Year 3 - Imperial College London
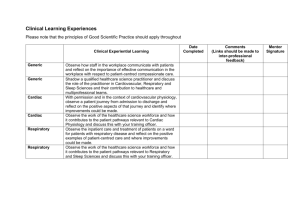
advertisement

School of Medicine Year 3 Clinical Log Book 2009/10 NAME: ....................................................................................... Evelyn Rouse (Years 3 and 5 Curriculum Assistant) Undergraduate Medicine Office Charing Cross Campus Imperial College London Room 138, The Reynolds Building St Dunstan’s Road London W6 8RP Tel: 020 7594 1616 Fax: 020 7594 9315 https://education.med.imperial.ac.uk Clinical Log Book 2009-10 Why use a clinical log book? The clinical part of the medical course is less structured and calls for more selfdirection and initiative than earlier parts. This means that you must take responsibility for directing your own learning in the hospital and general practice environment. This clinical log book is intended to help you with this and we hope you will find it useful. It will: show you what you should be observing, doing and practising when you are in the wards, clinics, theatres and in general practice; help identify any gaps in your learning and guide you in remedying them; prepare you for the Objective Structured Clinical Examination (OSCE), at which you will be assessed on your performance of the skills described in this book. On the Year 3 page of the Intranet we have given some suggestions about time points for learning. These are for guidance only but we hope that it will help you plan and monitor your learning. 1 Clinical Log Book 2009-10 Contents Section Page 1 Getting the most out of your firm 3 2 History and examination skills 4 3 Clinical skills and procedures 11 4 Communication skills 18 5 Patient Safety 25 6 Learning about patient care: Clinical Experience 27 7 Anaesthetics and critical care-learning outcomes 38 8 Formulary of drugs 40 9 Attainments in Pathology 51 2 Section 1 GETTING THE MOST OUT OF YOUR CLINICAL ATTACHMENTS During your clinical course you will be attached to firms and working on the wards. This type of attachment is very different from any learning which you have experienced in the past. You will be expected to plan much of your own learning, including finding and seeing patients for yourself and taking histories from and examining patients. Meet fellow students as a group once or twice a week to share experiences, present cases to each other, look at X-rays and investigation results and learn from each other. The more you do/participate the more you will gain from your clinical experience. There is no substitute for participation! Set yourself objectives for each firm. Your firm leaders will also emphasise this: it is vital that you attend “takes” when your firm is on call (construct a rota for yourselves if necessary). You should all attend the post-take ward-round with the consultant early the next morning. This provides a vast amount of experience in acute medicine and surgery Some suggestions to think about: 1. Talk to patients about what their experience in hospital has been like and how it has affected them and their families. 2. Whenever possible go with patients who are having special investigations and ask if you can watch. This is particularly important with patients you have clerked yourself. 3. Ask if you can observe the physiotherapist, radiographer, cardiology technician, dietician or occupational therapist on the ward or in their department when they are caring for patients allocated to you. Where practicable, offer to help (e.g. taking blood, doing ECGs). Offer to do a blood pressure or TPR round with/for the nurses and do the charting. Ask if you can sit in on a nursing report session. 4. Spend time on the ward after 5 pm when there are less people around and the house officer might appreciate some help with routine tasks and will have more time to talk about your patients. 3 Section 2 HISTORY AND EXAMINATION SKILLS A good history is the most powerful investigative tool we have in getting to understand the patient’s clinical problem. It is a skill which is difficult to acquire and you can only become good at it if you take every opportunity to practise history-taking again, again and again. In taking a history you should: 1. Introduce yourself to the patient and obtain his/her agreement to undertake a clinical assessment. The great majority will be happy to speak to you but some will not and you have to accept that. Try to establish a good rapport and listen sympathetically to the patient. 2. The next and crucial stage of history-taking is a detailed and careful questioning of the patient. Establish the patient’s main complaint or complaints (i.e. the presenting complaint) – in the patient’s own words. 3. Obtain a clear picture of all the important symptoms (the history of the presenting complaint); in particular clarify the chronology and characteristics of each major symptom (this is often best done by having a list of questions ready). Try to avoid medical terms and do not accept ‘diagnostic terms’ from the patient. Instead, get a detailed description of the actual symptoms – in the patient’s own words. Try not to lead the patient, but allow them to communicate their problem in their own way. 4. Having elucidated the clinical problem, go on to the rest of the history: systems review - you should have a set of standard questions to ask about every system but you have to use your judgment about leaving some out if appropriate; past medical history family history – parents, siblings, other close relatives, children personal and social history - including accommodation, work, with whom they are living (tactfully!), smoking and drinking habits (likewise) drug history, including any allergies – and also including non-prescribed drugs such as food supplements and herbal preparations, and recreational drugs other than alcohol and nicotine. See the Communication Skills section for a more detailed description. 