Pathology Chapter 11p510-527 [4-20
advertisement

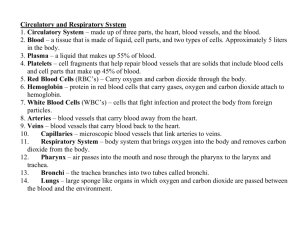
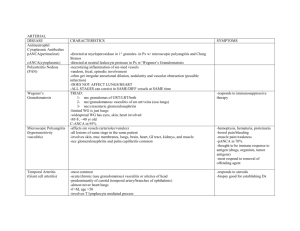
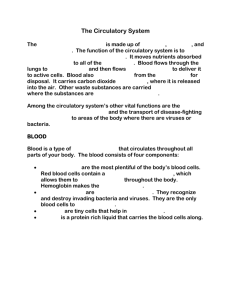
Pathology Chapter 11: Blood Vessels (pages 510-527) Vasculitis – vessel wall inflammation - - Vasculitides – vasculitis disorders Symptoms of vasculitis are usually constitutional symptoms like fever, myalgia, arthralgia, and malaise Any vessel can be affected Most vasculitides involve small vessels (arterioles, capillaries, venules) The most accepted way to classify vasculitis disorders is by vessel size – page 511-512 The 2 most common causes of vasculitis are immune caused inflammation and direct invasion of vascular walls by in microbes o Infections can also cause noninfectious vasculitis, where they don’t directly invade, and instead form immune complexes or through cross-reactivity o It’s important to know if it’s infection or immune inflammation caused, because immunosuppressives can be used for immune-mediated vasculitis, but could make worse infectious vasculitis o Trauma, toxins, and radiation can also cause vasculitis Noninfectious vasculitis: o The main immune causes of noninfectious vasculitis are immune complex deposition, antineutrophil cytoplasmic antibodies (ANCA), and antiendothelial cell antibodies o Immune complex-associated vasculitis: Looks similar to the arthus rxn Many systemic immune diseases, like lupus (SLE) and polyarteritis nodosa, manifest as immune complex-mediated vasculitis Antibodies and complement are usually found in vasculitis lesions Usually you have a hard time figuring out what the antigen is though Antigen-antibody complexes also circulate Drug hypersensitivity shows a vasculitis caused by immune complex deposition Some drugs are proteins, and others bind to our proteins Antibodies are then made against the drug-modified proteins or foreign molecules, lead to making of immune complexes The most common symptom is skin issues Removing the drug will get rid of the vasculitis Vasculitis caused by viral infections form immune complexes that circulate and deposit as lesions Ex: 1/3 of people with polyarteritis nodosa have underlying hepatitis B (HBV) - Pauci-immune – immune complex vasculitis where you don’t see many antigenantibody complexes, most likely cause they’ve already been cleared when you looked o Antineutrophil cytoplasmic antibodies (ANCAs) ANCAs bind to antigens in the cytoplasm of the neutrophil, mainly enzymes in neutrophil granules, monocyte lysosomes, and endothelial cells Anti-myeloperoxidase (MPO-ANCA) – antibodies that target myeloperoxidase (MPO), which is found in lysosomes and makes ROS (HOCl) MPO-ANCA are perinuclear antibodies (p-ANCA) MPO-ANCAs are characteristic of polyangitis & Churg-Strauss syndrome Anti-proteinase-3 (PR3-ANCA) – antibodies that target anti-proteinase-3 (PR3), which is found in azurophilic granules PR3-ANCA are cytoplasmic antibodies (c-ANCA) PR3-ANCAs are typically seen in Wegener granulomatosis ANCAs are indicators of an ANCA caused vasculitis, and how high they are corresponds to the degree of inflammation happening ANCAs can directly activate neutrophils causing them to release ROS and enzymes, leading to endothelial cell damage The targets of ANCAs are mainly intracellular, but you usually see the ANCAs in the cell membrane cause they can’t get into the cell How ANCA vasculitis happens: The ANCAs get formed – by drugs, or cross-reactive microbe antigens, or neutrophils either express on their surface or release PR3 and MPO Then infection, endotoxin exposure, or other inflammatory stimuli cause release of cytokines like TNF, that cause surface expression of PR3 and MPO on other neutrophils and other cell types ANCAs react with these cytokine-activated cells and either cause direct injury to endothelial cells, or induce more activation in neutrophils ANCA-activated neutrophils degranulate and also cause injury by releasing ROS, causing tissue injury Giant-cell (Temporal) arteritis – chronic, usually granulomatous inflammation of large-to-small sized arteries, that mainly affects arteries of the head, especially the temporal arteries o Temporal arteritis is the most common form of vasculitis in old people in the US o Giant cell arteritis in the ophthalmic artery can cause permanent blindness o So Giant-cell arteritis is a medical emergency o Reasons we think giant-cell arteritis is caused by the immune system: There is a characteristic granulomatous rxn HLA genes are involved It responds to steroids o The affected arteries develop thickening of the intima with nodules, that