Prevalence and predictors of bacterial meningitis among infants
advertisement
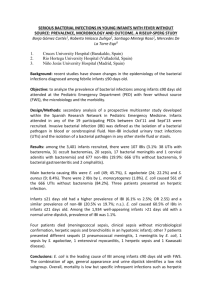
Prevalence and predictors of bacterial meningitis among infants under 90 days old with fever without a source Gomez B, Martínez E, Benito J, Catediano E, Lopez A, Mintegi S Pediatric Emergency Department, Cruces University Hospital, Bilbao (Spain) BACKGROUND: young febrile infants are in a higher risk of having a serious bacterial infection, including bacterial meningitis. In this way, some guidelines recommend performing a lumbar puncture (LP) systematically to every infant under 90 days old with fever without a source (FWS), whereas other ones propose performing it selectively according to clinical and analytical criteria. OBJECTIVE: to describe the prevalence and microbiology of bacterial meningitis (BM) among infants under 90 days old with FWS and to analyze its prevalence according to the general appearance, the age and the presence of altered biomarkers. METHODS: study based on a prospective registry including all the infants ≤90 days old attended with FWS in a Spanish Pediatric Emergency Department during 10 years (Sep'03 - Aug'13). We recommend performing an LP in not well-appearing infants, in those with a clinical suspicion of BM, in those ≤21 days old and in those with altered biomarkers (PCT≥0.5 ng/mL; CRP>20 mg/L; WBC count>15,000/mcL; ANC>10,000/mcL). A BM was defined as the isolation of a bacterial pathogen a) in cerebrospinal fluid (CSF); or b) in a blood culture if pleocytosis was associated. RESULTS: a total of 2,362 infants were attended. An LP was performed in 639 infants (27.0%) and a sample of CSF was obtained in 603 of them (94.3%). An LP was more frequently performed in not well-appearing patients (60.9% vs 25.7% among those classified as well-appearing; OR 4.49 [95% CI 2.83-7.15]) and in those ≤21 days old (70.1% vs 20.4% in those >21 days of age; OR 9.14 [95% CI 6.95-12.02]). Eleven children (0.46%; 95% CI: 0.19-0.73%) were diagnosed with a BM. Isolated bacteria were: S. agalactiae (3), E. coli (3), L. monocytogenes (3), S. pneumoniae (1) and N. meningitidis (1). No bacterial meningitis by L. monocytogenes was diagnosed in the last 6 years. Among the 11 infants, 9 were 21 days of age (prevalence of 2.8% vs 0.1% in those above 21 days of age; OR 30.42 [95% CI 6.13-204.60]); and 5 children were not well-appearing on arrival to the PED (prevalence of 5.7% vs 0.2% in those classified as well-appearing; OR 23.06 [95% CI 5.97-87.44]). The bacterial meningitis diagnosed in infants >21 days old were those by S. pneumoniae and N. meningitidis. The six infants classified as well-appearing upon arrival to the Emergency Department were the youngest ones of the series (age: 4-13 days). Among the 1,975 well-appearing infants >21 days old, an LP was performed in 378 (19.1%), being more frequently among those with altered biomarkers (29.1% vs 14.4% in those with normal blood test results; OR 2.44 [95% CI 1.92-3.09]). No wellappearing infant >21 days old was diagnosed with a BM, regardless of having or not altered biomarkers, neither during the follow-up. CONCLUSIONS: when managing infants under 90 days old with FWS, performing an LP must be strongly considered in not well-appearing infants and in those ≤21 days old. The recommendation of performing systematically an LP in well-appearing infants 2290 days old only due to analytical criteria must be re-evaluated.