5. At the end of this process you should have a good idea what the problem is and you should summarise the history, before going on to the clinical examination of the patient (which is dealt with further on in your log book). 6. The final stage of the history and examination is to construct a differential diagnosis. This is a list of possible pathologies which could explain the features shown by the patient. Try to do this when you write your notes, putting the most likely causes first. You may form a reasonably clear picture of the problem quite early in this process and this will increasingly influence the rest of what you say and do as you gain experience. 4 The main aim of Year 3 is to develop and practise the basic clinical skills of history-taking and examination. Use the log book principally as an aid to help you to do this systematically. Attaining Competence It is suggested that you work with a colleague to provide mutual feedback on your development of clinical competencies. When you feel that you have attained competence in a particular skill, ask a member of your firm, (a consultant, registrar or SHO) a senior nurse or GP, to observe you performing this skill, and if they are satisfied with the standard of your performance. Your firm leaders will want to see you do this as part of their assessment of your overall clinical competence. Ability to conduct a general physical examination Use a Clinical Skills textbook to help you (e.g. “Macleod’s Clinical Examination”), though these may contain more detail than you need. This log book is not in any sense a substitute. Seek the help of ward doctors and work in pairs to prompt each other. You are less likely to leave out important items, especially when you have had relatively little practice. Examined:- Date Date lymph nodes - axillary - cervical - inguinal skin hair and nails breast thyroid lump/mass(any site) Basic ears and throat examination 5 Date Date Examination of the cardiovascular system Examined and presented*:- Date Date Date Date cyanosis/clubbing peripheral and carotid pulses measurement of blood pressure jugular venous pressure palpation of precordium auscultation: normal heart sounds auscultation: murmurs auscultation: lung bases oedemaassessment ophthalmoscopy examination of varicose veins *: in this and succeeding sections regard this as a minimum number! 6 Examination of the respiratory system Examined and presented:- Date Date respiratory rate clubbing/cyanosis shape, expansion of chest position of trachea palpation and percussion of chest auscultation of chest: normal breath sounds auscultation of chest: added sounds 7 Date Date Examination of the alimentary and abdomen system Examined and presented:- Date Date Date jaundice/stigmata of liver disease mouth/hands inspection/general palpation of abdomen palpation of liver and spleen palpation of kidneys palpation of masses auscultation of abdomen hernial orifices/femoral pulses tests for ascites rectal examination* external genitalia* * would not normally be performed on patients during Year 3 8 Date Neurological and mental state examination ** Examined and presented; Date Date Date Date mental functioning including mini mental state exams speech and language balance gait arm drift and pronation cranial nerves (general) incl tuning fork tests power and tone of limbs co-ordination reflexes plantar responses sensation (touch, pin prick, joint position) cerebellar signs extrapyramidal signs upper v lower motor neurone lesion **: remember that there will be a specialised Neurology and Psychiatry attachment in Year 5, and an Ophthalmology attachment in Year 6. 9 Examination of the locomotor system*** Examined and presented: Date Date Date Date joints: inspection and palpation joints: normal and abnormal movement spine: inspection and palpation spinal movement examination of limbs gait GALS screen ***: remember that there will be a specialised rheumatology and orthopaedic surgery attachment in Year 5. For Year 3, you should focus on the GALS screen. 10 Section 3 CLINICAL SKILLS AND PROCEDURES The following skills and procedures may be taught in GP practices, the Clinical Skills Laboratory or on the ward. Your level of confidence and skill will increase only through practice with patients or in the lab. Whilst on all your introductory firms you need to acquire some basic skills; some you will witness, others perform. Because it is important that you obtain regular practice, you should date each time you practice or witness a procedure. We do not feel that being signed off is particularly helpful for either students or teachers but remember that if you do not do or see these procedures only you will lose out. Levels Criteria for Clinical Skills On the following pages you will find a list of skills which should be described or performed during your Year 3 clinical course. The minimum skills level you should attain is shown and the levels have the following meaning: Level 1 – Student can describe Level 2 – Student can perform on a model Level 3 – Student can perform (on patient) with supervision Level 4 – Student can perform without supervision, or can explain or interpret Depending on the learning opportunities available students may have the chance to outperform the minimum levels. 