what is a mobile crisis team? - 1-800
advertisement

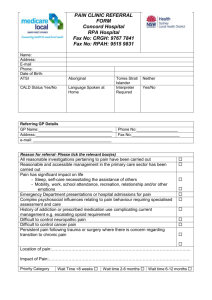
Referral Guide for Providers and Professionals: Mobile Crisis Teams 1-800-LIFENET LifeNet is a service of the Mental Health Association of New York City, Inc. in collaboration with The New York City Department of Health and Mental Hygiene. 50 Broadway, 19th Floor New York, NY 10004 www.800LifeNet.org Contents WHAT IS A MOBILE CRISIS TEAM? ........................................................................................................... 3 LIFENET MOBILE CRISIS REFERRAL CENTRAL ..................................................................................... 3 Who can request assistance from Mobile Crisis Teams? ............................................................................. 3 What services do Mobile Crisis Teams provide? .......................................................................................... 4 ENHANCED SERVICES FOR MOBILE CRISIS TEAMS ............................................................................. 5 Need Adapted Mobile Crisis Teams ............................................................................................................. 5 NA MCT Crisis Respite Centers.................................................................................................................... 5 Children’s Rapid Response Team ................................................................................................................ 5 Automatic Referral Group for MCT ............................................................................................................... 6 Mobile Crisis Team Referral Criteria ............................................................................................................. 6 Children’s Rapid Response Team Referral Criteria ...................................................................................... 7 Needs Adapted Mobile Crisis Team (Parachute NYC) Referral Criteria ...................................................... 7 HOW TO MAKE A PROVIDER FASTRACK MCT REFERRAL ................................................................... 8 Provider Fastrack Referral Process .......................................................................................................... 8 Hospital Discharge Planner Referrals ........................................................................................................... 8 ALTERNATE SOLUTIONS WHEN MCT IS NOT APPROPRIATE .............................................................. 9 FREQUENTLY ASKED QUESTIONS ........................................................................................................ 10 Service Cost ............................................................................................................................................ 10 Catchment ............................................................................................................................................... 10 Response Time ....................................................................................................................................... 10 Medication ............................................................................................................................................... 11 Anonymity................................................................................................................................................ 11 Current Treatment ................................................................................................................................... 11 Involuntary Psychiatric Evaluation .......................................................................................................... 11 PROVIDER REFERRAL FORM.................................................................................................................. 13 ...................................................................................................................... Error! Bookmark not defined. 2 WHAT IS A MOBILE CRISIS TEAM? A mobile crisis team is an interdisciplinary team of mental health professionals (e.g., nurses, social workers, psychiatrists, psychologists, mental health technicians, addiction specialists, peer counselors). Teams operate under the auspices of voluntary agencies and municipals hospitals. They respond to persons in the community, usually visiting them at home, although their mandate allows them to make contact at other locations. The Rapid Response Mobile Crisis Team for Children and Adolescents is a team of social workers and family advocates available to respond to youth specifically in the Bronx, Brooklyn and Queens community, including schools. Mobile Crisis Teams are also referred to as CPEP and Non-CPEP teams. The CPEP acronym stands for Comprehensive Psychiatric Emergency Program. A Non-CPEP team is defined under the guidelines of the aforementioned heading in our overview section titled: What is a Mobile Crisis Team? A CPEP team also known as: CPEP Crisis Outreach is a mobile crisis