reduces the diameter of the lumen – page 513 o - Classic giant cell arteritis lesions show granulomatous inflammation of the media, that leads to elastic lamina fragmentation o Giant cell arteritis is extremely segmental, and there may be big areas of normal vessel along with it o There is an infiltrate of T cells and macrophage o ¾ of patients show multinucleated giant cells o Temporal arteritis is rare before age 50 o Symptoms of temporal arteritis are vague and constitutional – includes fever, fatigue, and weight loss More specific signs not always seen are facial pain or headache that is most intense along the course of the superficial temporal artery, which it hurts to touch o When the otphalmic artery is involved, it causes eye problems in half of patients Problems range anywhere from diplopia to complete vision loss o When doing a biopsy for giant cell arteritis, negative doesn’t rule it out because of how segmental the arteritis is o Giving them corticosteroids helps Takayasu arteritis – granulomatous vasculitis of medium and larger arteries, characterized by eye problems and very weak pulses in the upper extremities o Takayasu arteritis is sometimes aka “pulseless disease” o Takayasu arteritis manifests with transmural fibrous thickening of the aorta, especially at the aortic arch and great vessels, and severe lumen narrowing of the major branch vessels – page 514 o Takayasu arteritis looks a lot like giant cell arteritis in the aorta (aortitis), and the only main difference is age Giant cell aortitis happens in people over 50, while Takayasu aortitis happens in people under 50 o Takayasu arteritis can happen in any population, but is associated with Japanese people o The cause of Takayasu arteritis is unknown o Takayasu arteritis classically involves the aortic arch In 1/3 of patients it also affects the rest of the aorta and its branches The pulmonary artery is involved in half of cases o There is irregular thickening of the vessel wall with intima hyperplasia, which narrows the lumens and can even obliterate it This narrowing causes the weak peripheral pulses o On histo, Takayasu arteritis looks just like giant cell arteritis o As it progresses, you get collagenous scarring with inflammatory infiltrates in all 3 layers of the vessel wall o Initial symptoms of Takayasu arteritis are usually nonspecific, and include fatigue, weight loss, and fever As it progresses, you get vascular symptoms, like decreased blood pressure and weak pulses in the upper extremities - Can also have eye symptoms, like retinal hemorrhages and blindness, and neuro problems When the distal aorta is involved, it can cause claudication of the legs When the pulmonary artery is involved, it can cause pulmonary hypertension Narrowing of the coronary vessels can cause an MI Narrowing of the renal arteries can cause systemic hypertension o In some people, Takayasu arteritis progresses rapidly, while others have a quiescent stage of 1-2 years, allowing long-term survival along with visual and neuro problems Polyarteritis nodosa (PAN) – systemic vasculitis of small or medium sized muscular arteries, but not the arterioles, capillaries, or venules o Usually, polyarteritis nodosa involves the renal and visceral vessels, but spares pulmonary circulation o 1/3 of people with polyarteritis nodoa have chronic hepatitis B (HBV), with HBsAg-HbsIg complexes in the affected vessels, indicating immune complex problems o Symptoms result from ischemia and infarction of affected tissues o Classic polyarteritis nodosa is characterized by segmental transmural necrotizing inflammation of small to medium-sized arteries The most common vessels affected are the kidneys Polyarteritis nodosa lesions usually don’t affect the whole circumference of the vessel, and usually happen at branch points The inflammatory process weakens the artery wall, and can lead to aneurysms or rupture Can also see impaired perfusion that leads to ulcerations, infarcts, ischemic atrophy, or hemorrhages in tissues supplied by the affected vessels In the acute phase there is transmural inflammation of the artery wall, usually accompanied by fibrinoid necrosis – page 514 bottom right pic Later, the inflammatory infiltrate is replaced by fibrous thickening of the vessel wall Characteristically, all stages of polyarteritis nodosa are going on at the same time in different vessels or the same vessel o Polyarteritis nodosa is usually seen in young adults, but can happen at any age o Polyarteritis is usually episodic with episodes of symptoms and then it gets better, with long periods without symptoms o The