 76 rectal, vaginal, and urine cultures showed that 59 (78%) isolated E. coli. There were 23 unique E. coli strains, which were predominantly from phylogroup B2 and represented 15 clonal complex. 17 strains were identified as extraintestinal pathogenic E. coli. Of the 23 strains, 6 occurred in both members of a particular couple and only in that couple. All 6 (100%) shared strains, versus 4 (24%) non-shared strains, represented the male’s index FUTI isolate. Shared strains also were more likely to cause asymptomatic bacteriuria (ABU) or acute cystitis and to colonize the woman’s rectum and/or vagina. Shared strains caused sustained co-colonization and recurrent symptomatic UTI and/or ABU in two couples. 60% of FSPs were frequently co-colonization with their male partner’s index E. coli strain. The clinical implications of co-colonization include risks of acute UTI in an FSP due to the male partner’s UTI strain and reintroduction of the strain into the index subject from a cocolonized partner. Shared strains were distributed more broadly, caused more infections, and exhibited more uropathogenic traits than did non-shared strains. This indicates that certain E. coli traits and lineages promote both UTI pathogenesis and intestinal colonization. Frequent cocolonisation demonstrates that male UTIs are sometimes sexually transmitted and these strains were often urovirulent traits promoting colonisation and transmission. International Journal of Antimicrobial Agents No submission Journal of Hospital Infection No submission BMC Infectious Diseases Article title: An outbreak of multi-drug resistant Escherichia coli urinary tract infection in an elderly population: a case-control study of risk factors First author & initial: Ikram R, Psutka R, Carter A, Priest P Page numbers or citation details if advance eprint: BMC Infectious Diseases 2015, 15 :224 (9 June 2015) Comments: 5 June/July 2015 - Microbiology/ID Pharmacists Journal Club (IDJC) P= patients aged >65 who had a multi-drug resistant e.coli isolated in the lab. Defined as resistant to more than 3 antibiotics but not ESBL producer. I= to investigate the risk factors associated with getting this C=n/a O = This case-control study found individual and predisposing risk factors that were associated with the outbreak. Individual risk factors that showed an association with the MDR E. coli UTI included being female, having diabetes, having recurrent UTIs and requiring a higher level of care all of which have been described in previous studies. The odds ratios associated with female gender, diabetes, recurrent UTIs, and age over 85 were around 2 to 3 in all analyses. Catheterisation increased the risk to a similar degree, but predisposing factors with much higher ORs were high dependency care and prescriptions of antimicrobials to which the MDR E. coli was resistant in hospital, particularly 3 or more courses. This study highlights the importance of joined up approach to antimicrobial stewardship, to include primary care, secondary care and nursing homes in order to prevent MDR e.coli infections in this population. Article title: Diet patterns and risk of sepsis in community-dwelling adults: a cohort study First author & initial: Orlando M. Gutiérrez, Suzanne E. Judd, Jenifer H. Voeks, April P. Carson, Monika M. Safford, James M. Shikany and Henry E. Wang Page numbers or citation details if advance eprint: BMC Infectious Diseases 2015, 15:231 doi: 10.1186/s12879-015-0981-1 Comments: This American study looked at the diet of patients who had had an episode of sepsis to see if diet affected this at all. They found that a higher score for a southern diet (added fats, organ meats, fried foods, processed meats, sugar-sweetened beverages and greens typical of southern cuisines) were independently associated with higher long-term risk of sepsis, particularly among individuals of black race. The authors state that this is important as it is the first study to link diet patterns with sepsis risk in a large US cohort, underscoring the important influence of diet on sepsis, and that studies elucidating whether these observed patterns are causal may be warranted. Article title: Agreement on the prescription of antimicrobial drugs First author & initial: Eduardo Casaroto1, Alexandre R. Marra2*, Thiago Zinsly, Sampaio Camargo1, Ana Rita Araújo de Souza1, Carlos Eduardo Saldanha de Almeida1, Elizia Piassi Pedroti1, Elivane da Silva Victor3, Oscar Fernando Pavão dos Santos2, Michael B. Edmond4 and Alexandre Holthausen Campos3 Page numbers or citation details if