PC-48 Code Blue - Team Equipment and Training
advertisement
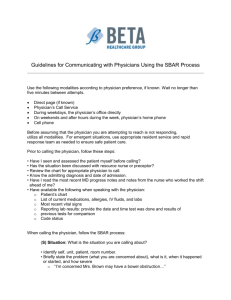
Subject: UH - Code Blue – Team, Equipment and Training Function: Provision of Care, Treatment and Services g and Business DevelopmentProP Applies To: Corporate UHC Number: PC-48.UH Revised: 2-19-13 MRC OBJECTIVE: To provide Emergency Life Support measures for all persons with Cardiac or Respiratory Arrest and/or an Obstructed Airway. POLICY: 1. There will be a designated Code Blue Team for all Adult Hospital Inpatient Units, Clinics physically based in the Hospital, Non-Patient Care Areas, Medical School, and School of Nursing to provide immediate response to persons requiring Cardiopulmonary Resuscitation. 2. Each clinic area not based on site at University Hospital must have the capability of responding to a Code Blue situation until an emergency team arrives. GENERAL INFORMATION: 1. Clinical Staff with ACLS Certification may initiate ACLS Protocols, within licensure, state regulations, and department policy until the Code Blue Team arrives. 2. Mouth-to-mouth resuscitation should be avoided if possible by using the pocket mask or hand resuscitator. 3. The Code Blue Team will be composed of the following staff designated to carry a Code Blue beeper at all times: A. Medicine Resident Physician B. Surgical Resident Physician C. Respiratory Therapist – Three D. Pharmacist when available (882-8601) E. House Manager or Designee F. An Emergency Department, ED, Registered Nurse for all areas that are not bedded UHC inpatient units. The ED will not need to respond to the Cath Lab. G. STAT Nurse H. An ICU Registered Nurse for UHC Inpatient Code Blue will act as Code Nurse, and will respond as follows when notified by beeper: 4. A Surgical Intensive Care Units Registered Nurse will cover A. All of the second floor CCA B. Diagnostic Center (GI Lab, Radiology, Pulmonary Function Lab, Sleep Lab, and Neurophysiology) C. Vascular Lab PC-48 Effective Date: 10-29-12 Page 1 of 10 D. Hyperbaric Center E. Missouri Orthopaedic Institute F. AIU (Ambulatory Infusion Unit (PCT2) 5. A Cardiac Intensive Care Unit Registered Nurse will cover A. 4 East B. 4 West C. Cardiac Cath Lab (including the EP lab) D. Dialysis 6. A Medical-Neurosurgical Intensive Care Unit Registered Nurse will cover A. 5-East B. 5-West C. 6-East D. 6-West E. Clinical Research Unit F. Progressive Care Unit (PCT5) 7. A Burn Intensive Care Unit Registered Nurse will cover A. 7-East B. 7-West C. Missouri Psychiatric Center, MUPC D. Neurosciences ICU (7PCT) E. Orthopedics (7PCT) F. Oncology (8PCT) 8. In the event the Code Blue is located on an UHC inpatient unit, the following persons in the Code Blue area will respond: A. The Clinical Supervisor or Charge Nurse of the involved inpatient unit. B. Two (2) Unit Based Nurses C. Unit Clerk if available 9. The following staff will respond as requested: A. An X-ray Technician B. IV Therapy Nurse 10. An Anesthesiology Physician will respond to a code when the Code Physician, Respiratory Therapist or Code Nurse requests assistance through activation of beeper 256-8200 (Resident) and beeper 256-8201 (Attending) with the call of Anesthesiology Respond To Code Blue at (Location) and phone number. 11. All inpatient units, and patient treatment areas and clinics, which provide moderate sedation are required to have a complete emergency cart. Patient treatment areas and clinics which do not administer moderate sedation may substitute Basic Life Support packs. RESPONSIBILITIES OF CODE BLUE TEAM ON INPATIENT UNITS: 1. The Code Physician will be responsible for the following phases of Code Management. A. Directions issued to Code Nurses, Respiratory Therapists, and assisting Physicians or Physician Assistants. PC-48 Effective Date: 10-29-12 Page 2 of 10 2. 3. 4. 5. 6. 7. B. Ordering and ensuring all procedures are completed including ET tube placement and confirmation of correct placement, IV placement, defibrillation, etc. C. Termination of Code and disposition of patient with the advice and consent of the attending physician or his/her physician designate, when available. D. Review and sign Code Blue Flow sheet Form prior to submission to Code Blue Committee. E. The Code Physician or his/her designee should contact the family regarding the events of the code. All other Physicians or Physician Assistants at the Code Scene will assist as directed by the Code Physician in the insertion of central or other venous access line, interpretation of rhythm or other monitoring functions, CPR or cardioversion, and any other tasks as directed by Code Physician. At the request from either the Code Physician, Respiratory Therapist, or Code Nurse, the Anesthesiology Physician will respond and