most common symptoms of polyarteritis nodosa are malaise, fever, and weight loss, rapid hypertension from the kidney vessels being affected, abdominal pain and melena (blood in stool) from lesions in the GI, widespread muscle aches and pains, and peripheral neuritis o Renal artery involvement is often bad and can cause death o If untreated, polyarteritis nodosa is usually fatal Treating with corticosteroids and cyclophosphamide causes remissions or cures in most (90%) of cases - - Kawasaki disease – acute febrile, self-limited illness in kids (80% is in kids under 4) with an arteritis affecting all size vessels o Kawasaki disease is the leading cause of acquired heart disease in kids o Kawasaki disease tends to involve the coronary arteries, and coronary arteritis can cause aneurysms that rupture or thrombose, leading to acute MI o It’s thought to be caused by a delayed-type (type 4) hypersensitivity rxn of T cells This leads to cytokine making and macrophage activation, and B cells are activated to make autoantibodies to endothelial cells and smooth muscle cells, which make the acute vasculitis worse The type 4 rxn is thought to be triggered by a virus o There’s lots of inflammation on the entire thickness of the vessel wall, but unlike polyarteritis nodosa there isn’t as much fibriniod necrosis o Kawasaki disease is aka mucocutaneous lymph node syndrome, because it presents with conjunctival and oral erythema and erosion, edema of the hands and feet, erythema of the palms and soles, a rash, and cervical lymph node enlargement o 1/5 of untreated people get coronary vessel problems like aneurysm, which can rupture or thrombose, MI, and sudden death Giving them IV antibody therapy and aspirin, the rate of coronary artery disease is decreased to less than 4% Microscopic polyangitis (aka hypersensitivity or leukocytoclastic vasculitis) – necrotizing vasculitis that affects capillaries, arterioles, and venules that are smaller than those involved in polyarteritis nodosa o Unlike polyarteritis nodosa, all lesions of microscopic polyangitis tend to be in the same stage in the vessels o Microscopic polyangitis can affect the skin, mucous membranes, lungs, brain, heart, GI, kidneys, and muscle Necrotizing glomerulonephritis happens in most (90%) of patients and pulmonary capillaritis is also common o Microscopic polyangiitis lesions can also happen in other disorders, like HenochSchonlein purpura, essential mixed cryoglobulinemia, and vasculitis from connective tissue disorders o Some microscopic polyangitis have an antibody response to antigens like drugs (penicillin), microorganisms (strep), or tumor proteins These can either cause an immune complex deposition, or can trigger secondary immune responses, like development of ANCAs o Most cases though are pauci-immune, which means there are no immune complexes o Microscopic polyangiitis is characterized by segmental fibrinoid necrosis of the media with focal transmural necrotizing lesions They look like polyarteritis nodosa, but spare the medium and large arteries, so large infarcts aren’t common In some areas, all you see are infiltrating and fragmenting neutrophils, which is why it’s called leukocytoclastic vasculitis o - - - Major symptoms include hemoptysis, hematuria, proteinuria, bowel pain or bleeding, muscle pain or weakness, and cutaneous purpura o Cyclophosphamide and steroid immunosuppressants cause remission and improves long term survival Exception – in people with the kidneys or brain involved Churg-Strauss syndrome (aka allergic granulomatosis and angiitis) – rare small vessel necrotizing vasculitis classically associated with asthma, allergic rhinitis, lung infiltrates, increased eosinophils, and granulomas o Lesions characteristically include granulomas and eosinophils o Less than half of cases show ANCAs o The major symptoms are purpura, GI tract bleeding, and glomerulosclerosis o Cardiomyopathy happens in over half of patients, and causes about half of deaths in Churg-Strauss Wegener granulomatosis: o Wegener granulomatosis is a necrotizing vasculitis characterized by 3 things: Acute necrotizing granulomas of the upper respiratory tract (ear to throat) or lower respiratory tract (lung) or both Necrotizing or granulomatous vasculitis affecting small to medium sized vessels (capillaries, venules, arterioles, and arteries) mainly in the lungs & upper airway Necrotizing, crescentic glomerulonephritis o Wegener granulomatosis is a T cell mediated hypersensitivity rxn, probably from an inhaled agent o PR3-ANCAs are seen most (95%) of cases o Upper respiratory lesions can be