Blood Management: A Primer for Clinicians
advertisement

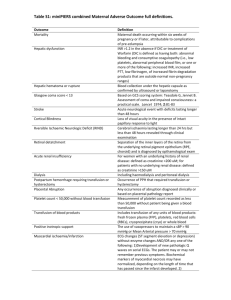
Blood Management: A Primer for Clinicians Abstract and Introduction From Pharmacotherapy Blood Management: A Primer for Clinicians Bradley A. Boucher, Pharm.D., FCCP, FCCM; Timothy J. Hannon, M.D., M.B.A. Authors and Disclosures Posted: 10/29/2007; Pharmacotherapy. 2007;27(10):1394-1411. © 2007 Pharmacotherapy Publications Abstract and Introduction Abstract Blood transfusions are common in the hospital setting. Despite the large commitment of resources to the delivery of blood components, many clinicians have only a vague understanding of the complexities associated with blood management and transfusion therapy. The purpose of this primer is to broaden the awareness of health care practitioners in terms of the risks versus benefits of blood transfusions, their economics, and alternative treatments. By developing and implementing comprehensive blood management programs, hospitals can promote safe and clinically effective blood utilization practices. The cornerstones of blood management programs are the implementation of evidence-based transfusion guidelines to reduce variability in transfusion practice, and the employment of multidisciplinary teams to study, implement, and monitor local blood management strategies. Pharmacists can play a key role in blood management programs by providing technical expertise as well as oversight and monitoring of pharmaceutical agents used to reduce the need for allogeneic blood. Introduction Transfusion of blood products is one of the most common interventions in the hospital setting. The number of blood components trans-fused in the United States was approximately 29 million in 2004.[1] This equates to nearly 80,000 units of blood components transfused every day. In light of the high volume of blood transfusions and their associated risks, regulatory and professional organizations, including the Joint Commission, the American Association of Blood Banks, and the College of American Pathologists, require ongoing monitoring of blood utilization within institutions.[2] The United States Food and Drug Administration (FDA), however, is responsible for ensuring the safety of the nation's blood supply, as well as food and drug safety. Despite the commitment to a large number of resources necessary for the delivery of blood components, and the focus of the FDA and the Joint Commission on safety initiatives, many practitioners have only a vague understanding of the complexities associated with blood transfusion therapy. Owing in large part to a lack of formal training in transfusion medicine for most clinicians, the administration of blood products is surrounded by emotions, misconceptions, myths, and prescribing by habit.[3] Furthermore, despite mounting evidence demonstrating significant harm from unnecessary blood transfusions,[4–6] results of several studies document a generalized lack of compliance with appropriate transfusion guidelines, as well as tremendous variation in transfusion practice among different institutions and among individual physicians within the same institution.[7–11] This lack of familiarity with transfusion guidelines is true not only for physicians and nurses, but also for pharmacists whose focus is primarily on pharmacologic therapy. In many institutions, this is clearly an example of the "silo" mentality where each respective depart-ment and their staff may be naEFve to the challenges being faced by other departments relative to the delivery of optimal health care. In essence, hospital pharmacies take responsibility for the safe storage and effective delivery of drugs to the patient's bedside, whereas blood bank departments are responsible for the same func-tions for blood products. Nonetheless, pharmacists as well as physicians and other health care practitioners have been forced in recent years to become more familiar with blood component therapy by necessity, as drug therapies have clearly overlapped with blood component therapies as therapeutic alternatives. Specific examples include the use of erythropoiesis-stimulating agents, alternatives to red blood cell transfusions, hemostatic agents (e.g., recombinant activated factor VII [rFVIIa]) in patients with refractory hemorrhage, and iron supplementation. Thus, many institutions have embraced the concept of blood management, which can be defined as an evidence-based, multidisciplinary process designed to promote the optimal use of blood products throughout the hospital. The purpose of this review is to serve as a primer on blood management for pharmacists and other health care practitioners interested in broadening their understanding of allogeneic transfusion. Transfusion Medicine Blood products have been a vital and integral part of modern health care since the advent of the first blood bank in 1936. The foundation of the current blood banking industry was laid during World War II, when efficient methods of blood processing, handling, and storage were developed to meet the huge war-time demand. Tremendous advances in blood processing technology and blood screening in the latter half of the 20th century have resulted in steady increases in blood safety and availability. The development of a safe and readily available blood supply has facilitated the advent of life-saving procedures, such as trauma resuscitation, cardiac surgery, organ transplantation, and chemotherapy. None of these procedures could have come about, nor could they exist, without an efficient collection, distribution, and delivery system for these millions of units of blood products. In essence, blood has become the "oil" of the medical industry, lubricating the gears of health care delivery. It is interesting to note that the blood collection industry is facing challenges similar to those found in the oil market, as blood demand threatens to outstrip supply and blood costs escalate. Local and regional blood shortages have become more frequent, leading to delayed hospital admissions and surgery cancellations. This situation is expected to worsen as the population ages and as surgical approaches and chemotherapy regimens that depend on or result in more aggressive use of blood products increase. The economic consequences of this supply and demand situation are discussed in a later section. Risks of Allogeneic Transfusions Although the blood supply is the safest it has ever been, transfusion of blood components remains a high-risk procedure. Each transfusion exposes patients to a variety of potentially serious complications, so unnecessary transfusions make little sense in view of the potential harm.[12–14] The most significant risks of transfusion in 2006 were unrelated to viral transmission.[15] Bacterial contamination of platelets is one of the leading causes of transfusionrelated morbidity and mortality, with a frequency of 1:2000–3000 transfusions.[15] Administration of blood products to the wrong patient (mistransfusion) is also a leading risk associated with transfusions. Although improved donor screening has reduced the risk of hepatitis and human immunodeficiency virus (HIV) transmission to less than one in a million transfusions,[15] mistransfusion still occurs with the alarming frequency of 1:12,000–19,000 units transfused, with death occurring in 1:600,000–800,000 transfusions.[16, 17] One of many concerns about autologous predonation, a topic discussed later in more detail, is that the probability of any transfusion event is increased 3–12-fold in patients who predonate.[18] Predonation causes an iatrogenic anemia, moving the patient closer to a transfusion trigger and exposing them more often to the hazards of the transfusion process itself and the risk of clerical error.[18] Prolonged storage of blood products (up to 42 days for red blood cells) is yet another transfusion concern secondary to a progressive decline in product quality and linear increases in cellular debris and inflammatory mediators.[19, 20] Prolonged storage significantly impairs the ability of stored red blood cells to deliver oxygen to the tissues,[21–23] and the buildup of inflammatory mediators can result in systemic inflammatory syndrome and transfusion-related acute lung injury (TRALI).[24, 25] Acute lung injury is the leading cause of transfusion-related morbidity and mortality worldwide and occurs with an estimated frequency of 1:500 platelet transfusions and 1:1000– 5000 plasma and red blood cell transfusions.[24, 26, 27] The occurrence of TRALI is likely underreported because of a lack of awareness by clinicians. In addition to TRALI being caused by inflammatory mediators, TRALI can also be caused by the presence of anti– human leukocyte antigen antibodies in donor plasma that attack recipient white cells.[28] This is most often seen in plasma products donated by multiparous women because of the exposure of fetal tissues during pregnancy and has caused the United Kingdom to convert to male-only plasma. It now appears that the United States will follow this lead and begin to phase out plasma from female donors (R. Benjamin, American Red Cross, personal communication, October 23, 2006).[29] Transfusion-related immunomodulation (TRIM) is caused by the introduction of a variety of foreign antigens from allogeneic transfusions that invoke immunologic changes in patients who have received a transfusion.[30, 31] These immunologic changes include both stimulation of humoral immunity, which results in alloantibody production, and downregulation of cellular immunity, which results in altered host defenses.