11 Skills to be Described or Performed Skill To Level (1) Date Date Instruments Use the following instruments: Stethoscope 4 Ophthalmoscope 4 Otoscope 4 Tendon Hammer 4 Diagnostic skills Take and record: Blood pressure 4 Temperature 4 Pulse 4 Respiratory rate 4 Further Diagnostic skills Spirometry and respiratory function tests 3 Perform and report ECG 4 Identify normal and some simple abnormalities in ECG 4 Measure and record peak flow rate 4 Record blood glucose measurement 4 Use Glasgow coma scale 4 Check pulse oximetry 4 Test urine (stick) 4 Observe arterial puncture and cannulation 1 Charts Read and record: TPR temperature, pulse, respiratory and blood pressure. 4 Vital signs (temperature, pressure, height and weight). 4 respiratory, blood Fluid balance 4 Treatment drug charts 4 The recommended minimum level is shown here. Level 1 – Student can describe, 2 – can perform on model, 3 – can perform (on patient) with supervision, 4 – can perform without supervision. Depending on the learning opportunities students may have the chance outperform the recommended levels. [1] 12 Skill To Level Procedural Skills Perform the following: Basic life support procedures 2 Scrubbing 4 Administer a metered-dose inhaler and demonstrate an awareness of the different types of inhalers. 4 Administer oxygen at defined concentrations 3 Prescribe and administer a nebuliser 3 Venepuncture 3 Cannulation 3 Male/female catheterisation 3 Suturing 3 Prepare and administer a nebuliser 4 Give injections (intramuscular and subcutaneous). 2 Wound care and dressing 3 Hand washing and infection control 4 Setting up an aseptic trolley 4 Gloving 4 Setting up an infusion 3 Taking a blood culture 3 Taking swabs and specimens for culture 3 Inserting a nasogastric tube 1 Investigations and Scans Interpret arterial blood gases (femoral/radial artery) 4 Interpret simple pathological reports 4 Interpret simple laboratory data haematology and microbiology. from biochemistry, 1 Explain the procedure and understand the interpreted results from: 1 Imaging X Ray Chest – identify simple abnormalities 4 Abdomen – identify simple abnormalities 4 Skeletal - identify simple abnormalities 4 13 Date Date Skill To Level IVU 4 Explain the procedure and understand the interpreted results from: 4 Scans Ultrasound Scan, CT and MRI 4 Isotope Bone, lung and thyroid 4 Understand the interpreted results from: Bronchoscopy 4 Upper GI endoscopy 4 Colonoscopy 4 Sigmoidoscopy 4 Biochemistry 4 U and E 4 Liver Function tests 4 Thyroid Function tests 4 Haematology 4 FBC 4 Clotting tests 4 14 Date Date Procedures to be observed only Skills to be observed (only) Date Blood transfusion Insertion of a CVP line Tracheal intubation Invasive arterial and CVP monitoring Artificial ventilation Pleural aspiration of effusion and pneumothorax Abdominal paracentesis 15 Date Date Other Procedures Procedure Date 16 Date Date Follow patients through the following procedures and be able to explain them simply, avoiding medical jargon. Practice giving explanations to a colleague. endoscopy bronchoscopy upper GI endoscopy colonoscopy sigmoidoscopy radiographic imaging chest x-ray contrast enema contrast meal IVU CT scan ultrasound examination imaging of abdomen and pelvis echocardiography use of Doppler to measure blood flow MRI scan isotope scan bone lung thyroid Please note that there is an opportunity to detail “significant and untoward" operations and procedures observed in the Portfolio of Clinical Experience. 17 Section 4 COMMUNICATION SKILLS You will have many opportunities to develop your communication skills. As well as being able to practice and reflect on how you take a history (gather information) you will also be able to observe and practice both the sharing of information with patients and written communication. To help you in the development of the appropriate skills we have included the lists of the skills associated with effective gathering and sharing of information with patients which you will be familiar with from Years 1 and 2. When practising these skills remember that it is not the practice in itself that is useful but the opportunity to reflect on what you did and to receive feedback. It is the three-tiered approach of practice, reflection and feedback that enables identification of areas of both strength and those that need further work. History taking (gathering information) Take the opportunity to record in the box below 10 consultations which you believe went either very well or very badly and record why you think that was the case. Consultation (record some details of content that will help you recall the consultation) What went well? 18 What could be done differently? Consultation (record some details of content that will help you recall the consultation) What went well? 19 What could be done differently? Sharing information You should aim to observe health professionals performing tasks related to sharing information. Tick the appropriate box when you have seen a task performed. You are then expected to attempt and become competent at certain tasks during Year 3 and the log book