inflammatory sinusitis with granulomas or ulcers of the nose, palate, or pharynx rimmed by granulomas with geographic patterns of central necrosis with vasculitis The necrotizing granulomas are surrounded by a zone of fibroblast proliferation with giant cells and WBCs There may be a lot of alveolar hemorrhage o Wegener granulomatosis affects guys more, usually around 40 years old o Classic features of Wegener granulomatosis are persistent pneumonitis with bilateral nodules and cavitary infiltrates, chronic sinusitis, ulcers of the nasopharynx mucoas, and kidney disease o Untreated Wegener granulomatosis is rapidly fatal, 4/5 die within a year o Treat with steroids, cyclophosphamide, and TNF-antagonists, which turn it inot a chronic remitting and relapsing disease Thromboangiitis obliterans (Buerger disease) – characterized by segmental, thrombosing inflammation of medium sized and small arteries, mainly the tibial and radial arteries o Thromboangiitis obliterans often leads to vascular insufficiency o Thromboangiitis obliterans happens almost entirely in heavy cigarette smokers, usually before age 35 The tobacco somehow injures the endothelial cells o o - - It’s more common in Israelis, Indians, and Japanese, and certain HLAs Thromboangiitis obliterans is characterized by a sharply segmental acute and chronic vasculitis of medium sized and small arteries, mainly of the extremities You see acute and chronic inflammation, accompanied by lumen thrombosis– page 517 The inflammation extends into nearby veins and nerves, and eventually the vessels and nerves all get encased in fibrous tissue o Early symptoms are superficial nodular phlebitis, Raynoud syndrome cold sensitivity in the hands, pain in the foot induced by exercise (called instep claudication) Unlike atherosclerosis, there’s severe pain, even at rest, due to neural involvement Chronic ulcerations of the toes, feet, or fingers, which can be followed by gangrene o If you stop smoking cigarettes during the early disease, it causes dramatic relief from further attacks Vasculitis resembling hypersensitivity angiitis or classic polyarteritis nodosa can sometimes be associated with other disorders, like rheumatoid arthritis, lupus, cancer, or systemic illness like mixed cryoglobulinemia, antiphospholipid syndrome, and Henoch-Schonlein purpura o Rheumatoid vasculitis happens after long-standing severe rheumatoid arthritis o Classic immune complex lupus vasculitis and antiphospholipid antibody syndrome look similar, but you treat lupus with anti-inflammatories, and antiphospholipid Ig with anticoagulants Infectious vasculitis can be caused by direct invasion of the infectious agent, usually bacteria or fungi, especially aspergillus and mucors o Vascular infections can weaken artery walls and lead to mycotic aneurysms, or can induce thrombosis and infarction o So inflammation-induced thrombosis of meningeal vessels in the bacterial meningitis can cause infarction of the underlying brain Raynaud phenomenon – happens form exaggerated vasoconstriction of digital arteries and arterioles, which causes a paroxysmal pallor or cyanosis of the digits of the hands or feet, and less often the nose, earlobes, or lips – page 518 - - Characteristically, the digits show 3 color changes the more distal you go: o Red – proximal vasodilation o White – central vasoconstriction o Blue – distal cyanosis Raynaud phenomenon can be a primary disease, or secondary to other stuff Primary Raynaud phenomenon is an exaggeration of central and local vasomotor responses to cold or emotional stresses o It affects up to 5% of people, and is most common in young women o - Late in the disease structural changes happen in the artery wall, when the intima thickens o Raynaud phenomenon is usually benign, but long-standing ones can cause atrophy of the skin, subcutaneous tissues, and muscles Secondary Raynaud phenomenon is vascular insufficiency of the extremities secondary to artery disease caused by other things, like lupus, scleroderma, Buerger disease, or atherosclerosis o Raynaud phenomenon can be the first sign of these problems 90% of veinous diseases are varicose veins and phlebothrombosis/thrombophlebitis Varicose veins – abnormally dilated tortuous veins formed from prolonged increased intraluminal pressure and loss of vessel wall support – page 519 - - - - Usually varicose veins affects the superficial veins of the upper and lower leg When legs “are dependent” for prolonged periods, venous pressures there can be very increased and lead to vein stasis and pedal edema o When this happens in seemingly normal veins, it’s