[30–32] Unfortunately, these immune system changes often occur in patients who are already stressed by surgery or illness. This TRIM effect is thought to be contributory to the consistent finding of stepwise increases in infection rates,[32– 40] ventilator support times, intensive care unit (ICU) and hospital lengths of stay,[6, 7, 25, 41–44] and short-term and long-term mortality in patients receiving transfusions (Figure 1).[6, 7, 33, 34, 41, 42] Also, several studies have demonstrated higher cancer recurrence rates in transfused versus nontransfused patients with cancer.[45–48] Although the concept of TRIM is still considered controversial by some because of the observational nature of many of the studies, others believe that the evidence is strongly supported by the demonstrated mechanism of action, the doseresponse relationship of the adverse effects, and the fact that the TRIM effect is modulated by leukoreduced blood products and in autologous transfusions.[30] In the face of these substantial risks, the benefits of transfusion therapy, especially the use of red blood cells, are not well elucidated. Few, if any, well-controlled studies demonstrate improved outcomes with red blood cell transfusions.[4, 5, 49–51] The landmark Transfusion Requirements in Critical Care (TRICC) trial published in 1999 was a multicenter, prospective, randomized trial of red blood cell transfusion strategies in 838 critically ill adult patients admitted to 25 Canadian ICUs from 1994– 1997.[4] Patients were excluded from the study for active blood loss at the time of enrollment, chronic anemia, pregnancy, after cardiac surgery, or imminent death. Physicians were also allowed to decline patient participation if they had a question whether to withhold or withdraw ongoing treatment. The 838 enrolled patients were randomly assigned to receive red blood cell transfusions with use of two different strategies: a liberal strategy group received transfusion at a hemoglobin trigger of 10.0 g/dl, and a restrictive strategy group received transfusion at a hemoglobin trigger of 7.0 g/dl. The results of the study were quite surprising in that the more liberal strategy transfusion group did not have better outcomes, which was in contrast to several observational studies that had concluded that critically ill patients had increased adverse outcomes as their hemoglobin levels decreased below 9.0– 9.5 g/dl.[52, 53] Overall, the adjusted multiorgan dysfunction score and in-hospital mortality rate were significantly higher in the liberal transfusion group than in the restrictive transfusion group. Further, no subgroup of these critically ill patients demonstrated an added benefit of higher hemoglobin levels as a result of packed red blood cell transfusion, and most patients in the liberal transfusion group had substantially worse outcomes. Even patients with a cardiac diagnosis did not have improved outcomes with a liberal transfusion strategy, although a greater proportion of patients with severe cardiac disease than other types of disease had attending physicians who declined to enroll patients in the study. The authors' conclusion was that a restrictive strategy of red blood cell transfusions (hemoglobin level 7.0 g/dl ) was at least as effective and possibly superior to a more liberal strategy (hemoglobin level 9.0– 10.0 g/dl) with the possible exception of those patients with acute coronary syndromes.[4] In another study, published in 2004, the authors questioned the benefit of transfusions in a highrisk cardiac population.[5] In this retrospective review of data from more than 24,000 patients enrolled in acute coronary syndrome trials, a multivariate analysis and propensity scoring model were used to derive the independent effects of anemia and transfusions. The authors concluded that blood transfusion in the setting of acute coronary syndromes is associated with higher mortality (adjusted odds ratio 3.94) and that the association persists after adjustment for other predictive factors and timing of events. Based on these findings, they cautioned against the routine use of blood transfusion to maintain arbitrary hematocrit levels in stable patients with ischemic heart disease. Another observational study investigating the impact of nadir hematocrit levels on cardiopulmonary bypass and transfusions in patients who underwent cardiac surgery confirmed worse outcomes (renal injury, renal failure, mortality) after red blood cell transfusions despite the demonstrated adverse effects of anemia in these patients.[49] Thus, although high-risk patient populations experience adverse outcomes from moderate-to-severe anemia, apparently allogeneic transfusions are ineffective in improving their clinical outcomes. Although none of the above-mentioned studies were designed to determine the cause of the higher adverse event rates in patients receiving transfusions, the higher rate was likely the result of the adverse effects of allogeneic blood and the ineffectiveness of stored blood to efficiently deliver oxygen to the tissues.[12, 19] As with any medical therapy, the decision to transfuse must be made in the context of an informed risk-to-benefit analysis. Despite these concerns, some physicians continue to overutilize blood component therapy and order transfusions in a liberal fashion inconsistent with the current scientific evidence.[7] Transfusion practices that are based on the "10/30" rule (the traditional but unsubstantiated practice to transfuse at a hemoglobin level of 10 g/dl or lower and hematocrit of 30% or lower)[7] and other equally outdated standards for component therapy are incongruent with evidence-based transfusion strategies and, therefore, are outside the current standard of care. Informed Consent for Transfusion Therapy Informed consent for blood component therapy is yet another important issue related to transfusion therapy. Under this doctrine, physicians have a duty to disclose to patients the nature of the proposed treatment; the risks, complications, and expected results or effects of the treatment; as well as the alternatives to the treatment, and their attendant risks and benefits.[54] Many physicians do not appreciate or adequately convey this information to patients when discussing transfusion therapy.[55] Good clinical practice and legal doctrine mandate that patients receive sufficient and accurate information to make thoughtful decisions about therapies. One of the National Patient Safety Goals developed by the Joint Commission encourages the active involvement of patients in their care as a patient safety strategy.[56] A comprehensive and active informed consent process, with its give-and-take between physician and patient, falls squarely within the purview of this stated goal. Moreover, although the informed consent discussion is ideally conducted by the treating physician, in most hospitals it is reduced to a printed form offered without discussion with the patient by clerical or nursing staff. It is the physician, however, who has the medical, legal, and ethical duty to obtain a valid informed consent.[54] This duty is fiduciary in nature and cannot be delegated. Similarly, many hospitals violate their internal bylaws, policies, and procedures, or the Joint Commission and the Centers for Medicare and Medicaid Services require-ments, because documentation of the transfusion decision and the informed consent discussion, as well as the informed consent form, often are not placed in the medical chart.[57, 58] As with all therapeutic treatment, it is the duty of hospitals and health care providers to involve patients in their care and to inform them fully of the risks, benefits, and alternatives to transfusions. Blood Transfusion Economics Blood utilization and blood costs are accelerating in the United States at a time when blood products, hospital labor, and health care dollars are in short supply. Difficulties in recruiting donors, increases in the cost of testing and processing blood, and higher skilled-labor costs have caused blood centers to more than double the price of blood over the last few years,[59] with more price increases on the horizon. Within hospitals, the procurement, storage, processing, and transfusion of blood products involve an array of expensive and increasingly scarce resources that include laboratory supplies, pharmaceuticals, and medical devices, as well as significant technician and nursing time.[60–62] The utilization of these resources in the administration of blood products to patients results in a 3–4-fold increase in the total cost of blood beyond the base cost of its acquisition (Figure 2).[60–62] As previously mentioned, a variety of controlled studies have demonstrated a direct relationship between the amount of blood products that patients receive and serious complications. These include increased infection rates, ventilator support times, ICU and hospital lengths of stay, and cancer recurrence rates, each being associated with increased patient care costs (Figure 1). It is particularly instructive to review the variable costs of hospital resources that have been shown to increase when patients receive blood transfusions ( Table 1 ).[33, 39, 63–69] Variable costs are those that are incurred on a per-use or per-event basis, such that they reflect incremental cost burden when they occur or cost savings if avoided. For example, the association between blood transfusion with increased length of stay and ventilator support time would add considerably to total transfusion costs incurred by hospitals. The approximate cost for a postoperative hospital day is $1300,[65] an ICU day $3700, and a ventilated patient in the ICU $4800/day.