accept responsibility for intubation of patient and documentation of intubation. Code Nurse or ICU Nurse Team Member will be responsible for the following: A. Assigning duties to nursing members of the Code Blue Team B. Assigning tasks as directed by Code Physician C. Restricting excess staff at the scene D. Notifying House Manager if ICU bed is needed E. Compliance with universal body fluid precautions F. Removal of excess furniture or equipment G. Arrange for notification of patient's family and support staff (Social Services, Chaplain, etc.). H. Maintain roommate privacy if in semi-private room I. Signing off on Code Blue Sheet. Nurse # 1 - (CPR) or Unit Nurse will be responsible for the following: A. Activating Code Response B. Initiating Basic Life Support (BLS) until Code Blue Team arrives C. Defibrillation, if ACLS Certified, as per Code Blue Physician orders D. Administering IV drugs per order of Code Physician. Nurse #2 - (Cart Nurse) or Unit Nurse will be responsible for the following: A. Bringing defibrillator and cart to Code Scene B. Preparing/distributing drugs per Code Nurse/Code Physician C. Accessing equipment/supplies from the emergency cart for the Code Blue Team. Nurse #3 - (Recorder Nurse) or Unit Clinical Supervisor or Charge Nurse will be responsible for the following: A. Documentation and recording of all Code Processes B. Assuring that Code Physician/Attending Physician and Code Nurse signs record after Code Blue has terminated C. Notifying Code Blue Team of elapsed time intervals, especially after medication administration D. Initiate Crash Cart Exchange process. PC-48 Effective Date: 10-29-12 Page 3 of 10 8. The Respiratory Therapy Team Members will be responsible for the following: A. Delivery and maintenance of oxygen supply B. Assisting with intubation and respiratory assessment, as requested by Anesthesiology or Code Physician. Respiratory Therapy may also perform the intubation if needed. C. Maintaining respiratory assistance equipment and patient ventilation D. Assisting with CPR until patient responds or is assisted mechanically, or until resuscitation activities are ceased by the Code Physician. E. Completion of the Respiratory Therapy Section of the Code Blue Review Form 9. The Unit Clerk will be responsible for the following: A. Directing the Code Blue Team to the Emergency scene. B. Keeping appropriate telephone lines open. C. Notify Telecommunications Operator of additional personnel requested by the Code Blue Team. D. Labeling and arranging for transport of STAT specimens with laboratory personnel. E. Obtain emergency equipment as needed. F. Obtain laboratory results and relay to the Code Blue Team. G. Notify Attending Physician of Code Blue. 10. The House Manager will be responsible for the following: A. Assessing and responding to the needs of Code Physician. B. May assume other roles as delegated by Code Nurse. C. If necessary, arrange for admission or transfer to ICU. PROCEDURES FOR CODE BLUE ON THE INPATIENT UNITS: 1. UHC Staff A. When discovering any person suffering from cardiac or respiratory arrest and/or obstructed airway activate the Code Blue light if available and call out "Code Blue" to alert the staff. Initiate CPR, note the time, and NEVER LEAVE THE PATIENT. 2. Unit Clerk or Clinic Staff A. Notify the Telecommunications operator at 882-7979 of the code blue, specify whether adult or pediatric, give the exact location, and remain at desk to direct the Code Blue Team to the scene. 3. Telecommunication A. Notify Code Blue Team members and House Manager via beeper of the location of the Code Blue Scene. 4. Code Blue Team A. One physician will declare himself or herself Code Physician. Normally this is the physician assigned to the Code Blue Team who arrives first. B. The physician who is designated Code Physician may change at any time there is mutual agreement between the two physicians. The purpose of this transition is to allow a smooth and rapid shift in management of Code Blue PC-48 Effective Date: 10-29-12 Page 4 of 10 C. D. E. F. situation from the Code Blue Team to a physician who normally cares for the patient and who is able and willing to assume the Code Physician role. The Attending Physician is the only person who may assume Code Control without mutual agreement from the designated Code Physician. The Code Physician will be in absolute control of the patient, all code mechanics, the orders and environment. The Code Physician will direct orders to respiratory therapy, assisting Physicians, and the designated Code Nurse. Orders given by other Physicians will not be carried out unless they are confirmed by the Code Physician. Procedures and Medications ordered by the Code Physician will be documented