intervention component of the CPEP offering crisis outreach and interim crisis service visits to individuals outside an emergency room setting, in the community in natural (e.g. homes), structured (e.g., residential programs), or controlled (e.g., instructional) environments. Crisis outreach service visits are emergency mental health services provided outside an emergency room which include clinical assessment and crisis intervention treatment. Interim crisis service visits are mental health services provided to individuals who are released from a CPEP for the purpose of facilitating the individual’s community tenure while waiting for the first post-CPEP visit with a community-based mental health provider. CPEP crisis outreach and interim crisis service visits are Medicaid reimbursable. LIFENET MOBILE CRISIS REFERRAL CENTRAL LifeNet is New York City's only multicultural crisis center operating 24/7 with mental health professionals providing free behavioral health assessments, interventions, and support in English, Spanish, Cantonese, and Mandarin. LifeNet is the go-to source for New Yorkers seeking information and referrals to the vast and complex behavioral health treatment and social support services network. The New York City Department of Health and Mental Hygiene (NYCDOHMH) has mandated that as of January 14, 2013 all requests for a Mobile Crisis Team (MCT) in New York City that come from the community, i.e. family members, neighbors, friends, landlords, clergy, service providers to those who assist person(s) with a mental health issue, or other person(s) concerned about an individual, will begin with a call to the LifeNet (1-800-543-3638) hotline through the Mental Health Association. A LifeNet Crisis Counselor will then determine if the situation meets criteria for the services of a MCT. Who can request assistance from Mobile Crisis Teams? Mobile crisis teams serve any person in New York City who is experiencing, or is at risk of, a psychological crisis, and who requires mental health intervention and follow up support to overcome resistance to treatment. Family members, neighbors, friends, landlords, school personnel, clergy or other person(s) concerned about an individual often call mobile crisis teams in addition to concerned service providers 3 What services do Mobile Crisis Teams provide? Mobile Crisis Team staff provides a range of services including assessment, crisis intervention, supportive counseling, information and referrals, linkage with appropriate community based mental health services for ongoing treatment. Effective May 2013 all Mobile Crisis Team will provide Follow-Up Care: Follow-Up Care consists of mental health services provided to individuals who are released from an urgent level of care such as a Comprehensive Psychiatric Emergency Program (CPEP Emergency Room, Inpatient Unit), Medical Emergency Unit and or are being followed by a Psychiatric Discharge Monitoring Program (Koskinas) for the purpose of facilitating the individual’s community tenure while waiting for the first post-discharge visit with a community-based mental health provider. What if the Mobile Crisis Team determines that the individual in crisis needs to go to the hospital psychiatric emergency room for further evaluation? Teams will arrange to transport individuals to emergency rooms if further psychiatric and/or medical assessment and care is indicated. If the individual in crisis does not agree to go to the hospital willingly, and meets the specified legal standards (i.e., has a mental illness [or, in some instances appears to have a mental illness] and presents a danger to self or others), mobile crisis teams can direct the police to involuntarily transport such persons to the psychiatric emergency room for further evaluation and possible hospital admission. In most instances the police will direct the ambulance services operated by the City's Emergency Medical Services to provide actual transport. The Mobile Crisis Teams' authority to direct the involuntary removal of persons to the emergency room is provided by the NYS Mental Hygiene Law, Sections 9.37 and 9.58. What other kinds of services do Mobile Crisis Teams provide? In recent years, the Teams also have become an integral part of the Department of Health and Mental Hygiene’s disaster response network. They have conducted crisis counseling to victims in the aftermath of disasters, such as plane crashes, building collapses, major fires and explosions. Crisis Plan A Crisis Plan is a document that is developed to address actions that need to be taken in the event that the person is experiencing a behavioral health crisis. Psychiatric Advance Directives A Psychiatric Advance Directive (PAD) is a legal document written by a currently competent person who lives with a mental illness. It describes the person’s mental health treatment preferences, or names an agent to make treatment decisions for the individual, should he or she become unable to make such decisions due to psychiatric illness. There are two kinds of PADs: 4 Instructive PADs, in which an individual gives instructions