[66] The incremental cost of a serious bacterial infection in a patient undergoing orthopedic surgery is estimated at $19,000– 20,500,[33, 67] demonstrating the potential economic impact of the link between transfusions and postoperative infections. Bleeding complications can be particularly expensive in patients undergoing surgery, since bleeding can prolong operating room time and impact outcomes, as well as postoperative length of stay. The variable cost/hour of operating room time is $1900–3100,[64] such that even minor intraoperative delays to deal with bleeding can be quite costly. Even more costly is the impact of postoperative bleeding, particularly if it requires repeat surgery. Repeat surgery for bleeding in patients who underwent cardiac surgery has been shown to greatly increase postoperative morbidity and mortality rates[70, 71] and has an incremental cost of $29,300–31,300.[65, 68] With an accounting for all of the resources consumed by these adverse events, the variable cost of a red blood cell transfusion may be as much as $1800–$2800/unit.[69] A final burden faced by hospitals related to blood costs involves reimbursement issues. A recent consulting report noted that the majority of all blood products are transfused to Medicare beneficiaries, and that Medicare reimbursement has consistently failed to account for increases in the total cost of transfusing blood products.[59] The report also noted systemic problems related to hospital coding and billing practices for blood and blood-related services. Blood Management Strategies In response to these issues, health care providers and hospitals are developing multiprofessional strategies to improve blood utilization, improve patient outcomes, and reduce costs. Blood management strategies are defined as proactive processes, techniques, drugs, or medical devices that reduce the need for allogeneic blood when used in an effective and timely manner. By reducing variation in transfusion practice and implementing more efficient methods to manage patients at risk for transfusion, hospitals can reduce the need for allogeneic blood products while improving patient safety and clinical outcomes. The following are key principles for developing effective blood management programs: Early identification and intervention for patients at high risk for transfusions Utilization of current scientific evidence and the promotion of clinical best practices Coordination of all members of the health care team Patient advocacy and patient safety Stewardship of scarce and expensive hospital resources Specific strategies to manage blood resources more efficiently include the judicious use of autotransfusion devices, systemic drugs that reduce bleeding, surgical and anesthetic techniques,[72] erythropoiesis-stimulating agents,[73] topical hemostatic agents, and measures to reduce iatrogenic blood loss.[74] Blood management strategies that are most likely to involve pharmacists are discussed below. Preoperative Preparation and Planning Preoperative preparation and planning are essential elements for the safe and optimal management of surgical patients. Through the early identification of high-risk patients who are amenable to strategies to modify those risks, hospitals can improve patient outcomes and improve overall resource utilization through reduced adverse events. In addition to the type and complexity of surgery, the universal predictors for transfusion requirements are preoperative anemia and a preexisting coagulopathy.[75–78] Formal protocols for preoperative testing of hemoglobin level for major blood loss surgeries and coagulation status testing in certain patient populations are important for this early identification and intervention. There should also be established protocols for discontinuation of drugs such as aspirin, warfarin, and clopidogrel, as well as certain herbal supplements that increase bleeding including garlic, ginkgo, and ginseng.[79] Anemia management protocols are essential to blood management programs because they selectively use iron and erythropoiesis-stimulating agents to increase red blood cell mass in anemic patients, allowing them to reduce or eliminate their need for allogeneic blood during moderate-to-high blood loss surgeries.[80] Nonpharmacologic Strategies A number of nonpharmacologic strategies can be used to decrease the need for allogeneic red blood cell transfusions. Most of these strategies are low cost in nature and can be easily implemented once nurses and physicians are motivated to minimize allogeneic transfusion requirements. One such strategy is to minimize the impact of diagnostic phlebotomy on the development of anemia, especially in critically ill patients.[81] In a study of 145 Western European medical-surgical ICUs, an average of 41.1 ml of blood was phlebotomized from patients daily.[6] Similar findings have been documented from ICUs in the United States.[82] Deceasing the frequency of phlebotomy is one obvious approach to minimizing iatrogenic anemia by obtaining laboratory tests only when clinically justified.[81] Also, discontinuation of invasive lines (e.g., arterial catheters, central venous catheters) should occur as soon as possible, since the ease with which samples can be obtained from these monitoring devices is thought to contribute to unnecessary blood sampling.[81] Use of smallvolume sampling tubes (e.g., pediatric sampling tubes) when feasible is yet another straightforward method for decreasing blood losses secondary to phlebotomy. Point-of-care bedside analytic techniques (e.g., blood glucose analyzers, arterial blood gas analyzers) that require only small volumes of blood can be used to accomplish the same goal.[81] Cost savings to the institution may be realized with these techniques as well. Use of closed systems of blood sampling in which blood obtained in clear catheters of infusate is not discarded are also advocated.[81] Intraoperative blood recovery (i.e., cell salvage methods) with subsequent reinfusion of shed blood into a patient that has experienced significant surgical bleeding is another common method to minimize allogeneic red blood cell transfusions. A recent meta-analysis determined that the mean reduction in red blood cell transfusions was 0.64 unit/patient with use of cell salvage methods, without any apparent adverse effects on clinical outcomes.[83] Utilization of advanced surgical techniques may also be relatively advantageous in terms of decreasing surgical blood loss. These surgical methods include laparoscopic, endoscopic, robotic, and transcatheter techniques, as well as use of advanced surgical instrumentation (e.g., ultrasonic scalpel, argon bean coagulator).[84] Collectively, integration of any or all of these nonpharmacologic strategies into a comprehensive blood management program has the potential to significantly reduce red blood cell transfusions in a cost neutral fashion without any negative clinical consequences. Iron Therapy Inadequate iron stores will eventually result in iron-deficient anemia. Furthermore, the anemia of inflammation involving attenuation of erythropoiesis may coexist with functional iron deficiency in critically ill patients.[85] In each instance, iron replacement therapy is warranted to reverse the anemia and minimize the use of red blood cell transfusions. Iron replacement therapy typically involves enteral administration of ferrous sulfate, gluconate, fumarate, or iron polysaccharide in ambulatory patients with iron-deficient anemia. Nonetheless, parenteral iron replacement therapy with iron sucrose, ferric gluconate, or iron dextran is often required because of gastrointestinal adverse effects associated with the enteral products or compromised enteral bioavailability in critically ill patients.[85, 86] These latter products are associated with a variety of adverse effects especially with long-term use (e.g., in patients with end-stage kidney disease).[87] Such adverse effects include anaphylaxis, acute renal tubular toxicity, accelerated atherosclerosis, and the potential for increasing the infectious risk by providing iron to the microbial pathogen.[86, 87] This latter concern remains controversial. Erythropoiesis-Stimulating Agents Among the pharmacologic strategies to minimize allogeneic blood transfusions, administration of erythropoiesis-stimulating agents has unquestionably received the greatest attention. Two such agents are available in the United States, namely, epoetin alfa and darbepoetin alfa. Epoetin alfa is a recombinant form of human erythropoietin, whereas darbepoetin alfa is a closely related higher molecular weight derivative of erythropoietin. The extensive use of erythropoiesisstimulating agents in clinical practice relates to data demonstrating blunted erythropoiesis in patients at high risk for acute anemia (e.g., chronic renal failure), commercial availability, and a large body of evidence documenting their ability to reduce the overall number of red blood cell transfusions. Although only two erythropoiesis-stimulating agents are available in the United States, other erythropoiesis-stimulating agents and novel strategies for simulating erythropoiesis are under investigation.