Detailed-outline-of-Diabetes-course
advertisement
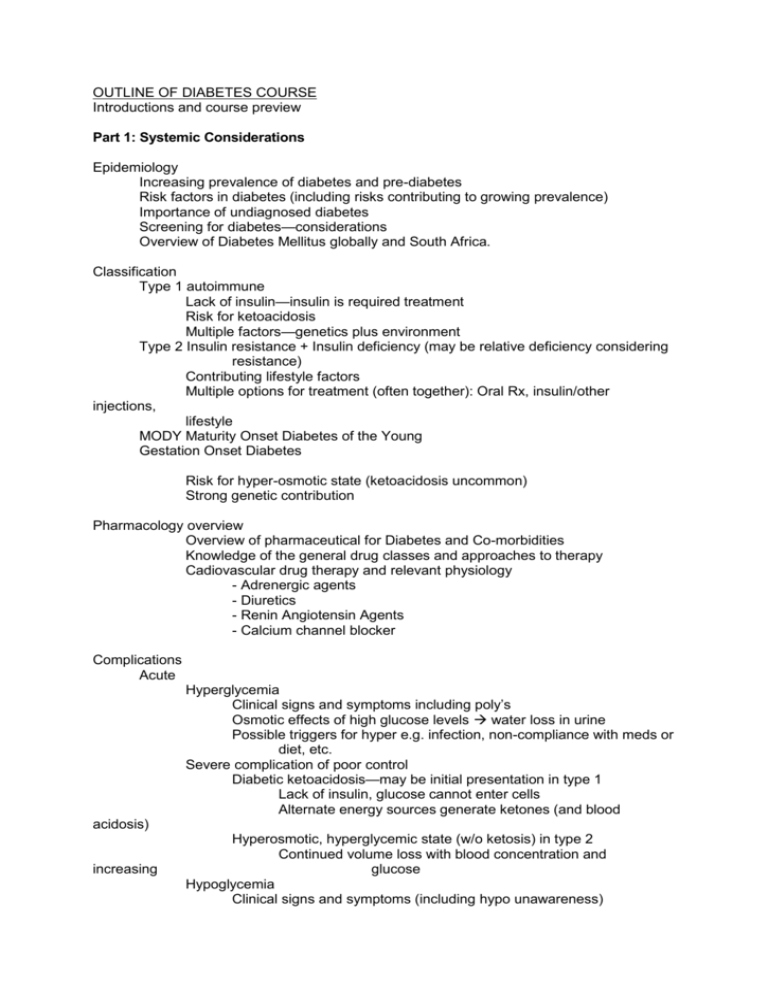
OUTLINE OF DIABETES COURSE Introductions and course preview Part 1: Systemic Considerations Epidemiology Increasing prevalence of diabetes and pre-diabetes Risk factors in diabetes (including risks contributing to growing prevalence) Importance of undiagnosed diabetes Screening for diabetes—considerations Overview of Diabetes Mellitus globally and South Africa. Classification Type 1 autoimmune Lack of insulin—insulin is required treatment Risk for ketoacidosis Multiple factors—genetics plus environment Type 2 Insulin resistance + Insulin deficiency (may be relative deficiency considering resistance) Contributing lifestyle factors Multiple options for treatment (often together): Oral Rx, insulin/other injections, lifestyle MODY Maturity Onset Diabetes of the Young Gestation Onset Diabetes Risk for hyper-osmotic state (ketoacidosis uncommon) Strong genetic contribution Pharmacology overview Overview of pharmaceutical for Diabetes and Co-morbidities Knowledge of the general drug classes and approaches to therapy Cadiovascular drug therapy and relevant physiology - Adrenergic agents - Diuretics - Renin Angiotensin Agents - Calcium channel blocker Complications Acute Hyperglycemia Clinical signs and symptoms including poly’s Osmotic effects of high glucose levels water loss in urine Possible triggers for hyper e.g. infection, non-compliance with meds or diet, etc. Severe complication of poor control Diabetic ketoacidosis—may be initial presentation in type 1 Lack of insulin, glucose cannot enter cells Alternate energy sources generate ketones (and blood acidosis) increasing Hyperosmotic, hyperglycemic state (w/o ketosis) in type 2 Continued volume loss with blood concentration and glucose Hypoglycemia Clinical signs and symptoms (including hypo unawareness) Inverse relationship of hypo incidence (more with tight control) to DM complications Avoidance Treatment Patient able to eat—oral sugar (glucose ideal) followed by complex carbohydrate to prevent recurrent hypoglycemia Patient unconscious—glucagon injection or IV fluid with dextrose Long Term Microvascular Ocular Focus as it relates to co-morbidity coincidence with other vascular conditions Renal Onset in type 1 not before 5 years Renal disease may be present in type 2 at diagnosis Factors contributing to DM often renal disease comorbidities (e.g. HTN) Renal disease (including proteinuria) is a risk factor for cardiovascular mortality Screening: Annual urine albumin/creatinine ratio for all diabetic patients Monitoring: If albuminuria is present, regular monitoring Risk factor reduction: BP control, smoking cessation, DM control Treatment for albuminuria/proteinuria to reduce risk of progression: ACE-inhibitors or ARB (angiotensin II receptor blockers) Correlation with retinopathy Neurological Peripheral neuropathy (“stocking/glove”) Sensory loss, motor weakness, painful Consequences: pressure sore, ulcer, infection, gangrene, amputation Autonomic neuropathy Gastrointestinal, cardiovascular, genitourinary Peripheral mononeuropathy Management, prevention: Glucose control, vascular risk factor reduction Foot care and monitoring, never go barefoot Macrovascular Peripheral vascular disease Ischemic cardiac disase Cerebrovascular disease For each: Comorbidities Presentations (symptoms, findings) Treatment Skin conditions (key conditions for exam focus) Infectious Metabolic Complications of insulin therapy Cardiovascular co-morbidities—atherosclerosis, hyperlipidemia, hypertension