Running head: THE NURSE IN COMPLEMENTARY AND
advertisement

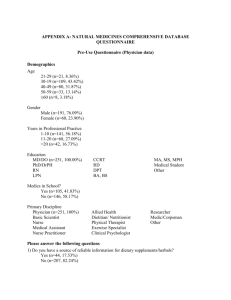
Running head: THE NURSE IN COMPLEMENTARY AND ALTERNATIVE MEDICINE The Nurse in Complementary and Alternative Medicine Richardia Gibbs-Hook Ferris State University 1 2 THE NURSE IN COMPLEMENTARY AND ALTERNATIVE MEDICINE Abstract This paper explores the definition of Complementary and Alternative Medicine and how its use impacts conventional medicine. Information about lack of communication concerning use of herbal products by patients as well as the fact that patients are not routinely asked about use will be provided. The nurse is profiled as the member of the healthcare team who is in a position to enhance communication concerning a patient’s use of herbal supplements and thusly prevent adverse reactions from occurring. 3 THE NURSE IN COMPLEMENTARY AND ALTERNATIVE MEDICINE The Nurse in Complementary and Alternative Medicine As Complementary and Alternative Medicine (CAM) is being utilized by more Americans, the implications for conventional medicine are many. Patients may be unwilling to volunteer herbal product use with physicians or nurses unless asked. The role of the nurse as patient advocate and the member of the healthcare team who has the most frequent and combined time with the patient puts the nurse in a position to obtain the most accurate information about herbal supplement use. As there are potential adverse reactions from combining herbal and conventional medicine, the nurse has an ethical responsibility to obtain herbal supplement usage information from the patient. Complementary and Alternative Medicine: Defined According to the United Sates National Center for Complementary and Alternative Medicine, CAM can be defined as “a group of diverse medical and healthcare systems, practices and products that are not presently considered to be part of conventional medicine” (2011, Zhang & Fong & Changli). This includes but is not limited to such products and practices as herbal supplements, vitamins, guided imagery, acupuncture, yoga, meditation, tai-chi, healing ceremonies and prayer (2011, Egede & Bais). Prevalence of Use According to Zhang herbal product use is on the rise “is used by more than 38.2 million people in the United States with thousands of products available world-wide” (2011). Ventola attributes the increase in use to dissatisfaction with conventional medicine, frustration with an impersonal medical system and for some consumers a feeling of control of illness or health promotion (2011). Also, the prevalence of mass media coverage of adverse reactions and side effects of conventional medications and treatments may drive a health care consumer to seek 4 THE NURSE IN COMPLEMENTARY AND ALTERNATIVE MEDICINE alternative or complementary therapies (Ventola, 2011). The internet is a tool that is used by many consumers and a vast amount of information is available about herbal remedies on any search engine. Risks Herbal supplements are not regulated in the same way that conventional medicine is with double blind studies and approval as medicine by the Food and Drug Administration. Many herbal supplements are either “unintentionally mixed with contaminants or intentionally mixed with pharmacological agents such as “warfarin, estrogen, corticoids” and other substances (2011, Zhang). Many consumers purchase herbal supplements because they have been led to believe that herbal is “all natural” and hence safe. Because the herbal industry is not regulated worldwide, it is for health practitioners to assess for accuracy in treatment of their patients take herbal supplements along with conventional medicine. Many drugs have adverse reactions when taken concurrently with popular herbal remedies. According to Zhang, there are documented safety concerns with “thirty-four drugs, including anticoagulants, anti-depressants, cardiovascular drugs and anticancer drugs” (2011). Lack of Communication Many patients are hesitant to share with their primary care provider (pcp) that they use herbal supplements. These patients may fear that the pcp will disapprove of the use and thus do not disclose the information or they are never asked in the first place. In a study of Hispanic women, 60% reported never being asked about supplement use and 40% never volunteered the information with another survey indicating that 72% of all patients did not report supplement use with two thirds of those having chronic illness requiring conventional medicine (Ventola, 2011). This is troubling because those with chronic illnesses are more likely to take multiple 5 THE NURSE IN COMPLEMENTARY AND ALTERNATIVE MEDICINE conventional medicines leading one to infer that those who take herbal medicine and conventional medicine are at a greater risk of supplement and drug interactions. If patients are not willing to volunteer information about herbal medicine out of fear of disapproval or a belief that herbal is synonymous with natural and natural is synonymous with safe, the health care industry has an ethical duty to ask every patient about herbal supplement use in an effort to keep patients safe. The Role of the Nurse As a patient advocate and the member of the health care team who may have the initial and most frequent contact with the patient, the nurse has the greatest opportunity to ascertain information about herbal supplement use and hence can be involved in educating the patient