[88] Epoetin alfa and darbepoetin alfa are indicated for the treatment of anemia associated with chronic renal failure and chemotherapy-induced anemia in patients with nonmyeloid malignancies. In each of these instances, data have demonstrated that these agents decrease the need for transfusions and increase and/or maintain hemoglobin concentrations.[89, 90] The time course for these positive outcomes to be realized range from several weeks to months. The erythropoiesis-stimulating agents have been the standard of care for the treatment of anemia associated with chronic renal disease and chemotherapy-related anemia for more than a decade. The relative merits of using the newer derivative, darbepoetin alfa, is a subject of active debate.[91] Although many issues remain unresolved with the use of erythropoietic stimulating proteins in patients with renal disease or cancer, the most prominent are those that surround doses and scheduling of doses, target hemoglobin concentrations, and concern regarding refractory patients.[91–93] As a result of concerns regarding increased occurrences of thrombotic events in patients with chronic renal failure, patients with cancer who are receiving chemotherapy, and surgical candidates, the FDA has recently recommended that health care professionals use the lowest dose possible of erythropoiesis-stimulating agent to gradually increase the hemoglobin concentration and to target hemoglobin concentrations that do not exceed 12 g/dl.[94] Epoetin alfa is also indicated for the treatment of anemia associated with HIV in patients receiving zidovudine and for reduction of allogeneic red blood cell transfusions in patients undergoing elective, nonvascular, noncardiac surgeries. Readers are referred to two recent reviews regarding the role of erythropoiesis-stimulating agents in the management of preoperative anemia and within the concept of bloodless medical care.[95, 96] In each of these instances, achievement and/or maintenance of adequate iron stores is an integral element relative to the success of these agents.[85] In recent years, epoetin alfa has also been clinically investigated for the treatment of anemia in critically ill patients.[86, 97, 98] Table 2 summarizes the major trials that studied epoetin alfa for this indication, including a recent trial completed in mechanically ventilated patients receiving care in two long-term acute care facilities.[99-104] Outstanding clinical questions to be considered relative to this issue include the optimal use of erythropoiesis-stimulating agents in the critically ill patient, identifying those patients most likely to derive benefit from this pharmacologic strategy, as well as dose, time to initiation of therapy, duration of therapy, route of administration (e.g., subcutaneous vs intravenous), and the lower threshold at which concurrent red blood cell transfusions should be given in patients receiving these agents.[97, 98] Results from a recently completed study of erythropoiesis-stimulating agents in critically ill patients that have not yet been published may provide additional insights in terms of further framing their role within this patient subset. One of the biggest factors that could limit the use of epoetin alfa and darbepoetin alfa in all patient subsets relates to their pharmacoeconomics. A major challenge in conducting pharmacoeconomic studies, however, is the full breadth of the potential effects of blood transfusions. As outlined above, to merely focus on the direct infectious complications of red blood cell transfusions or the acquisition and delivery costs associated with these transfusions may be vastly understating the economic factors. Hemostatic Blood Products and Drugs Acute blood loss can occur in a variety of medical and surgery settings. These include gastrointestinal bleeding, hemophilia, and perioperative bleeding. In trauma patients, acute hemorrhage is typically caused by vascular injury combined with coagulopathy. Hemorrhage secondary to injury to the major vessels requires surgical intervention for bleeding control in addition to transfusions to replace red blood cells that have been lost. However, reversal of acute coagulopathy regardless of etiology generally requires a multifaceted approach. Traditionally, the mainstays of therapy include transfusion of fresh frozen plasma, platelets, platelet factor concentrates, and cryoprecipitate, as well as reversal of hypothermia and acidosis that often accompany acute blood loss ( Table 3 ).[105–107] Readers are directed to more focused reviews on the use of conventional blood products in the treatment of massive hemorrhage.[108] Regardless, in refractory patients, a number of pharmacologic agents have been used as adjunctive therapies to control bleeding. One of the more controversial agents over the last few years is the off-label use of rFVIIa. A review of 117 case series and reports using rFVIIa in nonhemophilic trauma and surgery patients revealed restoration of hemostasis in 85% of the patients receiving the product.[109] Although rFVIIa doses were not uniformly reported, the mean ± SD dose where data were available was 81 ± 32 µg/kg (range 20– 144 µg/kg). Other outcomes reported in a subset of these cases were a reduction in mean packed red blood cell units transfused before and after rFVIIa (mean ± SD 37 ± 26 units in 30 patients and 2 ± 1.5 units in 6 patients, respectively) and improvement in coagulation test times. Overall survival rate was 77% in the cases included in the review. These results were generally confirmed in two parallel, randomized, placebo-controlled trials of rFVIIa in patients with blunt or penetrating trauma.[110] The effects were most apparent in the patients with blunt trauma in whom the number of red blood cell transfusions was significantly reduced (estimated reduction of 2.6 units/patient) as well as the percentage of patients needing massive transfusions (defined as requiring > 20 units of red blood cells). Adverse events (i.e., death, thromboembolic events, multiple organ failure, and acute respiratory distress syndrome) were evenly distributed between those patients receiving rFVIIa and those receiving placebo. Other off-label indications for use of rFVIIa include intracerebral hemorrhage,[111] liver disease,[112] obstetrics,[113] and other assorted bleeding conditions.[112] An unresolved issue surrounding the use of rFVIIa is its safety; the risk of thromboembolic events in patients receiving this agent for off-label uses was recently highlighted.[114] These events include nonintra-cerebral hemorrhagic stroke, acute myocardial infarction, other arterial thromboembolisms, venous thromboembolisms, and pulmonary emboli. The potential for positive reporting bias for all studies using rFVIIa for off-label uses is another concern that may limit its general applicability. Furthermore, the optimal dose of rFVIIa in nonhemophilic patients is undefined. This issue is particularly important in light of the high acquisition costs for rFVIIa. The average cost of rFVIIa therapy for trauma patients was estimated at more than $25,000.[109] Rigorous pharmacoeconomic analyses are warranted to evaluate this cost and the associated adverse event costs against cost savings in other areas (e.g., reduced transfusions, reduced morbidities) to determine the net cost/life saved. In patients with hemophilia with severe bleeding, the use of rFVIIa appears to be highly effective and result in a relatively low rate of thrombotic complications (1– 2%).[115] Other pharmacologic agents that have been investigated for their adjunctive role in reducing blood loss include desmopressin and the antifibrinolytics, aprotinin, tranexamic acid, and epsilon-aminocaproic acid. The primary role for these agents has been during the perioperative period. A systematic review of 18 controlled trials of desmopressin for minimizing perioperative allogeneic blood transfusion concluded that there is no benefit to be derived from this drug for this indication in patients without congenital bleeding disorders.[116] Nonetheless, a systematic review of antifibrinolytics by the same investigators yielded more favorable results. In 61 trials of aprotinin (7027 patients), a mean reduction of 1.1 red blood cell units transfused (range 0.69– 1.47 units) was observed during the perioperative period in those patients requiring a transfusion, without evidence of excess risk of adverse events.[117] Most of these studies were in patients undergoing cardiac surgery. A similar result was found for tranexamic acid in 18 trials (1342 patients) where the red blood cell unit savings was 1.03 units (range 0.67– 1.39 units).[117] Trials evaluating epsilon-aminocaproic acid for this indication were more limited (four studies) and did not indicate a statistically significant reduction in red blood cell transfusions.[117] Eight head-to-head studies between aprotinin and tranexamic acid did not suggest a relative advantage of one agent over the other. As such, the role of aprotinin in significantly reducing red blood cell transfusions in, at least, patients undergoing cardiac surgery, is well established with a strong likelihood for similar results with tranexamic acid. Regardless, a significant association between aprotinin and serious end-organ damage (i.e., heart, lung, brain) in patients undergoing cardiac surgery has raised concerns in terms of its use versus alternative antifibrinolytic agents. This is based largely on results of a recently published, prospective, large-scale, observational investigation.