about the specific mental health treatment desired should the individual experience a psychiatric crisis. Proxy PADs, in which the individual names a health care proxy or agent to make treatment decisions when the individual is unable to do so. ENHANCED SERVICES FOR MOBILE CRISIS TEAMS Need Adapted Mobile Crisis Teams (NAMCT) On February 15, 2013 NYC DOHMH began providing Need Adapted Mobile Crisis Team (NA-MCT) services: NA-MCTs are enhancements to existing Mobile Crisis Teams. The NAMCT’s are targeted to individuals who are experiencing an affective or non-affective psychosis related crisis or, for Brooklyn residents, are experiencing a first-episode of Severely Mentally Ill (SMI) category: Schizophrenia, Schizophreniform, Psychosis NOS, Schizoaffective Disorder, Bipolar Disorder and Major Depressive Disorder In addition to providing standard mobile crisis services, the NA-MCT will offer psychotherapy, peer support and family therapy as often as needed for up to one year for those people who are interested in and eligible for their services. In contrast with MCTs, NA-MCTs provide treatment, including medication, therapy and support. Therefore, if a person is already well engaged with treatment, they may not want to change their provider to the NA-MCT. However, if a person is tentatively or poorly engaged in treatment, they may find the NA-MCT model and approach more attractive and may wish to change providers. This decision is up to the person. Therefore, LIFENET need not consider a person’s current connection to treatment when making a referral. Each borough’s NAMCT varies slightly in its eligibility criteria. The NAMCT is trained in the Need Adapted Treatment Model (NATM) and Intentional Peer Support (IPS). They use peer specialists in tandem with behavioral health professionals to work with people and their family of choice in their home and/or community to develop trustful relationships and support networks that will help the person get through the current crisis, manage future crises and move towards recovery. NA MCT Crisis Respite Centers All Need Adapted Mobile Crisis Teams provide Respite Centers – LifeNet can provide caller with the phone number to the Respite Center. The Respite Center will screen the client for intake to the Center. o Residents of Staten Island can use Manhattan & Brooklyn Respite Center as there is currently no Respite / NA-MCT in the borough of Staten Island. Children’s Rapid Response Team 5 Children’s Rapid Response Teams provide rapid response and short term crisis management for children and adolescents in active crisis situations. To meet the criteria for the Children’s Rapid Response Teams, the child’s presenting problem should be acute rather than an ongoing concern. Some examples that would be considered are a recent change in functioning or behavior, out of character sadness, current suicidal ideation, or destructive/aggressive behavior within the last two days. Children’s Teams respond to school or home in the Bronx, Brooklyn and Queens. Teams provide crisis de-escalation, psychosocial assessment, initial prevention planning and collaboration with educators. Children’s Teams also provide support to families and caregivers by providing appropriate referrals, literature and education about how to prevent future crisis situations. Teams respond to the school or home within 2 hours of receiving the referral from LifeNet and are available 24 hours a day, 7 days a week. During non-business hours, the team will respond via phone call. Automatic Referral Group for MCT The Automatic Referral Group (ARG) is a group of providers who practice at urgent levels of care. Due to the nature of the services they provide, these levels of care are eligible for MCT referrals regardless of whether or not they meet the standard criteria. Comprehensive Psychiatric Emergency Programs (CPEP) Medical and Psychiatric Emergency Rooms Non-CPEP Mobile Crisis Teams CPEP Mobile Crisis Teams Inpatient Psychiatric Units Bellevue and St Luke’s Crisis Clinics Psychiatric Discharge monitoring Programs, Koskinas (HHC) Human Resources Administration (HRA) Visiting Psychiatrist Program Collyer’s Mansion type referrals from NYPD or FDNY Department of Homeless Services (DHS) for shelter or DHS Housed clients Mobile Crisis Team Referral Criteria Referral Criteria for MCT: The client or caller is experiencing or is at risk of experiencing a psychiatric or psychological crisis requiring mental health intervention and The client is currently not engaged in mental health treatment and is unwilling or unable to seek psychiatric services on his/her own or with the aid of a family member or friend or o The client has been discharged from an urgent level of care such as a Comprehensive Psychiatric Emergency Program (CPEP Emergency Room, Inpatient Unit), Medical Emergency Unit and or are being followed by a Psychiatric Discharge Monitoring Program (Koskinas) and requires mobile crisis services for the purpose of facilitating the individual’s community tenure while waiting for the first post-discharge visit with a community-based mental health provider. And the case does not qualify as being at “immediate risk” that would require an EMS referral. The client is experiencing or is at risk of experiencing a psychiatric or psychological crisis requiring mental health intervention and is currently non-compliant with mental health treatment and is unwilling or unable to continue obtaining psychiatric services on his/her own or with the aid of a family member or friend And the case does not qualify as being at “immediate risk” that would require an EMS referral. 