called simple orthostatic edema Up to 1/5 of guys and 1/3 of girls develop lower extremity varicose veins o Women are more affected because of higher pressures in the veins in their legs due to pregnancy Obesity increase the risk for varicose veins Varicose veins runs in families Varicose dilation of the veins makes the valves incompetent and leads to stasis, congestion, edema, pain, and thrombosis o The worst symptoms are persistent edema in the leg and ischemic skin changes, including stasis dermatitis and ulcers o Poor wound healing and superimposed infections can lead to chronic varicose ulcers o Embolism from superficial veins is very rare, unlike deep vein thrombosis (DVT) Esophageal varices – caused by liver cirrhosis o Liver cirrhosis causes portal vein hypertension, which leads to opening of portalsystemic shunts that increase the blood flow into veins at the gastro-esophageal junction (esophageal varices), rectum (hemorrhoids), and periumbilical veins of the abdominal wall (caput medusa) o Esophageal varices are the most important, since their rupture can lead to massive and possible fatal upper GI hemorrhage o Hemorrhoids can also be caused by primary varicose dilation of the venous plexus at the anorectal junction It’s caused by prolonged pelvic vascular congestion from pregnancy or chronic constipation Hemorrhoids can bleed, thrombose, and get inflamed, and are prone to painful ulceration Deep leg veins are the site of more than 90% of cases of thrombophlebitis and phlebothrombosis (which both basically mean vein thrombosis and inflammation) - - - - Deep venous thrombosis (DVT) of the legs is caused by prolonged immobilization that causes decreased blood flow through the veins o This can happen from extended bed rest, sitting for a while (like an airplane or car ride), and after surgery o Anything that slows venous return can cause DVT, including heart failure, pregnancy, and obesity Systemic hypercoagulability often predisposes to thrombophlebitis o In some paraneoplastic syndrome adenocarcinomas, they make lots of pro-coagulant factors, which cause venous thrombosis to classically appear in one site, disappear, and then reoccur in other veins This is called migratory thrombophlebitis (Trousseau sign) Thrombi in legs produce few, if any, reliable signs of symptoms o They sometimes show distal edema, cyanosis, superficial vein dilation, heat, tenderness, redness, swelling, or pain o Some tests that may check for these symptoms include pressure over affected veins, squeezing the calf muscles, or forced dorsiflexion of the foot (Homan sign) DVT’s can fragment and embolize, causing pulmonary embolisms o Pulmonary embolism is often the first sign of thrombophlebitis Superior vena cava syndrome – when cancer compresses or invades the superior vena cava - Often the cancer is bronchogenic carcinoma or mediastinal lymphoma The obstruction causes characteristic dilation of the veins of the head, neck, and arms, and cyanosis Pulmonary vessels can also be compressed, causing respiratory distress Inferior vena cava syndrome – cancer compresses or invades the inferior vena cava, or a thrombus compresses that came from the liver, kidney, or lower extremity veins - Certain cancers, like hepatocellular carcinoma and renal cell carcinoma, tend to grow within veins, and can occlude the inferior vena cava Inferior vena cava obstruction causes lower extremity edema, distention of the superficial collateral veins of the lower abdomen, and proteinuria when the kidney veins are involved Primary problems with lymphatic vessels are very uncommon Secondary problems with lymphatic vessels are much more common, & seen in inflammation or cancer Lymphangitis – acute inflammation caused when bacterial infections spread into lymph - The most common bacteria is group A β-hemolytic strep The affected lymphatics are dilated and filled with an exudate of neutrophils and monocytes o - The infiltrate can extend through the vessel wall into nearby tissues, and cause cellulitis or focal abscesses Lymphangitis looks like red, painful subcutaneous streaks (the inflamed lymphatics), and painful enlargement of draining lymph nodes (acute lymphadenitis) If the bacteria gets through the lymph, it can get to the veins and cause sepsis Lymphedema: - - Primary lymphedema: o Can be an isolated congenital defect, called simple congenital lymphedema, or as the familial Milroy disease (heredofamilial congenital lymphedema), which causes lymphatic agenesis or hypoplasia Secondary (obstructive) lymphedema happens from blockage of previously normal lymphatics o