[118] Since tranexamic acid and epsilonaminocaproic acid are significantly less expensive than aprotinin, future studies should focus on their relative overall cost-effectiveness for selected populations, taking into account not only acquisition costs but also costs of associated adverse events. Local use of biologic surgical packing materials (i.e., chitosan) and fibrin glues may also be used to minimize intraoperative blood loss.[84] Artificial Oxygen Carriers The quest for artificial oxygen carrier solutions as alternatives to allogeneic blood transfusions has spanned decades. Indications for these products have focused primarily on the perioperative setting, sustaining regional perfusion (e.g., stroke, myocardial infarction), and acute hemorrhagic shock.[119] Leading candidates emerging from this line of investigation include hemoglobinbased oxygen carriers and perfluorocarbon emulsions.[120, 121] Although none of these products have been approved for use in the United States or Europe, clinical trials are investigating the safety and efficacy of these agents. Regardless, the possibility of one or more of these products being licensed as blood transfusion alternatives within the foreseeable future remains to be seen. An interesting point is that while specific objective clinical end points are mandated for approval of these products, such end points have never been required or established for red blood cell transfusions.[119] Other challenging product development issues relate to the relative safety and cost-effectiveness of these products compared with allogeneic blood transfusions. Readers are directed to recent reviews on blood substitutes for a more detailed history and summary of the clinical trials of these products.[119–122] Autologous Predonation One strategy believed to result in avoidance of allogeneic red blood cell transfusions in some patients undergoing elective surgery is preoperative autologous donation. Typically, patients will donate 1– 3 units of packed red blood cells over a 3– 4-week period before their elective surgery.[84] However, the efficacy and cost-effectiveness of preoperative autologous donation have not been well established.[84] Noteworthy is that this strategy can be combined with administration of epoetin alfa and iron therapy preoperatively in an attempt to "optimize" the patient hematologically.[123] Risks associated with preoperative autologous donation include transfusion-associated circulatory overload[124] and the potential for clerical misidentification during the transfusion process.[18] These two risks are due to lower hemoglobin levels in preoperative autologous donation cases, moving them closer to a transfusion trigger, and more liberal transfusion triggers (autologous and/or allogeneic transfusions) in patients who receive preoperative autologous donation in spite of recommendations against this practice.[84, 125] Paradoxically, the use of autologous predonated blood can cause an iatrogenic anemia with return of the predonated blood.[126] There is also the potential for waste if the unit collected is not needed, which on average occurs in more than half of preoperative autologous donation cases.[84, 124] For this and other reasons detailed elsewhere, the use of autologous predonation is being discouraged in favor of intraoperative blood donation (acute normovolemic hemodilution)[72] and the use of algorithms that employ selective preoperative epoetin alfa and the use of evidencebased transfusion guidelines (Figure 3).[127] Cost-Effectiveness of Transfusion Alternatives A full economic analysis of these blood management strategies is beyond the scope of this review. However, it is worthwhile to have a framework for future analysis of the costeffectiveness of these therapies. Whereas authors often use the term "cost-effectiveness" to describe various types of economic analyses, there is a significant difference in the types of studies that seek to evaluate the trade-off between costs incurred and benefits gained for a particular therapy. Economic evaluations are divided into types based on how the outcome of the therapy was measured; specifically, these include cost-minimization, cost-effectiveness, costbenefit, and cost-utility. Table 4 summarizes these different measurement schemes, as well as the setting in which each is most frequently used. Examples of the two common economic decisions faced by hospital pharmacists related to blood management (i.e., cost-minimization and costeffectiveness analyses) are discussed below. Cost-Minimization Analysis This type of analysis is a simple comparison of the direct costs of two competing therapies. Although simple to do, cost-minimization analysis is rarely appropriate in the clinical setting because it assumes that all outcomes of the therapies being compared are the same. If, in fact, the outcomes differ, then the total costs of a particular therapy would not be captured. Many published studies use this simplistic and incomplete type of analysis. It is also the most common type of informal analysis done at the departmental level. The use of a cost-minimization analysis is particularly hazardous when a departmental "silo budget" exists. A silo budget occurs when cost centers are assigned to functional units within the organization that do not fully control their revenues and costs, yet they are held accountable for a fixed budget. This situation occurs commonly with hospital pharmacies where annual budgets are often set based on historical data (i.e., a percentage of last year's budget) rather than a continuous assessment of goals and requirements. If a pharmacy department is asked to increase their costs by the addition of new albeit expensive agents that reduce bleeding and transfusions, they may be tempted to resist such additions regardless of published evidence supporting improved patient outcomes. In these cases, the pharmacy department generally does not benefit economically from those improved outcomes despite potential improvements in quality of care and decreased total costs incurred by other departments, such as nursing and blood bank. Thus, although a cost-minimization analysis may result in the pharmacy minimizing its own departmental costs, this outcome may not be efficient from the hospital's perspective. Cost-Effectiveness Analysis A more appropriate evaluation of transfusion alternatives would be a cost-effectiveness analysis, which measures the cost of a treatment to achieve specific outcomes, such as units of blood avoided, or patient outcome measures, such as reductions in infection rates or days of hospitalization. This method represents a more sophisticated analysis of total costs versus total benefits but requires more effort on the part of the hospital as well as more flexible methods of budgeting and accountability. Changing Transfusion Practices The most challenging but potentially the most effective method to reduce allogeneic transfusions is to develop systems that promote the use of evidence-based transfusion guidelines.[128, 129] Of importance, physicians have to take responsibility for changing their transfusion prescribing habits. Regardless, the challenges to changing physician practice are many and include environmental factors such as poor communication between physicians and other members of the health care team, misalignment among individuals and departments due to different motivation and reward systems, a lack of experience in the use of cross-functional teams, and a failure to anticipate and deal with resistance.[130] It is therefore not surprising that hospitals struggle to implement quality initiatives and departmental reengineering projects. Numerous reports have been published describing attempts to change transfusion practices at the institutional level. A summary of these studies can be found in a recent systematic review addressing this topic.[131] The behavioral interventions used to change transfusion practices in the studies evaluated included the adoption of guidelines, education, reminders, and audits. Overall, it was concluded by the authors that even simple interventions appear to be effective in changing physician transfusion practices, thereby reducing blood utilization. Unfortunately, the heterogeneity of the studies evaluated did not allow for identifying the relative superiority of one intervention strategy over another or the merits of single versus multiple strategies being used. Furthermore, the cost-effectiveness of these strategies could not be evaluated. A recent study provides evidence that computerized provider order entry coupled with an electronic evidenced-based red blood cell transfusion algorithm may be a powerful tool for affecting changes in transfusion practices.[132] Interactive decisions with immediate feedback to the provider was a component of this system at the time of ordering a red blood cell transfusion. Results from this investigation revealed a significant reduction in the likelihood of administering a red blood cell transfusion after introduction of the protocol compared with the control period (odds ratio 0.43). Regardless of the strategy used, in general there appear to be three major stages in the process for changing medical practice: priming, focusing on learning alternative practices, and followup.[133] As a consequence of the major studies addressing the problems associated with allogeneic red blood cell transfusions, the priming stage of the change process appears to have already occurred.