should record when you attempted them Date Date Date Date Date Explain a procedure Explain a treatment regime Use the telephone to give information Written communication You will now have the opportunity to write up your own notes. Before doing so read the medical records of some of your patients and reflect on how effective the written documentaries are. Refresh your memory on the skills associated with effective written communication from your notes from Year 2 and bear these in mind when writing and recording histories, examinations and any findings. Tick and date the appropriate box to indicate what you have done. Date Date Date Date Date Record a history and examination Record examination findings Maintain patients' records neatly and accurately By the end of Year 3 you are expected to be competent in the above tasks. 20 In addition there are some tasks to be conducted in MOCK situations only. DO NOT PERFORM THEM IN REAL SITUATIONS AS UNDERGRADUATES. You should aim to observe these as frequently as possible and note in the box below each time you observe such a procedure. Procedure Dates observed Explaining test results Breaking bad news Gaining informed consent for a procedure Writing a discharge letter Writing a clinic letter to a GP Completing a death certificate Writing a clear (and legal) prescription 21 Date(s) practised in mock situation Skills associated with patient-centred interviews Stage 1: Commencing the interview A Preparation Attend to self-comfort Minimise distraction Focus attention on next consultation B Start to establish a relationship Greet the patient Introduce yourself (full name) Clarify your role in health care team Clarify patient’s name Attend to patient’s comfort State purpose of interview Mention note taking Clarify time available Assess patient’s ability to communicate Demonstrate interest and respect Stage 2: Gathering information Use open questions initially Allow patient to complete initial sentence Ask patient if s/he has any questions Demonstrate Active listening Verbal non-verbal Facilitative responses Pick up verbal and non-verbal cues Wait time Survey for problems Set agenda Clarify patient's use of terms Avoid unexplained jargon Summarise Use signposting/transition statements Use silence appropriately Use open-to-closed ended cone Avoid leading questions Avoid multiple questions Probes sensitively Show warmth Make empathic statements Identify patient's feelings Acknowledge feeling 22 Stage 3: Closing the interview Provide an end summary Discuss action plan Carry out a final check further information questions worries and concerns Thank patient and say goodbye Content (PC = Presenting Complaint) Students should be able to obtain information on the following: 1 Patient's major concerns 2 Patients' understanding of the cause of the presenting complaint 3 The effect of the PC on the patient's life 4 History of the PC 5 Previous episodes of the PC 6 Patient's knowledge of treatment to date 7 Patient's knowledge of investigations to date 8 Past medical history previous illnesses at least 5 from list for screening previous hospitalisations/operations medication (PC) medication (other) allergies 9 Family history Parents’ health siblings’ health other family members (e.g. children/partner) 10 Social History age who lives in household work (nature and satisfaction) housing 11 Lifestyle smoking alcohol recreational drugs diet exercise sleep 23 12 Function enquiry (systems to be covered) General Cardio-respiratory Gut Genito-urinary Neurological Musculo-skeletal Thyroid Skills associated with giving information Explain purpose of interview Check what patient already knows Determine amount of information patient wants Use short words and phrases Avoid use of jargon Use explicit categorisation Summarise Use specific advice statements Check understanding Clarify if patient has any questions Clarify if patient has any concerns Use active listening techniques Remember that patients recall best what they are told first and last. Information a patient may wish to know about any given procedure When the procedure will take place Where What preparation is necessary How long it will last How painful it will be Who else will be present What are possible side/after effects When the result will be available Who will give the result Offer to inform relatives There is no single correct approach. Requirement is for flexibility, sensitivity to individual needs and ability to take the initiative to empathise and communicate with the individual. Good practice is rooted in values, primarily the value of the person – adult or child and respect for both the individual and their family or close friends/carer. 24 Section 5 PATIENT SAFETY IN THE 3rd YEAR CURRICULUM Background In order to enhance patient safety a number of strategies and interventions are necessary but it is critical that learning about patient safety and human error should start at an early stage in order to inculcate a culture of safety amongst tomorrow’s doctors. This program represents the formal integration of Patient Safety into the undergraduate curriculum and builds on similar efforts already undertaken within Imperial. The learning objectives of this teaching programme are: To gain an understanding of human error. To appreciate concepts in error theories. To acknowledge that all of us have limitations of knowledge and skill and might need to seek help sometimes. To be able to recognize conditions and situations that predispose to error and to take measures to control them. Teaching format There will be one lecture given to all third year students that will cover all the learning objectives described above. This will be supplemented by two e-learning modules that highlight errors that have occurred in real practice and use these to illustrate key concepts in patient safety theory. All third year students will be expected to access and complete these two modules. Assessment Patient safety principles will be integrated into two OSCE stations during the third year OSCEs and students will be assessed for observed behaviours that reflect safe practice. 