6 Children’s Rapid Response Team Referral Criteria Referral Criteria for Children’s Rapid Response Team: Children ages birth through just prior to 17.11 months Child or adolescent must be experiencing a behavioral or mental health issue: o o o o o o Behaving in threatening manner: Experiencing a current psychiatric crisis Displaying active symptoms of depression Suspected of drug abuse with above situations Suspected of being bullied or perpetrator of bullying Experiencing, or is at risk of, a psychological crisis Reside in the assigned Community Districts in the Bronx, Brooklyn or Queens o Bronx Children Rapid Response: Responds to entire Bronx Community & every public school in Bronx, NY (Charter schools as well). o Brooklyn & Queens: Child must reside in the Community District or the Public School must be within the assigned Community District o Manhattan Child must reside in the Community District o Staten Island (Coming soon) Child can be already connected to mental health services Verbal or written parental consent If provider wants Team to visit a school, the school must call in the referral to give consent for Team to enter their building and provide intervention. Need Adapted Mobile Crisis Team (Parachute NYC) Referral Criteria REFERRAL CRITERIA FOR NEEDS ADAPTED MCT: 7 Experiencing a psychosis-related crisis (affective or non-affective) o For Parachute NYC Brooklyn – (Not available in Brooklyn at this time) o For Parachute NYC Bronx – The client must be 18-65 years old o For Parachute NYC Manhattan – The client must be 18-65 years old o For Parachute NYC Queens – The client must be 18-64 years old. Resident of Borough that NA-MCT is located (Manhattan, Queens, Bronx) Voluntarily seeks or accepts services (LifeNet can still make referrals for clients who are unwilling and consent will be established by NA-MCT) Has permanent housing (not homeless) Is able to have a family member (including close friend) engage in treatment with them. Medically stable, not have Dementia, Traumatic Brain Injury (TBI) or Organic Brain Disorder * NOTE: Though the client may not be eligible for NA MCT, they may still be eligible to make use of Respite Center’s. HOW TO MAKE A PROVIDER FASTRACK MCT REFERRAL Provider Fastrack Referral Process Provider Fastrack MCT referrals will ONLY be reviewed when received Mon- Fri 9am4:30pm. Outside of these hours, call 1800LIFENET to make an MCT referral. Provider Fastrack MCT referrals must be typed into the provided fillable form. The MCT Worksheet can be found on the MHA website. http://www.mhaofnyc.org/crisishotlines/ Fastrack is available Monday- Friday 9am-4:30pm. Fastrack is NOT available weekends and Holidays* Call 1-800LifeNet outside these hours to make a MCT referral. Fully complete all requested information in the fillable MCT Worksheet form. Fax referral to 1 646 514 9310 All referrals are pending until reviewed and approved by LifeNet You or your designee must be available to answer any questions LifeNet may have within 1 hour of transmitting your fax IF your referral is incomplete, LifeNet staff will contact you and let you know what is missing. You will be asked to update the MCT Worksheet and refax to LifeNet. If referral is accepted, LifeNet will contact you within 1 hour to provide the name and details of the MCT If the referral is declined, LifeNet staff will contact you within 1 hour to discuss alternatives Please email Gail Bower, LMSW GBower@mhaofnyc.org and Lynn Kaplan, Psy.D. LKaplan@mhaofnyc.org if you have not heard back from LifeNet within an hour to make sure that your fax was received. Holidays include New Year’s Day, President’s Day, Dr Martin Luther King Jr Day, Memorial Day, July 4th, Labor Day, Columbus Day, Veteran’s Day, Thanksgiving Day, Day after Thanksgiving, Christmas Day. For Holidays falling on weekend days, Fastrack will be closed on the Holiday’s observance day. (Cal 1-800 LifeNet for MCT on these days) Hospital Discharge Planner Referrals IF YOU ARE A DISCHARGE PLANNER CALLING FROM THE HOSPITAL FOR PURPOSES OF REFERRING A CONSUMER TO THE PARACHUTE NYC NA-MCT PROGRAM: 8 Please note that we will give you the direct number to the appropriate NA-MCT; LifeNet will not be doing the referral. The NA-MCT will speak with you and determine appropriateness of referral, and will follow through as needed. ALTERNATE SOLUTIONS WHEN MCT IS NOT APPROPRIATE THE FOLLOWING PROVIDER REFERRALS WILL NOT BE ACCEPTED BY LIFENET. ALTERNATIVES WILL BE PROVIDED TO THE CALLERS. REFERRALS NOT MEETING MCT ACCEPTANCE CRITERIA/ LIFENET ALTERNATE SOLUTIONS Psychiatric evaluation