[134] Thus, efforts should be directed at the later two stages of the change process, namely, focused education on transfusion requirements, and feedback after implementation of a blood management program by appropriate persons within an institution. Since the decision to transfuse is made thousands of times a day in U.S. hospitals by a multitude of physicians, all with differing backgrounds and interests in transfusion practice, there is a critical need for active and effective blood utilization committees to develop, promote, and monitor best practices in blood component therapy.[135] In their role as stewards of the blood supply, blood utilization committees must function both reactively (providing blood utilization review) and proactively (formulating and implementing effective transfusion guidelines). In this latter role, blood utilization committees must serve as change agents to alter established patterns of physician behavior.[1 Pharmacist's Role Numerous examples exist where pharmacists have traditionally played a lead role in the development and implementation of policies within the institutional setting. Often such policies are restrictive in nature, involving pharmacologic agents that are particularly costly (e.g., drotrecogin alfa activated[136]) and/or have high-volume usage (e.g., antimicrobial restriction programs). In other instances, pharmacists have played an integral role within selected practice settings promoting standardization of care. Noteworthy in this regard are the development of sedation and analgesia guidelines,[137] the prevention of stress-related mucosal disease[138] and deep vein thromboses in the critical care setting,[139] and antiemetic therapy within the oncology setting.[140] Coincidentally, these are some of the same practice environments where blood products are routinely administered. In a similar manner, pharmacists are playing an active role in a blood management program in many institutions at least as it relates to the use of pharmacologic alternatives. For example, one recently described pharmacist-managed anemia program in patients with chronic kidney disease focused on initiation and adjustment of epoetin alfa and iron therapy.[141] Cost avoidance in patients monitored within this program was $3000/patient/year. Another example is the development and implementation of evidence-based protocols for erythropoiesis-stimulating agents and concurrent iron therapy in various patient populations including critically ill patients.[142] Such a program in critically ill patients reduced the mean ± SD number of red blood cell transfusions from 16.6 ± 13.1 units before the protocol to 7 ± 11.8 units after protocol implementation.[142] Noteworthy in this study was the extremely high number of transfusions in both study periods. This may have been due to patient groups having mean ICU lengths of stay of 3– 5 weeks. More recently, multiprofessional usage guidelines for rFVIIa have been published.[143–145] Although these efforts are laudable, perhaps even more important is that pharmacists focus their attention beyond those issues involving high-priced pharmacologic agents. The first step in the process of engaging pharmacists in blood management is to heighten the awareness among pharmacists as to the broader implications of allogeneic red blood cell transfusions through educational efforts such as this primer. Once this has been accomplished, pharmacists will then be well positioned to contribute their expertise to the institutional medical committee (e.g., blood utilization committee, ICU committee) responsible for development of allogeneic red blood cell transfusion guidelines. In these cases, identification of physician champions to effectively promote the establishment of evidence-based blood management policies is critical to the success of such efforts. Nevertheless, the experience of pharmacists with the development and imple-mentation of other institutional policies could prove invaluable within a particular institution in terms of the long-term success and viability of a blood management program. Furthermore, through their involvement in blood management programs from guideline development to implementation to ongoing monitoring, pharmacists will have made significant strides toward tearing down one of those silos so frequently separating health care personnel within the institutional setting. Conclusion In many cases, transfusions are the end result of the actions or inactions of health care providers and hospitals to manage a series of events in complex patients. It is encouraging to note that this series of events is predictable and, to a great extent, controllable through the use of proactive interventions collectively termed blood management. By developing and implementing comprehensive blood management programs, hospitals can promote safe, efficient, and clinically effective blood utilization practices for the benefit of the health care system, its patients, and the local community. Alternatively stated, the goal of blood management is to ensure that each and every blood product that is transfused is appropriate, and that blood-related resources are used effectively. The cornerstones of blood management programs are the implementation of evidence-based transfusion guidelines to reduce variability in transfusion practice, and the employment of multidisciplinary teams to study, implement, and monitor local blood management strategies. Pharmacists can play a key role in blood management programs by providing technical expertise as well as oversight and monitoring of pharmaceutical agents used to reduce the need for allogeneic blood. References 1. American Association of Blood Banks. The 2005 nationwide blood collection and utilization survey report. Bethesda, MD: American Association of Blood Banks; 2006:3. 2. Shulman IA, Saxena S. The transfusion services committee: responsibilities and response to adverse transfusion events. Hematology Am Soc Hematol Educ Program 2005;1:483– 90. 3. Dzik WH. Emily Cooley lecture 2002: transfusion safety in the hospital. Transfusion 2003;43:1190– 9. 4. Hebert PC, Wells G, Blajchman MA, et al, for the Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med 1999;340:409– 17. 5. Rao SV, Jollis JG, Harrington RA, et al. Relationship of blood transfusion and clinical outcomes in patients with acute coronary syndromes. JAMA 2004;292:1555– 62. 6. Vincent JL, Baron JF, Reinhart K, et al. Anemia and blood transfusion in critically ill patients. JAMA 2002;288: 1499– 507. 7. Corwin HL, Gettinger A, Pearl RG, et al. The CRIT study: anemia and blood transfusion in the critically ill—current clinical practice in the United States. Crit Care Med 2004;32:39– 52. 8. Goodnough LT, Johnston MF, Toy PT, for the Transfusion Medicine Academic Award Group. The variability of transfusion practice in coronary artery bypass surgery. JAMA 1991;265:86– 90. 9. Stover EP, Siegel LC, Body SC, et al, for the Institutions of the MultiCenter Study of Perioperative Ischemia Research Group. Institutional variability in red blood cell conservation practices for coronary artery bypass graft surgery. J Cardiothorac Vasc Anesth 2000;14:171– 6. 10. Audet AM, Andrzejewski C, Popovsky MA. Red blood cell transfusion practices in patients undergoing orthopedic surgery: a multi-institutional analysis. Orthopedics 1998;21:851– 8. 11. Poses RM, Berlin JA, Noveck H, et al. How you look determines what you find: severity of illness and variation in blood transfusion for hip fracture. Am J Med 1998;105: 198– 206. 12. Spiess BD. Choose one: damned if you do/damned if you don't! Crit Care Med 2005;33:1871– 4. 13. Spiess BD. Blood transfusion: the silent epidemic. Ann Thorac Surg 2001;72:51832– 7. 14. Shulman IA, Shander A. Serious acute transfusion reactions. In: Spiess BD, Spence RK, Shander A, eds. Perioperative transfusion medicine. Philadelphia: Lippincott Williams & Wilkins, 2005:169– 75. 15. Goodnough LT. Risks of blood transfusion. Crit Care Med 2003;31:S678– 86. 16. Linden JV, Paul B, Dressler KP. A report of 104 transfusion errors in New York State. Transfusion 1992;32:601– 6. 17. Linden JV, Wagner K, Voytovich AE, Sheehan J. Transfusion errors in New York State: an analysis of 10 years' experience. Transfusion 2000;40:1207– 13. 18. Forgie MA, Wells PS, Laupacis A, Fergusson D, for the International Study of Perioperative Transfusion (ISPOT) Investigators. Preoperative autologous donation decreases allogeneic transfusion but increases exposure to all red blood cell transfusion: results of a meta-analysis. Arch Intern Med 1998;158:610– 16. 19. Tinmouth A, Fergusson D, Yee IC, Hebert PC. Clinical consequences of red cell storage in the critically ill. Transfusion 2006;46:2014– 27. 20. Kristiansson M, Soop M, Saraste L, Sundqvist KG. Cytokines in stored red blood cell concentrates: promoters of systemic inflammation and simulators of acute transfusion reactions? Acta Anaesthesiol Scand 1996;40:496– 501. 21. Suttner S, Piper SN, Kumle B, et al. The influence of allogeneic red blood cell transfusion compared with 100% oxygen ventilation on systemic oxygen transport and skeletal muscle oxygen tension after cardiac surgery. Anesth Analg 2004;99:2– 11. 22. Tsai AG, Cabrales P, Intaglietta M. Microvascular perfusion upon exchange transfusion with stored red blood cells in normovolemic anemic conditions. Transfusion 2004;44: 1626– 34. 23. Marik PE, Sibbald WJ. Effect of stored-blood transfusion on oxygen delivery in patients with sepsis. JAMA 1993;269: 3024– 9. 24. Silliman CC, Ambruso DR, Boshkov LK. Transfusion-related acute lung injury. Blood 2005;105:2266– 73. 