25 26 Section 6 Learning about Patient Care CLINICAL EXPERIENCE Introduction 27 Where you will learn 28 Learning Outcomes 28 Learning Methods 29 Inter-professional Learning 30 Checklists Clinical Presentations 31 Syndromes and diseases 34 Anaesthetics, Critical Care and Emergencies are covered in Section 7 Introduction At qualification all doctors, whatever their eventual career path, should have a common core of clinical knowledge and experience. As you move through this year you will proceed from learning basic clinical examination and history taking skills to more complex clinical investigation and management. By the end of the year you will be well on your way towards acquiring the general clinical knowledge and experience necessary to satisfy the medical school and the GMC. In Year 5 you will build on this clinical basis to study some subjects in more depth for example neurology and rheumatology. Remember though that this is a life-long process and, as a very eminent physician once said: “You never know enough”! This section is a companion to your logbook of clinical skills and should be used in a similar way. 27 Where you will learn As you know from this course guide the year includes 4 clinical attachments; one of 4 weeks (completed during Year 2), the next of 8 weeks and the last two of 10 weeks each. It is intended that the first two attachments will be at the same site and that you spend at least one-third of the year at one of central sites (Charing Cross, Chelsea and Westminster or St Mary’s). During the year you will be expected to see emergencies on the ward and in the A and E department and being on emergency take with your firm is a vital part of clinical experience. You will also gain other clinical experience on the wards, in outpatients and in the last 3 attachments in general practice, where you will spend half a day a week for 18 weeks with a general practitioner whose teaching will focus on clinical skills. As you move through the firms you should therefore have the opportunity to meet patients with the common symptoms, syndromes and diseases and you should try to meet patients with less common conditions on the list. Your experience will be paralleled by the Systems and Topics e-Lecture course which will be delivered predominantly as online learning via Blackboard and via up to 10 live lectures during the clinical attachments, and of course you must supplement this with private study using, books, journals and the Internet. PBL will very largely be based on actual patients rather than paper scenarios. Clinical teaching takes place at a large number of hospital sites and it follows that your experience will differ at each location. Teaching will be organised differently to fit in with the clinical service needs of each hospital and with the local availability of particular expertise. The learning objectives however are the same everywhere and the learning programmes will be based on that principle. At or before the beginning of each of your 10-week attachments you will be given a detailed scheme of the learning opportunities for the whole of your stay which will almost always include teaching outside your own firm. Learning outcomes Clinical examination By the end of the year you should know how to examine the normal cardiovascular system, respiratory system etc and be able to recognise common abnormalities of each system. Interviewing patients You should be able to take a history relevant to the symptoms, syndromes and diseases on the list Clinical Knowledge By the end of Year 3 you should know the common causes of the list of general and specific symptoms. You should be able to describe and understand the basic features (presentation, pathophysiology and aspects of pathology), investigations and the principles of clinical management for the common syndromes. 28 Clinical experience You will see a rather formidable list of clinical presentations and even more of syndromes and conditions. Some of these are relatively uncommon and you may see only one or two examples during the year, or even none. But we believe that it is important for you to be aware of the basic facts about even these disorders-we have not included anything really rare or “small print”. Equally, if you are on take and someone with a truly unusual syndrome comes in, do not feel that you should overlook it just because it is not on the list. All clinical experience is valuable. It is also essential to remember at all times, as no doubt you have in the first two years, that: 1. All meetings and interactions with patients are dependent on their consent. Whatever the setting this cannot be taken for granted. 