only Referral source cannot locate client The LifeNet Crisis Counselor can provide suggestions or alternatives on clinics to contact. If the caller is in crisis; LifeNet will conduct crisis counseling and risk assessment. If the caller is calling for a Psychiatric Evaluation LifeNet will recommend to caller to call a psychiatrist through their insurance or an outpatient clinic. MCTs are not designed to provide client locater services. Callers will be advised to call in a missing persons report. Case management needs (not at risk; If the referral source indicates that client is not at risk but needs to be linked to case linkage to treatment only) management services, LifeNet will provide referrals for case management programs. Client needs prescription LifeNet will encourage the caller to go to their nearest psychiatric ER if they are about to run out of medications. If caller/client does not have health insurance, LifeNet will encourage caller to go to a HHC (Health and Hospital Corporation) hospital where they can receive services regardless of insurance status. Client cannot get an appointment 9 This may be due to significant waiting lists at clinics. Teams are not capable of bypassing a clinic’s waiting list. Where possible, LifeNet Crisis Counselor will provide caller with information for clinics with walk in times. Chronic problems – not mental health LifeNet Crisis Counselor will provide appropriate referrals (ex: rehabilitation) related FREQUENTLY ASKED QUESTIONS Service Cost Most MCT services are free, however there are MCT’s who do bill clients for their services. Most of these are the teams associated with the Comprehensive Psychiatric Emergency Program (CPEP). The teams that do bill for their services will be indicated in their respective team profile. The teams will bill Medicaid, the client’s insurance company, or the client. In most instances, if the client does not have health coverage, collection is not enforced. If Medicaid, Medicare, or private insurance covers the client, obtain appropriate member #’s and names of companies and submit it to the MCT with the referral information. If a client expressed financial concerns, let them know the team will always work something out, and they must visit regardless of a person’s ability to pay. Catchment While each MCT is assigned to a specific catchment area, there are several MCTs whose catchment areas overlap. Deciding on which team to refer the caller will depend on their specific needs. Each MCT should be evaluated in terms of: 1. The team's hours - if one of the teams works weekends and the referral comes in on a Thursday or Friday, this team should be selected 2. Languages served 3. If the client is geriatric, a child/adolescent, or Orthodox Jewish community there are teams that specialize in those populations. There are instances when a team’s catchment area is the whole borough and other times where MCTs cover neighborhoods in the exact same borough. There are also teams whose catchment areas overlap. While at first this seems confusing, it can actually work to both the team’s and client’s advantage. A team that has a smaller catchment area will probably be less burdened and be able to more efficiently serve the client. It is a good habit to cross check the client’s CD against all the MCTs catchment areas in the borough. Response Time Effective January 2014 all mobile crisis teams (CPEP & Non-CPEP) are required to respond to referrals within 24-48 hours *(For differences in CPEP & Non CPEP teams please refer to pg. 1 – What is a Mobile Crisis Team). Where they are available, the Rapid Response Mobile Crisis Team for Children and Adolescents responds to calls within 2 hours of receiving a crisis referral from LIFENET. Consent and involvement from the minor’s family is an important component of the crisis service. MCTs visits are dependent on both the client’s and their own availability. Most teams do not call prior to making a visit but may accommodate requests to do so. The team might attempt to schedule an appointment with the 10 client, but often they make an unscheduled visit, especially if they cannot reach the client by phone. Realize that they are attempting to see clients who are unable/ unwilling to participate in treatment, so they don’t often call and ask if they can come. If a referral source asks that the team schedule an appointment, or would like to be present to help facilitate the referral, you must include this in your documentation. The team will do their best to accommodate, but we cannot promise this to the referral source. We cannot request that an MCT hold off on making a visit. They are a crisis service and are mandated to take action – not wait until a later time. Medication Each team handles the issue of medication differently. Some teams will distribute medication (possibly samples) while others provide prescriptions only. Many of the teams that are connected to hospitals will allow the client to fill the prescription at the hospital for a low fee. The best way to accurately inform a client about getting medication from a team is to tell