on the Code Blue Flow sheet, which will become official physician orders and remain a permanent part of the medical record. Code organization demands absolute authority of the Code Physician and Code Nurse over their respective teams. Conversation will be minimal and all input from Team Members will be directed to the Code Physician and Code Nurse. The Code Physician and Code Nurse will have the authority to remove excess staff from the scene and the responsibility to designate tasks and responsibilities inside of the Code Situation. RESPONSIBILITIES OF CODE BLUE TEAM IN ALL OTHER AREAS: NOTE: CPR Team members report to the Reception Desk to be escorted to the Code Blue site for Missouri Psychiatric Center (MUPC). Responsibilities are the same as in Inpatient Units with exception of the following: 1. The House Manager or Code Nurse will be responsible for the following: A. Assigning the Nursing Code Blue Team Members, delegating and relaying orders from The Code Physician B. Restricting excess staff C. Ensuring compliance with universal body fluid precautions D. Removing excess furniture E. Assuring that notification of patient's family and support personnel has occurred (Social Services, Chaplain, etc.) F. Documenting and recording all code processes and keeping Code Physician aware of sequencing and timing of drips, etc. G. Assuring that Code Physician/Attending Physician in charge signs record after Code Blue terminated. H. Filling out the Code Blue Review Form I. The House Manager will identify the ICU bed for further patient care 2. NURSE #1 - Emergency Center Nurse or Paramedic will be responsible for the following: A. Bringing the Defibrillator and Emergency Crash Cart and/or Code Blue Pack to Code-Scene B. Placing monitor on patient, initiate IV and assemble intubation equipment PC-48 Effective Date: 10-29-12 Page 5 of 10 C. Preparing and administering IV or ET drugs per order of Code Physician D. Monitoring the effectiveness of CPR E. Defibrillation, per order of Code Physician PROCEDURE OF CODE BLUE TEAM IN OTHER AREAS: NOTE: Clinics physically based in the Hospital, Non-Patient Care Areas, Diagnostic areas, MUPC, and the Medical School. Procedures are the same as in Inpatient Units with exception of the following: 1. Any Individual A. Upon discovery of anyone in cardiac or respiratory arrest or obstructed airway, call out "Code Blue" to alert staff in area - NEVER LEAVE THE PATIENT! Available qualified individuals should initiate CPR and use AED until team arrives. B. Notify operator at (882-7979) of the Code Blue emergency giving the exact location and specify adult or pediatric code. 2. Telecommunication Staff A. Page the Code Blue Team, and notify the team of the location of the Code Blue emergency. PROCEDURES OF CODE BLUE TEAM IN OFFSITE CLINICS: NOTE: Procedures in Offsite Clinic Areas are the same as in Inpatient Units with exception of the following: 1. Clinic Personnel A. The person identifying someone in medical distress will call "CODE BLUE" in order to obtain assistance and note the time. NEVER LEAVE THE PATIENT B. Provide notification immediately, by calling 911 for EMS response. State "Cardiac Arrest", give your exact location and specify whether a Pediatric or Adult Code. 2. Certified Personnel A. Initiate CPR immediately and use AED. 3. Registered or Licensed Practical Nurse A. Remain at location to assist with Physician's Orders and monitor the patient's condition. B. After Code Termination, document all care and all medications given for permanent record, and complete the Ancillary Service Request form for chargeable items. 4. Clinic Personnel A. Bring Basic Life Support Pack and AED or Crash Cart to "Code" location. B. Take family members to a private area, summon chaplain to be with them, and stand by to run errands. PC-48 Effective Date: 10-29-12 Page 6 of 10 PROCEDURES OF CODE BLUE TEAM IN SCHOOL OF NURSING 1. Any Individual A. The person identifying someone in medical distress will call “Code Blue” or “Help” in order to obtain assistance and note the time. NEVER LEAVE THE PATIENT. B. Notify EMS by calling 911, state “Cardiac Arrest” and give exact location. Identify whether the victim is an adult or pediatric victim. 2. Certified Personnel A. Initiate CPR immediately and use AED, if available. B. Assist EMS personnel as appropriate. C. Keep family/friends informed of activities. MAINTENANCE OF EMERGENCY CRASH CART CONTENTS AND BASIC LIFE SUPPORT PACKS: 1. Clinical Supervisor or Charge Nurse A. For areas that have standardized crash carts, initiate the crash cart exchange process following a Code Blue. B. For areas that have BLS packs, supplies and intubation equipment must be replaced and the packs resealed within one (1) hour after use. C. Crash Carts may be use for educational purposes. After the cart is used, the contents of the cart must be inventoried. A new lock is to be applied to the cart and lock number recorded on the Crash Cart checklist. The Crash Cart Exchange process is not used for this purpose. D. On a daily basis the following examinations must be carried out: 1. Ensure the Emergency Crash Cart is sealed and locked, then document on checklist. 