advance eprint: BMC Infectious Diseases 2015, 15:248 doi:10.1186/s12879-015-0992-y Comments: This study looked at whether two ID specialists agreed with the consultant on the prescribing of antibiotics or antifungals for patients on ITU. They found that in less than half of the cases (48%) did both specialists agree with the prescribing consultant, and 22% both specialists disagreed with the antibiotic choice. This study highlights the difficulty in choosing antibiotic treatment for patients, even for 2 specialists well acquainted with the hospital guidelines, local susceptibility data and patient details. The 6 June/July 2015 - Microbiology/ID Pharmacists Journal Club (IDJC) authors state that to minimize such differences we need faster and more accurate diagnostic tests as well as a better understanding by frontline providers of clinical guidelines and local susceptibility patterns. Article title: Outpatient parenteral antimicrobial therapy (OPAT) in patients with cystic fibrosis First author & initial Page numbers or citation details if advance eprint: Maya Graham Pedersen1*, Søren Jensen-Fangel1, Hanne Vebert Olesen2, San deep Prataprao Tambe3 and Eskild Petersen1 Comments: Retrospective study looking at complications associated with OPAT therapy in CF patients. The authors conclude that all patients were pleased to be offered the opportunity for OPAT. Using an infusion pump to administer the antibiotic treatment minimized peripheral venous line complications. The frequency of complications leading to removal of the catheter was about the same for PICC-lines and PACs, but the average life-time of the latter was much longer. Allergic reactions were not a major problem. European Journal of Clinical Microbiology No submission GENERAL MEDICAL JOURNALS New England Journal of Medicine Title Linezolid for XDR-TB - Final Study Outcomes Issue: New England Journal of Medicine. 373(3):290-291, July 16, 2015 Lee, Myungsun M.D. 1; Song, Taeksun Ph.D. 1; Kim, Youngran R.N. 1; Jeong, Ina M.D. 2; Cho, Sang Nae D.V.M., Ph.D. 3; Barry, Clifton E. III Ph.D. 4 38 patients with extensive drug resistant TB (all resistant to Isoniazid, Rifampicin, Ofloxacin and Moxifloxacin) had Linezolid added to their combination anti-TB therapy. They were treated with Linezolid for approximately 2 years. 12 months after the study ended they were reassessed. 27 had negative results on sputum culture. (3 were lost to follow up, 8 withdrew from the study -4 of these due to acquired Linezolid resistance.) Although many received a dose of 600mg for the duration of the trial several experienced side effects with this dose e.g. optic neuropathies and anaemia, and had their doses reduced to 300mg. The authors believe that incorporation of Linezolid into a pre-existing anti TB drug regimen substantially improved culture conversion rates. This study is limited as the numbers were small and there was no control group to compare with. Title: A Variegated Squirrel Bornavirus Associated with Fatal Human Encephalitis Journal: The New England Journal of Medicine. 373(2):154-162, July 9, 2015. Authors: Hoffmann, Bernd D.V.M et al. 7 June/July 2015 - Microbiology/ID Pharmacists Journal Club (IDJC) In Germany a case was reported of three men who all died with 2 years of each other of suspected viral encephalitis. All received broad spectrum antimicrobial treatment and ITU level care. While they were alive no infectious agent could be detected by means of microscopic, culture, molecular or serologic investigations of cerebrospinal fluid samples, biopsy samples or serum. Post-mortem examination of the first 2 patients could not detect any microorganisms -though signs of infection were present. All three men came from the same area of Germany and were friends having shared the same hobby of squirrel breeding. They had exchanged squirrels for breeding purposes. Post mortem examination on the 3rd patient and analysis of archived brain tissue from the first two patients using new metagenomics techniques isolated a previously unknown zoonotic pathogen (VSBV-1). This pathogen was also isolated from an oropharyngeal swab taken from one of the squirrels all three men had had contact with . The Lancet Article citation: Acute pancreatitis Review Article Pages 85-96 Paul Georg Lankisch, Minoti Apte, Peter A Banks Comments: This is a comprehensive article on acute pancreatitis but focusing on the antibiotic therapy the article suggests prophylactic antibiotics are not indicated in the management of acute pancreatitis. Surgical resection of pancreatic