Pathogenesis of atherosclerotic lesion; key concepts: Fatty streak (initial lesion, onset may be early in life with risk factors) Advanced atherosclerotic lesion develops fibrous cap which is prone to rupture Rupture results in platelet aggregation and potential vessel occlusion resulting in ischemic event (e.g. heart attack) Fibrous cap may stabilize and lower risk for rupture with control of lipids, BP, improved lifestyle Risk factors Age/gender aggregate Serum lipoproteins (clinical focus) Clinical signs (focus on ocular) Role of lipid lowering agents: Focus on statin drugs (primary and secondary prevention) Role of screening (guidelines vary, key issue—screening is recommended for “at risk” population) General understanding of risk reduction schema (consider aggregate of “traditional” risk factors) More aggressive goals for higher risk; diabetes is considered in highest risk strata Aspirin therapy Benefit of anti-platelet effects in cardiovascular risk reductions Risk of adverse effects—primarily gastrointestinal ulceration and bleeding (ulcers or elsewhere) Hypertension (HTN) Substantial worldwide prevalence and increasing (epidemiologic #’s not critical for exam) Major risk for heart attack and stroke across the globe Prevalence of: Undiagnosed HTN and Untreated HTN Important to know BP cut-offs for pre-hypertension and stages 1 and 2 Hypertensive urgency (timely medical office visit) vs. malignant hypertension (call medics- emergency) Essential HTN Secondary HTN End organ effects of chronic HTN Co-morbid risk factors (for risk stratification) Treatment Lifestyle modification (including low sodium diet) Drug treatment—4 major drug classes in common clinical use (think ABCD) A= ACE-inhibitors, Angiotensin 2 receptor-blockers (ARB) B= Beta-blockers C= Calcium channel blockers D= Diuretics (thiazide class is major one in use) Misc: Alpha (adrenergic)-blockers—useful also treating prostrate obstruction in older men Key factor in diabetes—lower BP treatment goal ---Metabolic syndrome ----Lifestyle Evidence based Medicine in DM: Key clinical studies Some examples a. Action to Control Cardiovascular risk in Diabetes (ACCORD) b. Action in Diabetes and Cardiovascular Disease (ADVANCE) c. d. e. United Kingdom Prospective Diabetes Study (UKPDS) Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Steno Diabetes Center- Copenhagen Primary care of diabetes Review overlap with specific management of diabetes complications, co-morbidities and therapies including: Tobacco Diet and weight management Drug treatments (see above) Lifestyle management options Pulmonary Risk for pneumonia and influenza complications Role of vaccination in prevention Dental Role of chronic dental infections in complicating diabetes control Role of poorly controlled diabetes in making dental infections more difficult to control Case studies are used to illustrate principles of medical intervention and increased optometric participation in co-managed patient care. Part 2: Ocular Consideration Epidemiology and overview of DM related to Ocular complications I. Diabetes Mellitus and Blindness a. Vision loss from Diabetes Retinopathy 1. Non-resolving Vitreous Hemorrhage 2. Fibrovascular Proliferation with Traction Retinal Detachment 3. Diabetic Macular Edema b. Incidence and Prevalence Statistics Part 2A:Ocular Considerations – Non-retinal Ocular Complications 1. II. Review of Anterior Segment Complications of DM a. Orbital/periorbital- xanthalasma, peri-orbital edema, mucormycosis b. Cornea – corneal abrasions, recurrent erosions, contact lens, lasik