them, “Each team deals with the issue of medication differently. They will come and talk to you about how you are feeling, and what your treatment options are. I will include your medication history in my referral, and they will be prepared to discuss that with you”. Anonymity The caller/ referral source cannot remain anonymous. There have been rare occasions where someone (a neighbor, friend, family member) has requested that the client not be told that they made the referral. The MCT has to be able to make the client aware of who called the team. It is unfair to the team if they show up at the client’s home, and are unable to state the purpose of their visit. The client also has a right to know who has phoned the team on their behalf. If the caller has concerns about their identity being revealed to the client, let them know you can make the referral, and they can discuss their concerns with the team, prior to their making a visit. The caller can withdraw the referral before the visit, if they change their mind after speaking to the team. Be sure to include these concerns in your referral, but do not promise the caller that their anonymity can be protected, that is not the case. Current Treatment Current treatment status does not define eligibility for MCT services; Presenting Problem should determine need for said services. If a caller, however, indicates that they have not been maintaining appointments a referral may be appropriate and this should be indicated clearly in your call documentation. If you receive an indirect call from, for example, a parent or friend of someone in possible need of an MCT referral, this individual must contact the treatment provider first regarding their concerns. If this has already been attempted with little resolution an MCT referral may be appropriate. Again this must be clearly indicated in the call documentation. Involuntary Psychiatric Evaluation The Mobile Crisis Teams' authority to direct the involuntary removal of persons to the emergency room is provided by Article 9 of the New York State Mental Hygiene Law (NYS MHL). Article 9 contains several sections that govern the decision by clinicians and police/peace officers to involuntarily remove individuals. The law defines the standards that must be met, as well as who is authorized to take such 11 action. Below are brief descriptions of relevant sections. Mobile Crisis Teams typically operate under sections 9.37 and 9.58. Section 9.45: A Section 9.45 removal order is issued by the Department's Commissioner directing the police to transport an individual to the emergency room when a treating clinician is able to demonstrate that this individual has a mental illness and presents a danger to self or others. Department guidelines require that a qualified clinical reporter (licensed M.D. or licensed psychologist, registered nurse or certified social worker treating the individual) provide the Office of Crisis Intervention Services with all the necessary information needed to establish that the client is mentally ill and presents a danger to self or others. Requesting a 9.45 order is not appropriate if the client is an immediate danger to self or others. In such cases, Department guidelines direct the clinician to call "911". Section 9.37: The Department Commissioner is empowered to designate board-certified psychiatrists who are part of mobile crisis teams, or who work in other key emergency arenas, to order the involuntary removal to a psychiatric emergency room of an individual who has a mental illness and presents a danger to self or others. The 9.37 designation is not available for emergency room doctors. Section 9.58: Section 9.58 of the State mental hygiene law was enacted in 1995. It extends the authority to order the involuntary removal of an individual to the psychiatric emergency room to specified staff (i.e., M.D.s, licensed psychologists, registered nurses and certified social workers) who are part of approved mental health mobile crisis teams, ACT and Homeless Outreach teams. The individual subject to involuntary removal must appear to have a mental illness and present a danger to self or others. In New York City, all 9.58 eligible mobile crisis workers must complete a special training sequence developed by the Department before they can receive the 9.58 designation. 9.58 provide an alternative to the 9.45 and 9.37 orders. Section 9.43: A 9.43 involuntary removal order is a civil order issued by a judge when he or she is presented with evidence that an individual has, or may have, a mental illness, and presents a danger to self or others (often referred to as a Mental Hygiene Warrant). A 9.43 order may be requested by a treating clinician or family member. A 9.43 order also can be issued by a judge in criminal cases when the individual appearing before the judge appears to have a mental illness and presents a danger to self or others, and the court determines either that the crime has not been committed or that there is not sufficient cause to believe that such a person is guilty of the crime. 12 PROVIDER REFERRAL FORM 13 14 15 16