Spironolactone and Hyperaldosteronism
Running head: SPIRONOLACTONE AND HYPERALDOSTERONISM
Evidence Based Practice Critically Appraised Topic
Spironolactone and Hyperaldosteronism
Matthew Espinosa, RN, FNP-S
University of Mary
March 4, 2014
1
Running head: SPIRONOLACTONE AND HYPERALDOSTERONISM 2
Case Scenario
A 48 year old female presents to the clinic for follow-up hypertension. Her blood pressure has been variable at home. The patient denies shortness of breath, chest pain, and claudication. The patient does have a history of hyperlipidemia. She has been maintaining a low salt diet, her edema is 1-2+ and has also varied during her last few visits. The patient has a Framingham risk score of 2% but could be less than 1% with better control of blood pressure and lipids. Potassium levels have been low, today 3.2. mEq/L. Due to continuously low potassium levels she was screened for primary aldosteronism. Her serum aldosterone was 24 ng/dL with an elevated plasma renin activity level of 51 ng/mL/hr. The patient has been on spironolactone therapy for over a year.
Clinical Question
In patients with idiopathic hyperaldosteronism, will spironolactone be an effective treatment for essential hypertension versus placebo?
Articles
Fischer, E., Beuschlein, F., Degenhart, C., Jung, P., Bidlingmaier, M., & Reincke, M. (2012).
Spontaneous remission of idiopathic aldosteronism after long-term treatment with spironolactone: results from the German Conn's Registry. Clinical Endocrinology,
76(4), 473-477. doi:10.1111/j.1365-2265.2011.04243.x
Batterink, J., Stabler, S.N., Tejani, A.M., & Fowkes, C.T. (2010). Spironolactone for hypertension. Cochrane Database of Systematic Reviews, (8), doi:10.1002/14651858.CD008169.pub2
Running head: SPIRONOLACTONE AND HYPERALDOSTERONISM 3
Summary and Appraisal of Key Evidence
Study 1
According to Fischer, et al. (2012), primary aldosteronism (PA) has been recognized as the most frequent cause of hypertension. The main causes are aldosterone-producing adenoma (APA) and idiopathic bilateral adrenal hyperplasia (IHA), accounting for more than 95% of the cases. The cure rate after unilateral or bilateral adrenalectomy in IHA is only 19%. Therefore, IHA is usually treated by lifetime administration of mineralocorticoid receptor (MR) antagonist, the drug of choice being spironolactone.
The German Conn’s Registry founded in 2006 began a research project in 2008. The study began with invites sent to 164 subjects with PA from an institution in Germany. From the
164 invites 142 patients responded and a consent was signed to be in the study. Of the 142 patients: 41 patients were classified as IHA, 87 as AHA, and 12 patients, with the underlying cause being PA, was inconclusive and they were treated with spironolactone.
Four patients were excluded for missing follow-up visits.
This left 37 patients with IHA that were treated with spironolactone. The average period of treatment being 5.8 years which put two patients into remission; one with complete remission and the other with partial remission. Although the other 35 patients with IHA did not experience partial or complete remission, the average blood pressure of those 35 patients before the study was 170/100 and the average blood pressure after the study was
132/81; demonstrating that patients treated with spironolactone, who had IHA, were able to significantly decrease the blood pressure into normal ranges.
Running head: SPIRONOLACTONE AND HYPERALDOSTERONISM 4
Study 2
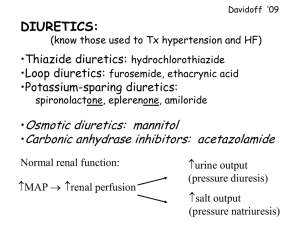
According to Batterink, et al. (2010), hypertension is typically defined as a blood pressure greater than 140/90 mmHg. Spironolactone antagonizes the mineralocorticoid receptors resulting in fewer activated sodium channels at the luminal membrane, and fewer sodium potassium ATPase pumps at the interstitial space membrane. This leads to a greater loss of sodium and subsequent reduction in blood volume while potassium is retained.
Batterink, et al. (2010), performed a meta-analysis of six total studies; one study was a parallel group randomized controlled trial and five were randomized cross-over trials. All randomized control trials (RCT) (parallel group and cross-over) were aimed to determine the extent to which spironolactone reduces blood pressure, the adverse effects profile, and to determine the clinical impact of its use for hypertension.
137 patients were included in the five cross-over studies. These patients received either placebo or daily doses of spironolactone. The one parallel group RCT, with 25 patients, received either spironolactone daily or placebo for 8 weeks.
This meta-analysis shows that spironolactone reduces systolic/diastolic blood pressure by approximately 20/7 mmHg compared to placebo when doses of 100-500 mg daily are given. Doses of 25 mg daily or less did not statistically reduce systolic or diastolic blood pressure compared to placebo.
Clinical Bottom Line
Based on these two studies spironolactone is an effective treatment in the patient with idiopathic hyperaldosteronism causing hypertension when compared to placebo. Further evidence-based research is needed to determine appropriate treatment plans for those with risk factors and comorbidities. According to Batterink et al. (2010), none of the
Running head: SPIRONOLACTONE AND HYPERALDOSTERONISM 5 studies reported clinical impact of spironolactone (i.e. whether spironolactone reduced heart attacks or strokes compared to placebo.) Overall reporting of adverse effects was poor so no conclusions can be drawn.
Implications for Practice
Based on the initial case scenario spironolactone is the treatment of choice. However, proper assessment of the cause of hypertension is mandatory to treat each patient. The patient clearly has an elevated serum aldosterone level as well as an elevated plasma renin level. According to McPherson & Pincus (2011), the patient should have stopped spironolactone for 4-6 weeks before testing serum aldosterone and plasma renin as it can directly affect those results. In the case scenario, the patient had not stopped her medications prior to being tested. This patient will need to be discontinued from her medication and treated with other vasodilators for 4-6 weeks to properly assess the underlying cause of her hypertension being idiopathic hyperaldosteronism.
Running head: SPIRONOLACTONE AND HYPERALDOSTERONISM 6
References
McPherson, R.A. & Pincus, M.R. (2011). McPherson: Henry’s clinical diagnosis and laboratory
methods. Philadelphia, PA. Elsevier. Retrieved from: http://www.mdconsult.com/books/page.do?eid=4-u1.0-B978-1-4377-0974-
2..00024-5--s0350&isbn=978-1-4377-0974-2&type=bookPage&from=content