25. Fransen E, Maessen J, Dentener M, et al. Impact of blood transfusions on inflammatory mediator release in patients undergoing cardiac surgery. Chest 1999;116:1233– 9. 26. Toy P, Popovsky MA, Abraham E, et al. Transfusion-related acute lung injury: definition and review. Crit Care Med 2005;33:721– 6. 27. Boshkov LK. Transfusion-related acute lung injury and the ICU. Crit Care Clin 2005;21:479– 95. 28. Popovsky MA. Transfusion-related acute lung injury. Transfusion 1995;35:180– 1. 29. Eder AF, Herron R, Strupp A, et al. Transfusion-related acute lung injury surveillance (2003– 2005) and the potential impact of the selective use of plasma from male donors in the American Red Cross. Transfusion 2007;47:599– 607. 30. Blumberg N. Deleterious clinical effects of transfusion immunomodulation: proven beyond a reasonable doubt. Transfusion 2005;45:S33– 9. 31. Blumberg N, Heal JM. Immunomodulation by blood transfusion: an evolving scientific and clinical challenge. Am J Med 1996;101:299– 308. 32. Triulzi DJ, Vanek K, Ryan DH, Blumberg N. A clinical and immunologic study of blood transfusion and postoperative bacterial infection in spinal surgery. Transfusion 1992;32: 517– 24. 33. Carson JL, Altman DG, Duff A, et al. Risk of bacterial infection associated with allogeneic blood transfusion among patients undergoing hip fracture repair. Transfusion 1999;39:694– 700. 34. Leal-Noval SR, Rincon-Ferrari MD, Garcia-Curiel A, et al. Transfusion of blood components and postoperative infection in patients undergoing cardiac surgery. Chest 2001;119: 1461– 8. 35. Agarwal N, Murphy JG, Cayten CG, Stahl WM. Blood transfusion increases the risk of infection after trauma. Arch Surg 1993;128:171– 6. 36. Claridge JA, Sawyer RG, Schulman AM, et al. Blood transfusions correlate with infections in trauma patients in a dose-dependent manner. Am Surg 2002;68:566– 72. 37. Houbiers JG, van de Velde CJ, van de Watering LM, et al. Transfusion of red cells is associated with increased incidence of bacterial infection after colorectal surgery: a prospective study. Transfusion 1997;37:126– 34. 38. Taylor RW, Manganaro L, O'Brien J, et al. Impact of allogenic packed red blood cell transfusion on nosocomial infection rates in the critically ill patient. Crit Care Med 2002;30:2249– 54. 39. Shorr AF, Duh MS, Kelly KM, Kollef MH. Red blood cell transfusion and ventilatorassociated pneumonia: a potential link? Crit Care Med 2004;32:666– 74. 40. Hill GE, Frawley WH, Griffith KE, et al. Allogeneic blood transfusion increases the risk of postoperative bacterial infection: a meta-analysis. J Trauma 2003;54:908– 14. 41. Moore FA, Moore EE, Sauaia A. Blood transfusion: an independent risk factor for postinjury multiple organ failure. Arch Surg 1997;132:620– 4. 42. Shapiro MJ, Gettinger A, Corwin HL, et al. Anemia and blood transfusion in trauma patients admitted to the intensive care unit. J Trauma 2003;55:269– 73. 43. Malone DL, Dunne J, Tracy JK, et al. Blood transfusion, independent of shock severity, is associated with worse outcome in trauma. J Trauma 2003;54:898– 905. 44. Vamvakas EC, Carven JH. RBC transfusion and postoperative length of stay in the hospital or the intensive care unit among patients undergoing coronary artery bypass graft surgery: the effects of confounding factors. Transfusion 2000;40:832– 9. 45. Langley SM, Alexiou C, Bailey DH, Weeden DF. The influence of perioperative blood transfusion on survival after esophageal resection for carcinoma. Ann Thorac Surg 2002;73:1704– 9. 46. Landers DF, Hill GE, Wong KC, Fox IJ. Blood transfusion-induced immunomodulation. Anesth Analg 1996;82:187– 204. 47. Vamvakas EC. Transfusion-associated cancer recurrence and postoperative infection: meta-analysis of randomized, controlled clinical trials. Transfusion 1996;36:175– 86. 48. Blumberg N, Heal JM. Effects of transfusion on immune function: cancer recurrence and infection. Arch Pathol Lab Med 1994;118:371– 9. 49. Habib RH, Zacharias A, Schwann TA, et al. Role of hemodilutional anemia and transfusion during cardio-pulmonary bypass in renal injury after coronary revascularization: implications on operative outcome. Crit Care Med 2005;33:1749– 56. 50. Spiess BD, Shander A. The transfusion decision. In: Spiess BD, Spence RK, Shander A. eds. Perioperative transfusion medicine. Philadelphia: Lippincott Williams & Wilkins, 2005:659– 65. 51. Spiess BD. Risks of transfusion: outcome focus. Transfusion 2004;44:S4– 14. 52. Nelson AH, Fleisher LA, Rosenbaum SH. Relationship between postoperative anemia and cardiac morbidity in high-risk vascular patients in the intensive care unit. Crit Care Med 1993;21:860– 6. 53. Hebert PC, Wells G, Tweeddale M, et al, for the Transfusion Requirements in Critical Care (TRICC) Investigators and the Canadian Critical Care Trials Group. Does transfusion practice affect mortality in critically ill patients? Am J Respir Crit Care Med 1997;155:1618– 23. 54. Hall MA, Bobinski MA, Orentlicher D. Informed consent, health care law and ethics. 6th ed. New York: Aspen, 2003. 55. Chan T, Eckert K, Venesoen P, et al. Consenting to blood: what do patients remember? Transfus Med 2005;15:461– 6. 56. The Joint Commission. National patient safety goals. Joint Commission perspectives. Oak Brook Terrace, IL: Joint Commission, 2006. 57. Code of Federal Regulations. Conditions of participation for hospitals. Medical record services. Title 42 CFR, section 482.24 (c)(2)(v), 2006. 58. The Joint Commission. Accreditation manual for hospitals. Oakbrook Terrace, IL: Joint Commission, 2006. 59. Goodman C, Chan S, Collins P, et al. Ensuring blood safety and availability in the US: technological advances, costs, and challenges to payment—final report. Transfusion 2003;43:S3– 46. 60. Cremieux PY, Barrett B, Anderson K, Slavin MB. Cost of outpatient blood transfusion in cancer patients. J Clin Oncol 2000;18:2755– 61. 61. Cantor SB, Hudson DV Jr, Lichtiger B, Rubenstein EB. Costs of blood transfusion: a process-flow analysis. J Clin Oncol 1998;16:2364– 70. 62. Mohandas K, Aledort L. Transfusion requirements, risks, and costs for patients with malignancy. Transfusion 1995;35: 427– 30. 63. U.S. Department of Labor, Bureau of Labor Statistics. Consumer price index. Available from http://data.bls.gov/cgi-bin/surveymost?cu. Accessed March 28, 2007. 64. Dexter F, Blake JT, Penning DH, et al. Use of linear programming to estimate impact of changes in a hospital's operating room time allocation on perioperative variable costs. Anesthesiology 2002;96:718– 24. 65. Engoren M, Arslanian-Engoren C, Steckel D, et al. Cost, outcome, and functional status in octogenarians and septuagenarians after cardiac surgery. Chest 2002;122: 1309– 15. 66. Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med 2005;33:1266– 71. 67. Sonnenberg FA, Gregory P, Yomtovian R, et al. The cost-effectiveness of autologous transfusion revisited: implications of an increased risk of bacterial infection with allogeneic transfusion. Transfusion 1999;39:808– 17. 68. Silvestry SC, Smith PK. Current status of cardiac surgery in the abciximab-treated patient. Ann Thorac Surg 2000;70:S12– 19. 69. Blumberg N, Kirkley SA, Heal JM. A cost analysis of autologous and allogeneic transfusions in hip-replacement surgery. Am J Surg 1996;171:324– 30. 70. Moulton MJ, Creswell LL, Mackey ME, et al. Reexploration for bleeding is a risk factor for adverse outcomes after cardiac operations. J Thorac Cardiovasc Surg 1996;111:1037– 46. 71. Unsworth-White MJ, Herriot A, Valencia O, et al. Resternotomy for bleeding after cardiac operation: a marker for increased morbidity and mortality. Ann Thorac Surg 1995;59:664– 7. 72. Spahn DR, Casutt M. Eliminating blood transfusions: new aspects and perspectives. Anesthesiology 2000;93:242– 55. 73. Corwin HL. Anemia in the critically ill: the role of erythropoietin. Semin Hematol 2001;38:24– 32. 74. Corwin HL, Parsonnet KC, Gettinger A. RBC transfusion in the ICU. Is there a reason? Chest 1995;108:767– 71. 75. Pola E, Papaleo P, Santoliquido A, et al. Clinical factors associated with an increased risk of perioperative blood transfusion in nonanemic patients undergoing total hip arthroplasty. J Bone Joint Surg Am 2004;86A:57– 61. 76. Massicotte L, Sassine MP, Lenis S, Roy A. Transfusion predictors in liver transplant. Anesth Analg 2004;98:1245– 51. 77. Magovern JA, Sakert T, Magovern GJ, et al. A model that predicts morbidity and mortality after coronary artery bypass graft surgery. J Am Coll Cardiol 1996;28:1147– 53. 78. Moskowitz DM, Klein JJ, Shander A, et al. Predictors of transfusion requirements for cardiac surgical procedures at a blood conservation center. Ann Thorac Surg 2004;77:626– 34. 79. Ang-Lee MK, Moss J, Yuan CS. Herbal medicines and perioperative care. JAMA 2001;286:208– 16. 80. Shander A, Knight K, Thurer R, et al. Prevalence and outcomes of anemia in surgery: a systematic review of the literature. Am J Med 2004;116 (suppl 7A):S58– 69. 81. Fowler RA, Berenson M. Blood conservation in the intensive care unit. Crit Care Med 2003;31:S715– 20. 82. Smoller BR, Kruskall MS. Phlebotomy for diagnostic laboratory tests in adults: pattern of use and effect on transfusion requirements. N Engl J Med 1986;314:1233– 5. 83. Carless PA, Henry DA, Moxey AJ, et al. Cell salvage for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 2003;(4):CD001888. 84. Shander A. Surgery without blood. Crit Care Med 2003;31:S708– 14. 85. Pieracci FM, Barie PS. Diagnosis and management of iron-related anemias in critical illness. Crit Care Med 2006;34: 1898– 905. 86. Rudis MI, Jacobi J, Hassan E, Dasta JF. Managing anemia in the critically ill patient. Pharmacotherapy 2004;24:229– 47. 