2. Within the limits of what you can and should do you should always take opportunities to be actively helpful in the care of patients, not only as observers. 3. In several of the situations listed here you will appreciate that the patient can take the role of teacher. Learning methods As already mentioned, these will comprise: Lectures Intranet / Blackboard material Tutorials Ward rounds Bedside teaching PBL (mainly patient based) Textbooks Internet sites Journals 29 Interprofessional learning As a doctor you will be part of a team looking after patients. It is therefore important for you to know how other members of the team approach their patients and what skills they bring which will complement your own. Most of your time is spent learning from doctors, but during your attachments in Year 3, to help you with understanding the approach of other team members you will be having some sessions with students of other health care professions. The form that these sessions will take will vary according to the resources of the particular trust: you may be learning alongside other students or from other professionals or both, most often in the context of a Multidisciplinary Team. You will be learning about them but just as importantly they will be learning about your approach as doctors and the impression that you make on them may affect their future attitudes towards doctors. In the OSCE you will be assessed on 1. Promoting effective and appropriate communication between health professionals with the aim of improving the patient pathway. 2. Demonstrating an understanding and respect for the role of others by participating in interprofessional working practices. 3. Demonstrating sound clinical judgement across a range of differing professional and care delivery contexts. Please note that there is an opportunity to detail case studies, where you have observed multi-disciplinary teamworking, in the Portfolio of Clinical Experience. Questions to consider: 1. When taking a history, what questions do other professionals ask that might be useful to you? 2. How do they approach their patient? Is the patient relaxed? How do patients react to their approach of other professionals? 3. How is the information that they gather useful to you? 4. How is it shared with you and others? 5. Do you understand the notes made by other professionals? 6. When would you normally meet other professionals to discuss a patient? 30 Clinical presentations For convenience these are listed under systems headings. As you already realise this may not necessarily fit into predictable categories: for instance, chest pain sometimes has gastro-oesophageal origins. Medical and surgical diagnoses are not separated. It is expected that at the end of the year students will have knowledge of the common differential diagnoses for these symptoms and presentations and a basic scheme of investigation. Since the 3rd and 4th attachments occupy an almost unbroken period of 20 weeks it might be helpful to have some landmarks, bearing in mind that half of you will be doing your medical attachment first and half the surgical. In this section therefore we have marked each presentation or condition as M which is medical or S as surgical. In some circumstances this is rather artificial, but the main purpose is to help you in pacing your learning. You will see that medical conditions predominate and this does reflect clinical practice on an everyday basis. Therefore we suggest: That you familiarise yourself with all items marked S during your surgical attachment, whether you do that first or second. That the items marked M will mainly form part of your medical attachment but that you can take opportunities for learning about them during the surgical firm if it does not interfere with your main learning objectives during that period General Weight loss–also endocrine M Fever M Night sweats M Tiredness - also endocrine, haematology etc M Lumps in neck and groin – also haematology S Rashes – as markers of systemic disease M Cellulitis M Alcohol abuse (may be gastrointestinal, neurological, psychiatric) M Collapse +/- loss of consciousness (may be cardiovascular, neurological) M Cardiovascular Chest pain M Shortness of breath (acute and chronic) – also respiratory M Palpitations M Oedema-also GI, renal M Claudication – also neurological S 31 Stroke –also neurological M Respiratory all M As above Cough Haemoptysis Wheeze Gastrointestinal all S Acute abdominal pain Chronic abdominal pain Nausea and vomiting – also infections, cardiovascular, neurology etc Haematemesis Diarrhoea Constipation Melaena and rectal bleeding Endocrine all M Weight loss Weight gain Polyuria and polydipsia Goitre Haematology all M Lymph node enlargement Pallor Fatigue Easy bruising/bleeding Renal/urology Loin pain S Haematuria S Oedema M Uraemia M Urinary retention S Urinary frequency S Incontinence S Scrotal swelling S 32 Neurology (Year 5 attachment but important general medical presentations) As under cardiovascular, also: all M Acute headache, including meningism Chronic recurrent headache Collapse Seizures Focal weakness Focal sensory disturbance Cognitive deficit/decline Acute confusion/delirium Rheumatology (also a Year 5 attachment but important general medical presentations) Joint pain all M Joint swelling Backache 33 Clinical situations, syndromes and diseases Our intention is that you will become acquainted with main presentations, and the principles of