Obstruction can be from tumors, surgery, fibrosis (scarring), or filariasis Both types of lymphedema increase the hydrostatic pressure in the lymphatics distal the obstruction, and causes increased interstitial fluid accumulation (edema) o Persistence of this edema causes increased deposition of interstitial connective tissue, brawny induration or peau d’orange (orange peel) appearance of the overlying skin, and eventually ulcers from inadequate tissue perfusion o Accumulation of lymph can cause chylous ascites (in abdomen), chylothorax, and chylopericardium The lymph gets there from rupture of dilated lymphatics usually from obstruction by a tumor Primary tumors of large vessels (aorta, pulmonary artery, vena cava) are very rare, and are mostly connective tissue sarcomas Vascular cancers can come from the endothelium (hemangioma, lymphangioma, angiosarcoma) or from cells that support and/or surround blood vessels (glomus tumor, hemangiopericytoma) Benign blood tumors usually produce obvious vascular channels (vessels) filled with blood cells or lymph, lined by a layer of normal-looking endothelial cells Malignant tumors are more cellular, show atypia, and are proliferative with mitotic figures, and usually don’t form well-organized vessels You can look for CD31 or von Willebrand’s factor to see if the tumor came from endothelium Benign blood tumors: - Hemangioma – very common tumors characterized by increased #’s of vessels filled with blood o Page 521 – pic of hemangiomas o Hemangiomas are 7% of all benign tumors in kids o Most hemangiomas present form birth, and expand as the kid grows o Many capillary lesions regress spontaneously o - Most hemangiomas are localized, and most are superficial lesions of the head or neck 1/3 of hemangiomas though are found internally in the liver o It’s rare for a hemangiomas to turn malignant, if ever o Capillary hemangioma - happens in the skin, subcutaneous tissues, and mucous membranes of the oral cavities and lips, and in the liver, spleen, and kidneys The most common form of hemangioma It’s called “strawberry type” or juvenile hemangioma of the skin in newborns, and is extremely common – page 521 top right pic Capillary hemngiomas grow rapidly in the first few months, but then fades at 13 years old, and completely regresses by age 7 in up to 90% of cases Capillary hemangiomas are bright red/blue with an intact overlying epithlium Capillary hemangiomas are unencapsulated aggregates of closely packed capillaries, usually filled with blood and lined by endothelium When the capillaries rupture, it causes hemosiderin pigment in the lesion and focal scarring o Cavernous hemangioma – show large dilated vascular channels that are less circumscribed than capillary hemangiomas and more often involve deep structures Cavernous hemangiomas can be locally destructive, and don’t tend to spontaneously regress, so they may need surgery Most cases are not of clinical significance, but can vulnerable to ulcer and bleed Cavernous hemangiomas are seen in von Hippel-Lindaue disease, happening in the cerebellum, brainstem, or retina, along with similar lesions in the pancreas and liver Cavernous hemangiomas are red/blue, soft, spongy masses made of large cavernous blood-filled vascular spaces – page 521 bottom left pic Intravascular thrombosis with dystrophic calcification is common o Pyogenic granuloma – rapidly growing pedunculated red nodule on the skin, gingiva, or oral mucosa – page 521 bottom right pic It bleeds easily and is often ulcerated About 1/3 of pyogenic granulomas develop after trauma, and grow The proliferating capillaries are accompanied by lots of edema and inflammatory infiltrate similar to granulation tissue Pregnancy tumor (granuloma gravidarum) – pyogenic granuloma that happens rarely in the gingiva of pregnant women Pyogenic granulomas can spontaneously regress or undergo fibrosis Lymphangiomas – benign lymphatic tumors o Simple (capillary) lymphangioma – made of small lymphatic channels in the head, neck, and axiallary subcutaneous tissues They are raised lesions that show endothelial lined spaces different from normal capillaries only in that there are no RBCs o Cavernous lymphangioma (cystic hygroma) – found in the neck or axilla of kids, and common in Turner syndrome - - - They can get huge, and are made of massively dilated lymphatic spaces lined by endothelial cells Glomus tumor (glomangioma) – benign, very painful tumors from smooth muscle cells of the glomus body, a special arteriovenous structure involved in thermoregulation o Glomus tumors are most often found in the distal part of