87. Alam MG, Krause MW, Shah SV. Parenteral iron therapy: beyond anaphylaxis. Kidney Int 2004;66:457– 8. 88. Macdougall IC, Eckardt KU. Novel strategies for stimulating erythropoiesis and potential new treatments for anaemia. Lancet 2006;368:947– 53. 89. Siddiqui MA, Keating GM. Darbepoetin alfa: a review of its use in the treatment of anaemia in patients with cancer receiving chemotherapy. Drugs 2006;66:997– 1012. 90. Henry DH, Bowers P, Romano MT, Provenzano R. Epoetin alfa: clinical evolution of a pleiotropic cytokine. Arch Intern Med 2004;164:262– 76. 91. Steensma DP, Loprinzi CL. Epoetin alfa and darbepoetin alfa go head to head. J Clin Oncol 2006;24:2233– 6. 92. Glaspy J, Vadhan-Raj S, Patel R, et al. Randomized comparison of every-2-week darbepoetin alfa and weekly epoetin alfa for the treatment of chemotherapy-induced anemia: the 20030125 study group trial. J Clin Oncol 2006;24:2290– 7. 93. Zhang Y, Thamer M, Stefanik K, et al. Epoetin requirements predict mortality in hemodialysis patients. Am J Kidney Dis 2004;44:866– 76. 94. U.S. Food and Drug Administration, Center for Drug Evaluation and Research. Information for healthcare professionals. Erythropoiesis stimulating agents (ESA). Online posting March 9, 2007. Available from http://www. fda.gov/cder/drug/InfoSheets/HCP/RHE2007HCP.htm. Accessed March 21, 2007. 95. Napolitano LM. Perioperative anemia. Surg Clin North Am 2005;85:1215– 27. 96. Shander A, Goodnough LT. Objectives and limitations of bloodless medical care. Curr Opin Hematol 2006;13:462– 70. 97. Pajoumand M, Erstad BL, Camamo JM. Use of epoetin alfa in critically ill patients. Ann Pharmacother 2004;38:641– 8. 98. Givens M, Lapointe M. Is there a place for epoetin alfa in managing anemia during critical illness? Clin Ther 2004;26:819– 29. 99. Gabriel A, Kozek S, Chiari A, et al. High-dose recombinant human erythropoietin stimulates reticulocyte production in patients with multiple organ dysfunction syndrome. J Trauma 1998;44:361– 7. 100. van Iperen CE, Gaillard CA, Kraaijenhagen RJ, et al. Response of erythropoiesis and iron metabolism to recombinant human erythropoietin in intensive care unit patients. Crit Care Med 2000;28:2773– 8. 101. Corwin HL, Gettinger A, Rodriguez RM, et al. Efficacy of recombinant human erythropoietin in the critically ill patient: a randomized, double-blind, placebo-controlled trial. Crit Care Med 1999;27:2346– 50. 102. Corwin HL, Gettinger A, Pearl RG, et al. Efficacy of recombinant human erythropoietin in critically ill patients: a randomized controlled trial. JAMA 2002;288:2827– 35. 103. Still JM Jr, Belcher K, Law EJ, et al. A double-blinded prospective evaluation of recombinant human erythropoietin in acutely burned patients. J Trauma 1995;38:233– 6. 104. Silver M, Corwin MJ, Bazan A, et al. Efficacy of recombinant human erythropoietin in critically ill patients admitted to a long-term acute care facility: a randomized, double-blind, placebo-controlled trial. Crit Care Med 2006;34:2310– 16. 105. Drews RE. Critical issues in hematology: anemia, thrombocytopenia, coagulopathy, and blood product transfusions in critically ill patients. Clin Chest Med 2003;24:607– 22. 106. Spahn DR, Rossaint R. Coagulopathy and blood component transfusion in trauma. Br J Anaesth 2005;95:130– 9. 107. Gottschall J, ed. Blood transfusion therapy: a physicians handbook. 8th ed. Bethesda, MD: American Association of Blood Banks, 2006. 108. Ketchum L, Hess JR, Hiippala S. Indications for early fresh frozen plasma, cryoprecipitate, and platelet transfusion in trauma. J Trauma 2006;60:S51– 8. 109. Barletta JF, Ahrens CL, Tyburski JG, Wilson RF. A review of recombinant factor VII for refractory bleeding in nonhemophilic trauma patients. J Trauma 2005;58:646– 51. 110. Boffard KD, Riou B, Warren B, et al. Recombinant factor VIIa as adjunctive therapy for bleeding control in severely injured trauma patients: two parallel randomized, placebo-controlled, double-blind clinical trials. J Trauma 2005; 59:8– 15. 111. Alexander E. Emerging role of recombinant factor VIIa in neuroscience. Am Assoc Crit Care Nurses Adv Crit Care 2006;17:363– 7. 112. Franchini M, Zaffanello M, Veneri D. Recombinant factor VIIa: an update on its clinical use. Thromb Haemost 2005;93:1027– 35. 113. Sobieszczyk S, Breborowicz GH, Platicanov V, et al. Recombinant factor VIIa in the management of postpartum bleeds: an audit of clinical use. Acta Obstet Gynecol Scand 2006;85:1239– 47. 114. O'Connell KA, Wood JJ, Wise RP, et al. Thromboembolic adverse events after use of recombinant human coagulation factor VIIa. JAMA 2006;295:293– 8. 115. Levi M, Peters M, Buller HR. Efficacy and safety of recombinant factor VIIa for treatment of severe bleeding: a systematic review. Crit Care Med 2005;33:883– 90. 116. Carless PA, Henry DA, Moxey AJ, et al. Desmopressin for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 2004;(1):CD001884. 117. Henry DA, Moxey AJ, Carless PA, et al. Anti-fibrinolytic use for minimising perioperative allogeneic blood transfusion. Cochrane Database Syst Rev 2001;(1):CD001886. 118. Mangano DT, Tudor IC, Dietzel C. The risk associated with aprotinin in cardiac surgery. N Engl J Med 2006;354:353– 65. 119. Moore EE, Johnson JL, Cheng AM, et al. Insights from studies of blood substitutes in trauma. Shock 2005;24: 197– 205. 120. Spahn DR, Kocian R. Artificial O2 carriers: status in 2005. Curr Pharm Des 2005;11:4099– 114. 121. Stollings JL, Oyen LJ. Oxygen therapeutics: oxygen delivery without blood. Pharmacotherapy 2006;26:1453– 64. 122. Creteur J, Vincent JL. Hemoglobin solutions. Crit Care Med 2003;31:S698– 707. 123. Goodnough LT, Price TH, Rudnick S, Soegiarso RW. Preoperative red cell production in patients undergoing aggressive autologous blood phlebotomy with and without erythropoietin therapy. Transfusion 1992;32:441– 5. 124. Bierbaum BE, Callaghan JJ, Galante JO, et al. An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am 1999;81:2– 10. 125. Gould SA, Forbes JM. Controversies in transfusion medicine: indications for autologous and allogeneic transfusion should be the same: pro. Transfusion 1995;35:446– 9. 126. Billote DB, Glisson SN, Green D, Wixson RL. A prospective, randomized study of preoperative autologous donation for hip replacement surgery. J Bone Joint Surg Am 2002;84A: 1299– 304. 127. Pierson JL, Hannon TJ, Earles DR. A blood-conservation algorithm to reduce blood transfusions after total hip and knee arthroplasty. J Bone Joint Surg Am 2004;86A:1512– 18. 128. Goodnough LT, Soegiarso RW, Birkmeyer JD, Welch HG. Economic impact of inappropriate blood transfusions in coronary artery bypass graft surgery. Am J Med 1993;94: 509– 14. 129. Carson JL, Hill S, Carless P, et al. Transfusion triggers: a systematic review of the literature. Transfus Med Rev 2002;16:187– 99. 130. Institute of Medicine, Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st Century. Washington, DC: National Academy Press, 2001. 131. Tinmouth A, Macdougall L, Fergusson D, et al. Reducing the amount of blood transfused: a systematic review of behavioral interventions to change physicians' transfusion practices. Arch Intern Med 2005;165:845– 52. 132. Rana R, Afessa B, Keegan MT, et al. Evidence-based red cell transfusion in the critically ill: quality improvement using computerized physician order entry. Crit Care Med 2006;34:1892– 7. 133. Geertsma RH, Parker RC Jr, Whitbourne SK. How physicians view the process of change in their practice behavior. J Med Educ 1982;57:752– 61. 134. Klein HG. Blood avoidance for the critically ill: another blow to liberalism? Crit Care Med 2006;34:2013– 14. 135. Hannon TJ. Transfusion guidelines: development and impact on blood management. In: Saxena S, Shulman IA. eds. The transfusion committee: putting patient safety first. Bethesda, MD: American Association of Blood Banks Press, 2006:115– 29. 136. Wong-Beringer A, Liao C, Nguyen M, Pallares J. Applying patient selection criteria for drotrecogin alfa therapy in practice. Am J Health-Syst Pharm 2003;60:1345– 52. 137. Jacobi J, Fraser GL, Coursin DB, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002;30:119– 41. 138. Allen ME, Kopp BJ, Erstad BL. Stress ulcer prophylaxis in the postoperative period. Am J Health-Syst Pharm 2004;61:588– 96. 139. Devlin JW, Tyburski JG, Moed B. Implementation and evaluation of guidelines for use of enoxaparin as deep vein thrombosis prophylaxis after major trauma. Pharmacotherapy 2001;21:740– 7. 140. Dranitsaris G, Leung P, Warr D. Implementing evidence based antiemetic guidelines in the oncology setting: results of a 4-month prospective intervention study. Support Care Cancer 2001;9:611– 18. 141. Walton T, Holloway K, Knaus M. Pharmacist-managed anemia program in an outpatient hemodialysis population. Hosp Pharm 2005;40:1051– 6. 142. Pell LJ, Martin BS, Shirk MB. Epoetin alfa protocol and multidisciplinary bloodconservation program for critically ill patients. Am J Health-Syst Pharm 2005;62:400– 5. 143. Martinowitz U, Michaelson M. Guidelines for the use of recombinant activated factor VII (rFVIIa) in uncontrolled bleeding: a report by the Israeli multidisciplinary rFVIIa task force. J Thromb Haemost 2005;3:640– 8. 144. Rudisill CN, Hockman RH, Degregory KA, et al. Implementing guidelines for the institutional use of factor VIIa (recombinant): a multidisciplinary solution. Am J HealthSyst Pharm 2006;63:1641– 6. 145. Shander A, Goodnough LT, Ratko T, et al. Consensus recommendations for the off– label use recombinant human factor VIIa (NovoSeven) therapy. Pharm Ther 2005;30: 644– 58.