investigation and management of these conditions. You should make every effort to gain first-hand clinical experience of as many as possible. For some rare conditions this may be difficult or impossible but form the majority it should be possible during one of the four attachments in the year, even if, as already mentioned, students have to go outside their own firm. Again, the subdivision is largely by systems, but remember the note in the previous section. Cardiovascular all M unless indicated Myocardial infarction Other acute coronary syndromes Stable angina Acute heart failure Chronic heart failure Atrial fibrillation (see also emergencies) Valve disease including endocarditis Hypertension Aortic aneurysm Cerebrovascular accident (stroke) Lower limb vascular disease S Deep vein thrombosis Pulmonary embolism Varicose veins S Respiratory all M Asthma Chronic obstructive pulmonary disease Pneumonias Tuberculosis Carcinoma of the bronchus Pneumothorax Fibrosing lung disease (especially occupational) Bronchiectasis Gastrointestinal Peptic ulcer disease (see also emergencies, acute abdomen) M Gastro-oesophageal reflux and hiatus hernia M Inflammatory bowel disease M Inguinal and femoral hernias S Hepatitis (acute and chronic) M 34 Cirrhosis and portal hypertension M Cholecystitis and gall stones S Appendicitis S Peritonitis S Pancreatitis M Diarrhoea due to infection or infestation M Haemorrhoids S Anal fissures and fistulas S Diverticular disease S Carcinoma of the large bowel S Carcinoma of the pancreas S Carcinoma of the stomach S Carcinoma of the oesophagus S Endocrine and metabolic all M Diabetes mellitus “Metabolic syndrome” Hypothyroidism Hyperthyroidism Osteoporosis Osteomalacia Diabetes insipidus Hypopituitarism and pituitary tumours Acromegaly Cushing’s syndrome Adrenal insufficiency Hypercalcaemia (including hyperparathyroidism) Hypocalcaemia Haematology all M Anaemias (iron/folate/B12 deficiencies) Leukaemias (acute/chronic) these will be covered in detail Lymphomas in the Year 5 Pathology Course Myeloma but may present in general medicine Clotting disorders (genetic/acquired) Sickle cell disease 35 Renal/urology M/S respectively Acute renal failure (see also emergencies) Chronic renal failure and its complications Glomerulonephritis Use of dialysis (haemo- and peritoneal) Urinary tract infections Renal/ureteric stones Prostatic hypertrophy Carcinoma of the prostate Carcinoma of the kidney Carcinoma of the bladder Congenital abnormalities of renal tract Neurology (predominantly Year 5, but may present in general medical setting) Migraine all M Transient ischaemic episodes Meningitis Peripheral neuropathy Paraparesis / Paraplegia Subarachnoid haemorrhage Parkinson’s disease Epilepsy Dementias Rheumatology (predominantly Year 5, comment as for neurology) Recognition of osteoarthritis and rheumatoid arthritis all M Recognition of multisystem diseases (systemic lupus, sarcoid) Polymyalgia rheumatica Acute arthropathy Oncology mixed M and S unless indicated Malignancies already mentioned under specific systems Concepts of screening Carcinoma of the breast (and non-malignant breast lumps) Principles of radiotherapy and chemotherapy Palliative care including pain management 36 S Medicine for the elderly all M Although most of the conditions affecting the elderly have already been listed (with the very important exception of dementia), students need to be aware of the principles of: Differential epidemiology of disease Variation in disease presentation in the elderly Modifications in management in the elderly Clinical Pharmacology and Therapeutics all M Most of the formal teaching of therapeutics takes place in the final year but the following are part of learning for Year 3: Principles of pharmacokinetics and drug metabolism Types of adverse drug reaction Adverse drug interactions Special considerations in prescribing for the elderly, children and in pregnancy and lactation (these are particularly relevant for Year 5) Principles of new drug development Students should also be aware of the main types of drugs used in the above conditions and their main uses and problems but detailed descriptions of management will not be expected at this point, except for the emergencies listed in the next section. 37 Section 7 ANAESTHETICS AND CRITICAL CARE Learning objectives Understanding the application of basic physiology to the cardiovascular, respiratory and metabolic events, normal and abnormal, occurring during anaesthesia Awareness of the common medical conditions likely to increase perioperative risk and the principles of their management Ability to recognise critical events perioperatively Ability to identify the critically ill patient, in particular the importance of sepsis and the systemic inflammatory response syndrome following major surgery Understanding principles of management of these patients, with particular emphasis on oxygen therapy and fluid balance Understanding approaches to the management of acute pain, particularly postoperatively, and of chronic pain, emphasising the multidisciplinary nature of the pain team Acquisition of practical skills including management of the airway (not intubation), managing delivery of oxygen by different devices, IV cannulation, and setting up IV infusions with additives. Emergencies all M unless indicated This includes most of the important medical and surgical emergencies. If at all possible