the digits, especially under the fingernails o You fix it by excising the tumor o Glomus tumors are slightly elevated red/blue nodules that are aggregates, nests, and masses of specialized glomus cells Vascular ectasias – common lesions characterized by local dilation of preexisting vessels o They’re not true tumors o Telangiectasia – congenital anomaly or acquired exaggeration of preformed vessels, usually in the skin or mucous membranes, made of capillaries, venules, and arterioles, forming a small red lesion o Nevus flammeus (“birthmark”) – characteristically a flat lesion on the head or neck that can be pink or purple Nevus flammeus is the most common form of ectasia There is only vascular dilation, and most regress Port wine stain – special nevus flammeus that grow in kids, thicken the skin, and don’t fade Port wine stains are seen in Sturge-Weber syndrome, which shows the stains on the face, and mental retardation Often, a port wine stain on the face in Sturge-Weber syndrome usually indicates there are more extensive vascular malformations o Spider telangiectasia – shows a radial, often pulsatile array of dilated subcutaneous arteries or arterioles (looks like legs of a spider) around a central core (the body) Spider telangiectasia is most often seen on the face, neck, or upper chest Spider telangiectasia is usually caused by high estrogen states, like pregnancy or cirrhosis o Hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu) disease) – inherited telangiectasias seen from birth, that are made of dilated capillaries and veins Bacillary angiomatosis – vascular proliferation from an opportunistic infection in immunocompromised people – page 523 o Lesions can be in the skin, bone, brain, or other organs o Infection is caused by Bartonella henselae (causes cat-scratch disease cause cats carry it) and Bartonella Quintana (causes trench fever and is carried by body lice) o Bacillary angiomatosis are red papules and nodules, with capillary proliferation and endothelial cells with atypia and mitoses The lesion includes the Bartonella bacteria The vascular proliferation happens from induction of host HIF-1α by the Bartonella o HIF-1α then drives VEGF making Treat with macrolide antibiotics, like erythromycin Intermediate grade (borderline) blood tumors: - Kaposi sarcoma (KS) – page 524 o Kaposi sarcoma is common in people with AIDS, but rare in other people o 4 forms of Kaposi sarcoma: Chronic Kaposi sarcoma (aka classic or European KS) Characteristically happens in eastern Europeans, especially ashkenazi jews, or Mediterranean people, and is uncommon in the US Chronic KS can happen with an underlying second cancer, or changes in immunity, but it doesn’t happen with HIV Chronic KS shows multiple red to purple skin plaques or nodules, usually in the distal lower extremities o These slowly increase in size and # and spread more proximal Chronic KS tumors are usually asymptomatic and remain localized to the skin and subcutaneous tissue Lymphadenopathic Kaposi sarcoma (aka African or endemic KS) – common in Africa, and not associated with HIV They show lymphadenopathy Lymphadenopathic Kaposi sarcoma is the most common tumor of men in Africa Transplant-associated Kaposi sarcoma – happens from immunosuppression after organ transplant It’s usually aggressive, and affects the lymph nodes, mucosa, and viscera, but not the skin AIDS-associated (epidemic) Kaposi sarcoma - most common cancer in people with AIDS in the US It was a big deal when it first showed up in AIDS patients, but now we give them antivirals that decreases its occurrence to less than a % It can involve the lymph nodes or viscera, and spreads widely early in the disease o Most (95%) of Kaposi sarcoma lesions are infected with human herpesvirus 8 (HHV-8, aka KS-associated herpesvirus, KSHV) HHV-8 is a γ-herpesvirus that’s transmitted by sex and saliva HHV-8 is needed to form Kaposi sarcoma KSHV causes a lytic and a latent infection in endothelial cells Cytokines released by HIV-infected T cells and inflammatory cells cause proliferation VEGF is also induced o o o o o o In latent KSHV infections, apoptosis is prevented by making p53 inhibitors and viral cyclin D At first, only a few spindle cells are infected, but late int eh disease, pretty much all spindle cells carry KSHV, and they express both endothelial cell and smooth muscle markers Classically, there are 3 stages of Kaposi sarcoma: patches, plaque, and nodule Patches – red to purple macules found in the distal lower extremities – page 524 right pic Shows dilated irregular endothelial cell-lined vascular vessels