surgery c. Iris- complication d. Lens/cataract extraction e. Glaucoma f. Mono-neuropathy – pupil and cranial nerve III and VI Part 2B: Ocular Considerations - Retinal Ocular Complications III. Clinical Risks Factors (influencing rate of progression of diabetic eye disease) a. Duration of Diabetes i. Type 1 ii. Type 2 b. Control of Hyperglycemia – DCCT c. Diabetic Nephropathy d. e. f. g. Hypertension Pregnancy Ocular Surgery Serum Cholesterol IV. Clinical Pathologic Processes in Diabetic Retinopathy a. Loss of pericytes of retinal capillaries b. Out-pouching of capillary walls to form microaneurysms c. Closure of retinal capillaries and arterioles d. Breakdown of the blood/retinal barrier with increased vascular permeability of retinal capillaries e. Proliferation of new vessels and fibrous tissue f. Contraction of vitreous and fibrous proliferation with subsequent vitreous hemorrhage and retinal detachment. V. Implications of Lesions of Diabetic Retinopathy a. Venous Caliber Abnormalities b. Intraretinal Microvascular Abnormalities (IRMA) c. Cotton Wool Spots (Soft Exudates) d. Hemorrhages and Microaneurysms (H/Ma) e. Hard Exudates f. Non-perfusion of the Retina g. Macular Edema VI. Laser Photocoagulation of the Retina and Choroid a. Basic Information b. Photocoagulation c. Therapeutic Rationale d. Ocular Chromophores e. Ophthalmic Laser Characteristics f. Clinical Application g. Laser Delivery Systems g. Vein Occlusion Study h. Focal Laser Treatment i. Scatter (PRP) Treatment j. Patient Care k. Follow-up care l. Complications of laser surgery VII. Clinical Considerations a. Levels of Diabetic Retinopathy i. ETDRS Standard Photographs ii. Risk/Rate of Progression by Levels to PDR and High Risk PDR iii. High Risk Characteristics (HRC) iv. Diabetic Macular Edema--May be present at any level of Diabetic Retinopathy v. Clinically Significant Macular Edema (CSME) VIII. Diabetic Effects on Macular Structure and Function a. Macular Edema b. Non-perfusion of parafoveal capillaries, with or without intraretinal fluid c. Traction in the macula by fibrous tissue proliferation causing dragging of the retinal tissue, surface wrinkling, or detachment of the macula d. Intraretinal or pre-retinal hemorrhage in the macula e. Lamellar or full thickness retinal hole formation f. Combination of the above IX. Treatment modalities for Diabetic retinopathy X. Considerations for vitrectomy m. Non-resolving vitreous hemorrhage n. Traction retinal detachment threatening the macula o. Severe vascular and/or fibrous proliferations p. Unsatisfactory response to laser surgery q. Psycho-social considerations Part 2C. Evidence-based diabetes care on retina I. Diabetic Retinopathy: Clinical trials and science behind the care a. Diabetic Retinopathy Study (DRS) i. Inclusion/exclusion criteria ii. Outcomes measures/endpoints iii. Results/endpoints b. Early Treatment Diabetic Retinopathy Study (ETDRS) i. Laser for macular edema ii. Early treatment for diabetic retinopathy iii. Aspirin effects on progression of retinopathy II. Diabetic Retinopathy Clinical Research Network (DRCR.net) – newer studies a. NEI funded diabetes eye research collaborative b. Established in 2002 c. Summary of DRCR Recently completed studies i. A Pilot Study of Laser Photocoagulation for Diabetic Macular Edema ii. A Randomized Trial Comparing Intravitreal Triamcinolone Acetonide and Laser Photocoagulation for Diabetic Macular Edema iii. Evaluation of Vitrectomy for Diabetic Macular Edema Study iv. A Pilot Study of Peribulbar Triamcinolone Acetonide for Diabetic Macular