necrosis is an option but more conservative interventions are now favoured, one of which is antibiotics. Antibiotic treatment alone can heal infected necrosis and this is now the first step when such lesions are shown. Antibiotic treatment is possible in almost two-thirds of patients with necrotising pancreatitis, with a mortality of 7% Article citation: New guidelines for prevention and management of implantable cardiac electronic device-related infection Pages 2225-2226 Jonathan A T Sandoe, et al. Comments: This article discusses the increases in infections related to implanted cardiac electronic devices (ICED). These infections are often complex and can be life threatening in patients with associated endocarditis. The British Society of Antimicrobial Chemotherapy have established a working party in collaboration with key UK national societies to develop guidelines that would improve the quality of care provided to patients with implantable cardiac electronic devices. The guidelines provide an educational resource for all relevant health-care professionals; encourage a multidisciplinary approach to the management of ICED infection; promote a standardised approach to the diagnosis, management, surveillance, and prevention of ICED infection through pragmatic evidence-rated recommendations; and provide advice about future research and audit projects. Article citation: Tenofovir alafenamide verses tenofovir disoproxil fumarate coformulated with elvitegravir, cobicistat, and emtricitabine, for initial treatment of HIV-1 infection: two randomised, double-blind, phase 3, non-inferiority trials. Pages 2606-2615. Paul E Sax et al. Comments: The tenofovir alafenamide containing regime was non-inferior to the tenofovir disoproxil fumerate regime, both showed high efficacy. The tenofovir alafenamide containing regime had smaller decreases in glomerular filtration rate, less proteinuria, and a more favourable effect on hip and 8 June/July 2015 - Microbiology/ID Pharmacists Journal Club (IDJC) spine bone mineral density. The hope is that these findings will translate into improved safety of tenofovir alafenamide based therapy with maintaining high efficacy rates. Article citation: Tenofovir alafenamide for HIV infection: is less more? Christina Wyatt and Jared Baeten Comments: This commentary discusses briefly how HIV therapy has vastly improved over the years, lower pill burden, efficacious and less toxic than the early generation antiretrovirals. The author makes reference to the published trial mentioned above which demonstrates the superior side effect profile of Tenofovir alafenamide when compared to tenofovir disoproxil fumerate but it suggests caution as to whether the small difference shown in the study will translate into clinically meaningful benefits when used more widely. If post marketing experience does confirm the improved safety profile then the safer drug might reduce costs through reduced toxic effect monitoring and adverse event monitoring. The smaller dose of tenofovir alafenamide (25mg) compared to tenofovir disoproxil fumerate (300mg) might also reduce manufacturing costs. These benefis could be particularly beneficial in resource-limited settings. Article citation: antiretroviral chemoprophylaxis: new successes and questions Kenneth Mayer. Comments: The article discusses the PROUD and IPERGAY studies which both showed reduced HIV transmission rates in the groups that took pre-exposure prophylaxis (PrEP) in the form of tenofoviremtricitabine (86% decrease in transmission rates when compared to control group). Early initiation of antiretoviral therapy has been shown to reduce transmission in sero-discordant couples by 96%. Similar studies looking at early initiation of antiretrovirals and/or PrEP in east Afrca howed significant transmission risk reductions. Other studies in southern African looking at the benefits of pericoital tenofovir gel have shown mixed results, though due to poor compliance with the study mediation. The article then goes on to discuss what these study findings mean for future practice. JAMA – Journal of the American Medical Association No submission Annals of Internal Medicine No articles of interest PLOS Medicine No submission British Medical Journal No submission JAMA Internal Medicine (formerly Archives of Internal Medicine) No articles of interest 9 June/July 2015 - Microbiology/ID Pharmacists Journal Club (IDJC) BMC Medicine No submission Cochrane Database of Systematic Reviews Nothing of interest this month Mayo Clinic Proceedings No submission 10