lt23788-sup-0001
advertisement

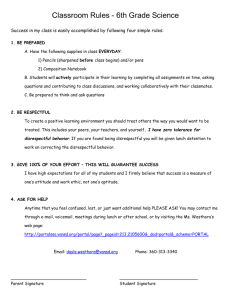
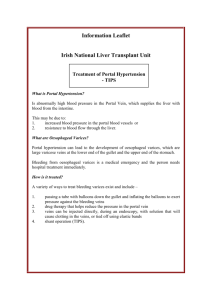
AMR was the probable primary cause of allograft loss Case 1 (Figure 1) A 56 year-old female (with a gynecologic history significant for one stillbirth) with a MELD of 12 underwent a primary liver transplant (LT) for autoimmune hepatitis with a 37 year-old male donor after 12.2 hours of cold ischemia in 1990. She had 7 distinct preformed DSAs present: 5 class I and 2 class II with an MFIsum of 115,791. Further evaluation showed bead saturation of all 4 class I DSAs at 1:81 dilution. Four of the 5 class I DSAs were of multiple IgG subclasses and IgG3 was present in 2. C1q was strongly positive in the 4 class I DSAs showing bead saturation and weakly positive in the other class I DSA. The post-reperfusion biopsy contained portal tracts with a mixed inflammatory infiltrate, edema, and neutrophils cuffing the bile ducts with a lowgrade ductular reaction. The C4d stain showed diffuse microvascular endothelial staining in the portal tracts, periportal sinusoids and central veins. Preoperatively the patient’s platelets were 127,000/uL, 2 units of platelets were administered in the operating room, yet they declined to 54,000/uL on post-operative day (POD) 3. Six liver biopsies were performed for persistently abnormal liver function tests, the POD16 biopsy showed combined AMR and ACR. The pre-explant indication liver biopsy on POD29 showed sinusoidal dilatation, atrophy, and congestion as well as portal edema, injured and senescent-appearing bile ducts. The corresponding C4d appeared similar to the post-perfusion biopsy with diffuse microvascular endothelial cell staining in the portal tracts with slightly less diffuse sinusoidal staining and no central vein staining. However, despite 2 steroid recycles, prednisolone doses no less than 20 mg/day, and treatment in the tacrolimus study (total dose per day of 10-20 mg) her liver tests progressively worsened, she developed ascites, and expired from a cardiac arrest on POD40. Case 2 (Figure 2) A 47 year-old primiparous female with a MELD of 40 underwent a primary LT for alcohol-induced cirrhosis with a 45 year-old female donor after 7.6 hours of cold ischemia in 2005. She had 8 distinct preformed DSAs present: 4 class I and 4 class II with an MFIsum of 131,596. Further evaluation showed bead saturation of 4 DSAs (2 class I and 2 class II) at 1:81 dilution. Five DSAs were of multiple IgG subclasses and 6 had IgG3 present. C1q was strongly positive in 5 DSAs. The post-reperfusion liver biopsy displayed mild mixed portal inflammation, some of which may have come from the donor, and a low-grade ductular reaction. The lobule contained about 40% macrovesicular steatosis with large coalescent fat globules, indicative of donor steatosis, with nearby fibrin deposition and neutrophilia. The C4d stain was focally positive in endothelial cells lining the portal microvasculature, including inlet venules. Preoperatively platelets were 55,000/uL, but despite receiving 8 units of platelets over the first 6 days declined to 11,000/uL on POD6. Re-review of the patient’s only indication liver biopsy on POD12 demonstrated active central perivenulitis, portal edema, ductular reaction, marked reactivity of the entire portal microvascular endothelia comprising enlarged rounded nuclei and abundant cytoplasm, and early scarring of the venous intima. Corresponding C4d stains showed diffuse portal microvascular staining. Although originally interpreted as acute cholangitis, an ERCP with stent placement was followed by a relentless increase in serum bilirubin, and a follow up percutaneous transhepatic cholangiogram on POD18 was normal. The patient’s immunosuppression included: solumedrol and Daclizumab on POD1 and 2 followed by OKT3 on POD 4-9 and 14-15, and renal failure led to cyclosporine initiation on POD17. Dialysis was performed preoperatively through POD8 and was re-initiated on POD16. Respiratory failure with ascites occurred on POD18, and she expired on POD21. Case 3 (Figure 3) A 58 year-old multiparous female with a MELD of 27 underwent primary LT for primary biliary cirrhosis with a 58 year-old male donor after 11.8 hours of cold ischemia in 2004. She had 5 distinct preformed DSAs: 3 class I and 2 class II with an MFIsum of 20,975. Further evaluation showed diminution of DSA over serial dilutions (no