Edema v. Temporal Variation in Optical Coherence Tomography Measurements of Retinal Thickening in Diabetic Macular Edema vi. A Phase 2 Evaluation of Anti-VEGF Therapy for Diabetic Macular Edema: Bevacizumab vii. An Observational Study of the Development of Diabetic Macular Edema Following Scatter Laser Photocoagulation viii. Subclinical Diabetic Macular Edema Study Part 3: Non -Pharmacological Treatments Part 3A: Nutrition Fundamentals of nutrition Treat to target goals: Blood pressure, A1C%, cholesterol etc. Effectiveness of Medical Nutrition Therapy (MNT). guidelines Short and long term affects of weight loss and clinical outcomes Nutrients: micro and macronutrients and affect Affect of food on blood glucose Portions and how much should one eat: carbohydrate, protein, fat Meal planning and carbohydrate counting Insulin and carbohydrate calculations Affects of Alcohol Part 3B: Physical activity Affects in Preventing related diabetes and other comorbidities Younger and Aging adult Type 1 diabetics and affects of physical activity Type 2 diabetics and affects of physical activity Acute benefits and risks of physical activity on DM Long term complications of diabetes and affects of physical activity on DM Aerobic, Anaerobic, strength training, muscle toning – affects Part 3C: Behavior Change Strategies How does Diabetes affect the patient? Patient centered approach and guidance/support Develop a plan with the patient Commitment to the plan What should a patient do if they encounter low blood sugar? Technology support for change strategies Part 3D: Interdisciplinary aspects and importance of community care and screening Resources within South Africa . Part 4A and 4B Workshops: Diabetic retinopathy image acquisition/image review workshop Workshop designed to prepare and certify the eye care professional in all aspects of digital image acquisition, interpretation and diagnosing level of diabetic retinopathy. Workshop designed review the lesions and clinical levels of diabetic retinopathy and diabetic macular edema to determine clinical management. This portion of the program prepares the primary care optometrist to make appropriate diagnostic decisions and to provide guidelines in managing various levels of diabetic retinopathy and diabetic macular edema. Part 5A and B Workshops: From theory to Practice: Diet management, monitoring and maintenance of blood glucose levels Workshop A: Diet control, carbohydrate counting and self monitoring These are important component of diabetes self management. This interactive workshop is designed to instruct the primary care optometry on various elements of diabetes self management. Integrate the material from lecture on nutrition and help them with meal planning Healthy heart meal planning Monitoring matters: pattern management Workshop B: Monitoring Matters: Pattern Management The participant will learn how to test blood glucose levels with conventional glucometers, and test their ability to inject physiological saline in place of insulin. They will develop an understanding of what tools can be used: pump, pen, needles a. b. c. i. ii. iii. iv. v. Introduction to self-management Types of glucometers 1. Glucometer strips 2. Standardized measurements 3. Calibration Review of types of insulin Types of administration Complications 1. Injection site 1. Hypoglycemia 2. Emergency management and treatment Carbohydrate counting 1. Nature of carbohydrates 2. Instructing the patient 3. Insulin use and meals Costs, availability, disposability Foot management, guidelines and management.