students should see these on the wards and particularly in A and E departments. It may not be possible to obtain first-hand experience for all of these but awareness of how to recognise them is essential as is knowledge of the principles of management. all M unless indicated Cardiac arrest Anaphylaxis Severe sepsis Meningitis Hypovolaemic shock secondary to haemorrhage Acute arrhythmias (supraventricular and ventricular) Complete heart block Acute left ventricular failure Malignant hypertension Acute arterial occlusion Status asthmaticus Tension pneumothorax Respiratory failure Haematemesis 38 Variceal haemorrhage Perforated ulcer S Acute obstruction S Acute liver failure/encephalopathy Hypoglycaemia Diabetic ketoacidosis Non-ketotic hyperosmolar coma Lactic acidosis Acute adrenal insufficiency Severe hypercalcaemia (esp. in malignancies) Hypo- and hypernatraemia Poisoning salicylates, paracetamol, opiates, tricyclics, methanol, lithium, digoxin Head injury Chest and abdominal trauma Severe burns Status epilepticus Acute paraparesis/paraplegia Acute renal failure Malaria 39 Section 8 FORMULARY OF DRUGS Drug Indication Pharmacological class Comments Please use the following table as a basis for a personal list of drugs and look up all the new drugs you come across in the BNF and standard recommended books. Comments may include patient response, possible side-effects, potential interactions with other drugs. 40 41 Drug Indication Pharmacological class Comments 42 Drug Indication Pharmacological class Comments 43 Drug Indication Pharmacological class Comments 44 Drug Indication Pharmacological class Comments 45 Drug Indication Pharmacological class Comments 46 Drug Indication Pharmacological class Comments 47 Drug Indication Pharmacological class Comments 48 Drug Indication Pharmacological class Comments 49 Drug Indication Pharmacological class Comments 50 Drug Indication Pharmacological class Comments Section 9 ATTAINMENTS IN PATHOLOGY During clinical attachments in Years 3 and 5, you should undertake the following tasks in pathology practice. The list is not exhaustive, merely representative of the pathology skills and knowledge applicable to the practice of medicine. You may be examined in some aspects of these as part of general medicine, pathology, or in an OSCE or PACES, since pathology is key to the study of medicine. These skills are all part of everyday medical and surgical practice and should therefore form part of following through a patient in hospital. The following may be examined in YEAR 3 are marked with an asterisk in the right hand margin. * As you make these observations, or gain these skills, you might wish to tick them off on this list. Cellular Pathology 1 Observe a cervical smear sample being taken and be able to discuss the possible results. 2 Observe a frozen section from an operation being cut and reported by the attendant pathologist 3 Attend a multi-disciplinary team meeting (any of the specialities) at which a pathologist is present. 4 During your surgical attachment follow a surgically-excised specimen from formalin-fixation to diagnosis in the pathology department. 5 Observe a fine needle aspiration of any site, for example lymph node, breast or thyroid and be able to discuss the advantages and disadvantages of this procedure. Some of these will be done in outpatients. Chemical Pathology/Clinical Chemistry 1 Observe, follow-up and interpret blood gas results from a patient from ITU * 2 Observe, follow-up and interpret a low serum sodium from a post-operative patient * 3 Meet a patient with type II diabetes and discuss with the patient the possible complications of this disease * 4 Look at an abnormal liver function test from a patient and attempt to interpret the results * 5 Look at the case notes of a patient with high serum calcium and note the symptoms caused by high calcium levels * 6 Observe and interpret urine dipstick testing for pH, glucose, ketones, bilirubin, blood and protein. * 51 Haematology 1 Observe how a patient is identified and a blood sample is taken for blood grouping/cross-matching * 2 Observe how patient identity and details of blood for transfusion are checked and how a blood transfusion is monitored * 3 Meet a patient with sickle cell disease and be able to describe the clinical features of a painful crisis * 4 Attend an anticoagulant clinic and observe how therapy is monitored and doses are adjusted * 5 Observe a patient receiving either prophylactic or therapeutic heparin and be able to explain how the dose is decided and whether or not therapy requires monitoring * Immunology 1 Know how to send a blood sample for cryoglobulins to the laboratory 2 Know how patients with systemic lupus erythematosus are monitored 3 Know how self-injectable adrenaline is administered 4 Meet a patient with an autoimmune disease or transplant and discuss the immunosuppressive drugs they take and the requirement for monitoring for drug toxicity Microbiology 1 Observe how blood culture is taken aseptically after thorough disinfection of skin 2 Observe how a sample of cerebrospinal fluid is taken aseptically after thorough disinfection of skin 3 Observe how a "Dipstick" is used to test a sample of urine and how the result is interpreted * 4 Know how to instruct a patient to collect a mid-stream specimen of urine * 5 Observe how to collect wound swabs from deeply-infected sites, without skin contamination 52