about potential adverse reactions. Optimally this would be done during a patient admission assessment in a hospital setting, but could also occur in the physician’s office or public health department. While in the hospital there are other opportunities to inquire about supplement use during routine medication administration and at discharge. A patient being sent home on Coumadin for the first time may have neglected to share herbal supplement use upon admission and if not asked about the use may go home and return to taking the herbal supplements along with the Coumadin. to the ethical principal of Nonmaleficence can be defined as “the duty to do no harm” (Chitty & Black, 2011, p. 109). Failing to obtain a full medication list including herbal supplements could bring harm to the patient and thus is an ethical responsibility of the nurse. Cultural Considerations Nurses encounter patients from multiple cultural backgrounds. From Native Americans to first generation immigrants, America is a multi-cultural country with populations that may use herbal remedies as traditional medicine because that is what has always been done in a native 6 THE NURSE IN COMPLEMENTARY AND ALTERNATIVE MEDICINE culture (Ventola, 2011). In the same manner that nurses must be sensitive to transcultural differences in patients, special consideration may need to be given to different ethnic groups who that traditional herbal medicine from a particular culture. When language may already be a barrier in these instances, the nurse must make a thorough assessment of medication and herbal supplement use in order to avoid adverse supplement and drug interactions during hospitalization and in the patient’s home. Acceptance of Use According to Ventola, orthodox medicine practitioners have historically denounced the use of alternative and complementary therapies despite the fact that many current conventional medications are derived from plants. For example Quinine, which is the only treatment for malaria was derived from unconventional treatments (2011). “With support from the federal government, medical and nursing schools are incorporating lessons about CAM and dietary supplements into the education and training of physicians and nurses” (2011, Ventola). Code of Ethics In reference to the Code of Ethics for nurses (ANA, 2001), the nurse assists healthcare consumers in informed decision making. Obtaining information concerning herbal supplement use is the ethical responsibility of the nurse in order to educate the patient and the patient’s family about what may be unsafe practice for the patient. While alternative medicine has not made its way completely into acceptance on the part of conventional medicine, the health care consumers are clearly using herbal medicines as evidenced by yearly expenditures of 14.8 billion dollars (Ventola, 2011). While it may take time for physicians and nurses to become completely educated about herbal medicines, the nurse can assist patients and keep them informed of potential interactions simply by asking “Do you use any herbal supplements?” Clearly this 7 THE NURSE IN COMPLEMENTARY AND ALTERNATIVE MEDICINE information is not being asked and utilized on a routine basis, and healthcare practitioners owe it to their patients to inform them of risks. The risk of adverse reactions is much greater if the topic is not broached. Conclusion Alternative and Complementary medicine use is on the rise. Patients may not share the fact that they consume herbal medicines with their primary care provider for a variety of reasons. Regardless of the reasons, there are still risks associated with the concurrent use of herbal medicines with conventional medicines. If patients are not willing to share the information voluntarily, they need to be asked about the use of herbal supplements. As a patient advocate, the nurse is in an optimal position to inquire about herbal supplement use during their multiple interactions with families. Patients who may mistakenly believe that herbal is the same as natural and therefore harmless need to be educated about the use of these products. The nurse identifies learning needs based on nursing knowledge, the various roles the nurse may assume, and the changing needs of the population (ANA, 2010). As herbal product use is on the rise, so are the educational needs of the patient population and nursing on this topic. 8 THE NURSE IN COMPLEMENTARY AND ALTERNATIVE MEDICINE References ANA, (2010). Nursing: Scope and Standards of Practice (2nd ed.). Silver Spring, Maryland: Author Chitty, K.K., & Black, B.P. (2011). Professional nursing: concepts and challenges (6th ed.). Maryland Heights Missouri: Saunders Elsevier Egede, L.E., & Bais, S.S. (2011). BMC Complementary Alternative Medicine Dec 30 11(18). Department of Medicine, Medical University of South Carolina, Charlotte, South Carolina. Retrieved from PubMed Pender, N., Parsons, M., & Murdaugh, C. (2011). Health promotion in nursing practice (6th ed.). Upper Saddle River, New Jersey Ventola, C.L., (2010). Current Issues Regarding Complementary and Alternative Medicine in the United States. Pharmacy and Therapeutics P.T. 35 (8), 461-468. Retrieved from Cinhal Zhang, A.L., Fong, H.H.S., & Changli, X.C. (2011). Integration of herbal medicine into evidence based clinical practice: Current status and issues. Herbal Medicine: Biomolecular & Clinical Aspects (2nd ed.). Boca Raton, Florida: CRC Press