2. Ensure the Emergency Drug Tray is sealed and locked, then document on checklist. 3. If Drug Tray is unlocked or expired, return to Pharmacy for replacement. 4. Ensure the Oxygen Cylinder contains greater than 500 lbs. of pressure of oxygen. 5. Zoll R Series defibrillators perform a daily self check at midnight. The defibrillator documents this check on an internal log. Verify a green check mark on front of defibrillator to indicate unit is properly functioning. 6. Zoll M Series defibrillators must be manually test-fired at 30 joules to verify proper functioning. 7. Automatic External Defibrillator (AED) – A. Ready Status for the FR2+/FR2 is a flashing hourglass. B. Ready Status for the Zoll AED Plus is a green check mark. C. Ready Status for the Zoll AED Pro is a green check mark. D. Ready Status for the Lifepak CR Plus is an OK on the front display. PC-48 Effective Date: 10-29-12 Page 7 of 10 E. Ready Status for the Cardiac Science is a green Rescue Ready Status indicator. 8. Verify that crash cart lock number matches the checklist. 9. Each Emergency Cart and its Emergency Drug Tray, or the Basic Life Support Pack, will be checked and documented at least once each day of business to assure that they are sealed and locked. 10. Once a month, sealed BLS Packs will be unsealed to be checked for outdates that will occur over the next 30 days. Any outdated supplies or equipment will be promptly replaced. 11. Check the Crash Cart expiration date daily and initiate Crash Cart Exchange process if indicated. 12. If the seal or lock is broken for any reason, the entire Cart/Pack must be rechecked for completeness and expiration dates. New seal or lock must be applied and recorded on checklist. 13. Crash Carts that are not on the Crash Cart Exchange Program A. Must have all equipment (e.g. laryngoscope, flashlight, doppler, etc.) tested on a monthly basis to verify function. B. Must have a complete audit of the Emergency Crash Cart on a monthly basis. 14. All licensed staff members will be familiar with the contents and location of the Crash Cart/Basic Life Support Packs/AED and Supplies. 15. Local or distant off-site clinics with a full Crash Cart, that are not on the Crash Cart Exchange Program, will need to keep a back-up Emergency Drug Box. This will replace a used Emergency Drug Box and continue an Emergency Drug supply while a new box is being supplied by Pharmacy Storeroom. 2. Clerical Staff A. Notify the departments for replacement of supplies (i.e. pharmacy and distribution). B. A checklist will be collected periodically by the Unit Managers to be filed for a period of 30 days. C. Notify Clinical Engineering for routine repair of equipment. If emergency or immediate repair is required, contact the on call Clinical Engineering Technician, the appropriate Unit Manager or the House Manager. MONITORING CODES: 1. Code Nurse, Code Physician and Respiratory Therapy A. The Code Blue Review Forms are filled out, reviewed by the Unit Educator (if applicable) and sent to the Clinical Outcomes Office (DC103.40) for preliminary review by the CPR Committee. TRAINING FOR CODE BLUE EMERGENCIES - ALL AREAS: PC-48 Effective Date: 10-29-12 Page 8 of 10 1. Hospital Administration A. Provide sufficient budget and space for training programs and qualified CPR and ACLS instructors. 2. Center for Education and Development A. Make provisions for newly employed direct patient care staff to become certified in BLS if not previously certified, and to recertify all direct patient care staff at least every two (2) years. B. Provide ACLS certification and recertification for all clinical staff mandated by Department guidelines for this training. 3. Hospital and Medical Staff Departments A. Provide appropriate CPR training for direct patient care staff. Provide ACLS for appropriate staff. 4. Anesthesia A. Assist in Respiratory Therapy personnel training on how to manage a patient's airway. REFERENCES: Key Content Expert: Chair, Provision of Care, Treatment and Services Approved: Signature available on original document James H. Ross, Chief Executive Officer University of Missouri Health Care PC-48 Effective Date: 10-29-12 10-29-12 Date Page 9 of 10 HYPERLINK TO : CRASH CART/BLS PACK CONTENTS/LOCATIONS PC-48 Effective Date: 10-29-12 Page 10 of 10