bead saturation). One class I and 2 class II DSAs were of a single IgG subclass without IgG3 or C1q. The post-reperfusion biopsy showed minimal to no portal inflammation and focal macrovesicular steatosis involving 20% of hepatocytes in an occasional lobule with negative C4d staining. Pre-operative platelets of 136,000/uL declined to 68,000/uL on POD3. Two indication liver biopsies for persistently abnormal liver function tests showed mild ACR on POD7, which was treated with a steroid recycle. Although rejection was not identified at the time, the second biopsy on POD11 was re-read as severe rejection with combined AMR and ACR based on mild mixed portal inflammation with eosinophils, a moderate ductular reaction, diffuse endothelial cell hypertrophy of the portal microvasculature, hemorrhage into the portal stroma, early vein scarring, and senescent-appearing bile ducts and diffuse C4d positivity in the portal tracts and central veins. Despite the original steroid recycle, prednisolone doses no less than 20 mg/day, treatment with tacrolimus (levels ranged from 7.4-23 ng/mL) and mycophenolate, her liver function tests progressively worsened. Renal failure ensued, and she expired on POD20. At autopsy, the liver allograft revealed evidence of a very aggressive combined AMR and ACR reaction, as evidenced by widespread coagulative necrosis with large foci of dystrophic calcification indicative of previous injury, acute cholangitis (although biliary obstruction was not found), endothelial lifting with sloughing of cells into the lumen with enlarged nuclei, active lymphocytic arteritis with intimal foam cells and vasospasm. Altogether, the combined AMR and ACR were strongly suggestive of a “recall” response in this sensitized multiparous female, although de novo antibodies cannot be absolutely excluded. DSA could not be ruled out as a contributor to allograft loss Case 4 A 52 year old male with a MELD of 16 received a 59 year-old female donor after 8.4 hours of cold ischemia that also showed 40% macrovesicular steatosis with active steatohepatitis, minimal portal inflammation, and negative C4d staining in the post-reperfusion biopsy. The pre-existing steatosis and steatohepatitis were felt to be the primary cause of allograft loss, but there were 4 distinct class I DSAs found with an MFIsum of 70,396, one of which displayed bead saturation at 1:81 dilution. Explant pathology showed minimal mixed portal inflammation, a low-grade ductular reaction, mild-moderate endothelial cell hypertrophy with focal endothelial denudation and platelet fibrin thrombi, and minimal C4d present in the portal capillaries. Case 5 A 40 year-old female with a MELD of 13 received a 56 year-old female donor liver after 7.8 hours of cold ischemia. Four distinct preformed DSAs were present: 3 class I and 1 class II with an MFIsum of 40,752. Further evaluation showed 1 DSA reached bead saturation at 1:81 dilution. The post-reperfusion biopsy had minimal mixed portal inflammation with a ductular reaction, marked Kupffer cell hypertrophy with focal platelet aggregates, but a negative C4d stain. Pre-operative platelet values of 128,000/uL decreased to 36,000/uL on POD4, whereas alanine aminotransferase and serum bilirubin inexplicably climbed over the 4 days preceding re-transplantation despite treatment with high dose steroids and tacrolimus. Explant histopathology showed marked portal neutrophilia, prominent ductular reaction, wide spread centrilobular necrosis without venulitis, and minimal endothelial reactivity indicative of severe ACR with a possible AMR component, although the C4d stain was negative. Case 6 A 55 year-old female with a MELD of 33 received a 55 year-old male donor after 8.7 hours of cold ischemia. A partially re-canalized hepatic artery thrombus was found on pathologic re-evaluation that was believed to be the primary cause of graft loss on POD54. However, 3 class I antibodies were found with an MFIsum of 39,691. Post–reperfusion liver biopsy showed minimal mixed portal inflammation with minimal arterial vasospasm and negative C4d staining. POD38 liver biopsy and explant tissue showed findings typical of hepatic artery thrombosis: centrilobular necrosis, bile infarcts, ductular reaction, and cholestasis. A C4d stain was negative, but in light of the negative C1q it is possible that antibodies contributed to the endothelial injury and arterial thrombosis.