Over time, lesions spread proximally and become larger raised plaques made of dermal accumulations of dilated jagged vascular vessels lined and surrounded by plump spindle cells Eventually, the lesions get nodular and more cancerous Nodules are made of sheets of plump, proliferating spindle cells You see more marked hemorrhage Most primary KSHV infections are asymptomatic Classic Kaposi sarcoma is, at first, restricted to the surface of the body Treat by surgical excision, with a great prognosis Radiation works well for classic and lymphadenopathic KS Immunosuppressive KS can be fixed by removing the immunosuppression AIDS-associated KS is treated with antiretroviral therapy for HIV Malignant blood tumors: - - Angiosarcoma – malignant endothelial cancer that usually affect older people, most often in the skin, soft tissue, breast, and liver – page 525 o Hepatic angiosarcomas are associated with carcinogen exposures, including arsenic, thorotrast (a radioactive contrast), and polyvinyl chloride (seen in a lot of plastic) All of these have a long latent period between exposure & cancer development o Angiosarcomas can also arise in lymphedema, classically in the ipsilateral upper extremity several years after radical mastectomy with lymph node resection for breast cancer It arises from lymph vessels, called lymphangiosarcoma o They start as small asymptomatic, often multiple, red nodules, which eventually become large fleshy masses o An angiosarcoma shows all degrees of differentiation, from anaplastic to recognizable endothelial cells forming blood vessels o Can figure out they come from endothelial cells with CD31 or von willebrand factor o Angiosarcomas are aggressive, locally invasive, and can metastasize easily Hemangiopericytomas – rare tumors from pericytes o Pericytes – myofibroblast-like cells that surround capillaries and venules o Most common in the lower extremities The changes in a vessel after therapeutic intervention (ex: stenting) are similar to those from any vascular insult - - - - - Local endothelial trauma (stents), vascular thrombosis (angioplasty), or abnormal mechanical forces (coronary bypass), all induce similar responses of wall healing So just like how injuries can induce intima hyperplasia leading to atherosclerosis, trauma from vascular intervention tends to cause intima thickening made of recruited smooth muscle cells and their ECM Balloon angioplasty – dilation of an occluded artery by inserting an intravascular catheter with a balloon attached o Done to restore blood flow at sites of occluded arteries, especially in coronary arteries o Simple balloon dilation of an atherosclerotic vessel induces media stretching and causes plaque fracture, often with local hemorrhagic dissection of the adjacent artery wall This restores vascular flow, but with risk of more extensive dissection and lumen thrombosis So you give them anticoagulants to prevent the thrombosis o Most patients have improved symptoms in the short term o Abrupt reclosure can happen from compression of the lumen by extensive dissection or thrombosis o The long-term success of angioplasty is mainly limited by the development of proliferative restenosis, due to intimal thickening Happens in up to half of patients within 6 months of the procedure Coronary stents – expandable tubes of metallic mesh that are inserted to keep the lumen open after angioplasty, and are now used in most angioplasty procedures o Stents keep the lumen large, prevent dissections, & limit vascular spasm o Stents though also cause plaque erosion and/or endothelial cell disruption, so they can cause acute thrombosis So they also need temporary anticoagulants o Metal stents eventually lead to restenosis like just angioplasty does, so now we use stents coated with anti-proliferative drugs that limit smooth muscle cell hyperplasia This causes less intima thickening, but may prolong how long you need the anticoagulants because they slow re-endothelialization Synthetic or autologous vascular grafts are used to replace damaged vessels or bypass diseased arteries o Synthetic grafts only work well in large arteries like the aorta, and small ones cause thrombosis early or late intima hyperplasia Autologous vascular grafts are most often taking the saphenous vein from their leg, or left internal mammary artery, for a coronary artery bypass o Only half of saphenous vein grafts last 10 years Grafts occlude because of thrombosis (early), intima thickening (months to years after), and atherosclerosis (latest problem) o More than 90% of internal mammary artery grafts still work 10 years later