Chapter 17: Cardiovascular Emergencies
advertisement

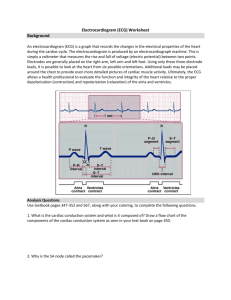
Chapter 17: Ready for Review • Cardiovascular disease has been the number one killer in the United States almost every year since 1900. • The cardiovascular system is composed of the heart and blood vessels. Its primary function is to deliver oxygenated blood and nutrients to every cell. • The body attempts to maintain a fairly constant blood pressure to ensure perfusion of vital organs. • Patients experience a variety of symptoms when they have a cardiovascular problem, the most common of which are chest pain, dyspnea, fainting, palpitations, and fatigue. • Patients with cardiovascular disease are often prescribed several medications. Patients with advanced age typically experience more side effects from medications than do younger patients. Adverse drug events account for approximately 10% of all ED visits in the elderly. • Cardiac rhythm disturbances (dysrhythmias) may arise from a variety of causes, including AMI. • One of the most important tasks in the prehospital care of a patient with an AMI is to anticipate, recognize, and treat life-threatening dysrhythmias. In fact, ECG analysis is indicated in any patient who might have a cardiac-related condition. • Most deaths from AMI are due to dysrhythmias, which typically occur during the early hours of the infarct. • Cardiac monitors consist of leads that are connected to electrodes, which are placed on the patient. Each lead offers an electrical snapshot of a certain part of the heart. The cardiac monitor records the electrical activity acquired by each lead used, resulting in a 12-lead ECG tracing. • Cardiac monitoring and ECG analysis are indicated in any patient who might have a cardiac-related condition. Any patient with chest pain or a history of heart problems should undergo ECG analysis. • Cardiac monitoring usually involves using four limb leads to create an ECG printout showing lead I, II, and III to monitor the electrical activity in the patient’s heart. • Components of a rhythm strip produced by an ECG include the P wave, PR interval, QRS complex, J point, ST segment, T wave, and QT interval. • Each component of the rhythm strip represents a phase of electrical activity within the heart. One whole complex on a rhythm strip represents one complete cycle of electrical conduction. • Items to assess when you are analyzing a rhythm strip or ECG include the following: P waves, the PR interval, QRS duration, rhythm, and rate. • The 12-lead ECG enables localization of cardiac ischemia to specific areas of the heart. The 12 leads include three limb leads (I, II, and III), three augmented limb leads (aVR, aVL, and aVF), and six precordial leads (V1 to V6). • Leads that look at the same general area of the heart are called contiguous leads. • Transmission of 12-lead ECG findings to the receiving facility is an important step that can lead to a faster diagnosis, decrease the time from emergency onset to definitive therapy (door-to-balloon time and door-to-needle time), and decrease mortality. • Management of cardiac arrest involves BLS and ALS skills, including CPR, defibrillation, • • • • • • • • • • cardiac monitoring, IV fluid or medication infusion, post-resuscitative care, and cooling. Defibrillation is an intervention used to interrupt rapid chaotic rhythms such as ventricular tachycardia and ventricular fibrillation. Defibrillation simultaneously depolarizes all cardiac tissue in hopes of allowing the SA node to resume the function of primary pacemaker. Paramedics most often perform manual defibrillation rather than automated external defibrillation, because they are trained in interpreting cardiac rhythms. Synchronized cardioversion is an intervention used to interrupt rapid, organized, and hemodynamically unstable rhythms such as supraventricular tachycardia and atrial fibrillation. Unlike defibrillation, synchronized cardioversion is timed or “synchronized” to the patient’s cardiac rhythm. Energy is delivered precisely at the peak of the R wave to capitalize on the already depolarized state of the ventricles. The energy delivered during synchronized cardioversion is aimed at depolarizing any tissue that remains polarized in hopes that the SA node resumes the primary pacemaking function. Transcutaneous pacing is an intervention used to depolarize heart muscle using an external stimulus. Pads placed on the patient’s chest deliver electrical energy to the heart, causing muscle contraction. The external pacemaker serves as a bridge to permanent internal pacemaker implantation. Transcutaneous pacing is used to treat patients with hemodynamically unstable bradycardias. Treatment of hemodynamically unstable dysrhythmias should be centered on rate control of the dysrhythmia using electrical therapies. Most cardiac arrest victims have evidence of atherosclerosis or other underlying cardiac disease. However, cardiac arrest can also occur secondary to electrocution, submersion, and other types of trauma. Indeed, many cardiac arrest victims have no warning before the event occurs. Coronary artery disease is the most common form of heart disease and the leading cause of death in adults in the United States. Cardiac tamponade occurs when excessive fluid accumulates within the pericardium, limiting the heart’s ability to fully expand. This can reduce cardiac filling to the point that the heart is unable to circulate blood. Emergent pericardiocentesis is lifesaving in patients with cardiac tamponade and hemodynamic instability. Transport the patient to the closest emergency facility. Cardiogenic shock results from extensive injury to the myocardium and carries a high mortality rate. Transport the patient expeditiously to the hospital. Except for the correction of life-threatening dysrhythmias, there are no measures that can stabilize the condition of a patient in cardiogenic shock in the field. Aortic aneurysms—particularly acute dissecting aneurysms of the thoracic aorta and expanding or ruptured aneurysms of the abdominal aorta—are of greatest concern to the EMS responder. The most common chief complaint is sudden severe ripping or tearing pain in the chest or abdomen. Treatment of hypertensive emergencies includes slow, controlled lowering of the patient’s blood pressure. Management of elevated blood pressure should be reserved for the emergency department physician. Remember that systemic hypertension can be a result of increased intracranial pressure and is essential to maintain cerebral perfusion pressure.