Perianal Abscess: Introduction - Dis Lair
advertisement

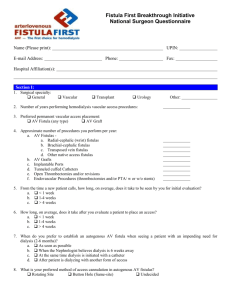
Perianal Abscess: Introduction A perianal abscess represents an infection of the soft tissues surrounding the anal canal, with formation of a discrete abscess cavity. The severity and depth of the abscess are quite variable, and the abscess cavity is often associated with formation of a fistulous tract. For that reason, along with perianal abscess, perianal fistula also is discussed in this article. Problem An anorectal abscess originates from an infection arising in the cryptoglandular epithelium lining the anal canal. The internal anal sphincter is believed to serve normally as a barrier to infection passing from the gut lumen to the deep perirectal tissues. This barrier can be breached through the crypts of Morgagni, which can penetrate through the internal sphincter into the intersphincteric space. Once infection gains access to the intersphincteric space, it has easy access to the adjacent perirectal spaces. Extension of the infection can involve the intersphincteric space, ischiorectal space, or even the supralevator space. In some instances, the abscess remains contained within the intersphincteric space. The variety of anatomic sequelae of the primary infection is translated into variable clinical presentations. Frequency The peak incidence of anorectal abscesses is in the third and fourth decades of life. Men are affected more frequently than are women, with a male-to-female predominance of 2:1 to 3:1. Approximately 30% of patients with anorectal abscesses report a previous history of similar abscesses that either resolved spontaneously or required surgical intervention. A higher incidence of abscess formation appears to correspond with the spring and summer seasons. While demographics point to a clear disparity in the occurrence of anal abscesses with respect to age and sex, no obvious pattern exists among various countries or regions of the world. Although suggested, a direct relationship between the formation of anorectal abscesses and bowel habits, frequent diarrhea, and poor personal hygiene remains unproved. The occurrence of perianal abscesses in infants also is quite common. The exact mechanism is poorly understood but does not appear to be related to constipation. Fortunately, this condition is quite benign in infants, rarely requiring any operative intervention in these patients other than simple drainage. Etiology Perirectal abscesses and fistulas represent anorectal disorders arising predominately from the obstruction of anal crypts. Infection of the now static glandular secretions results in suppuration and abscess formation within the anal gland. Typically, the abscess forms initially in the intersphincteric space and then spreads along adjacent potential spaces. Pathophysiology As mentioned above, perirectal abscesses and fistulas represent anorectal disorders that arise predominately from the obstruction of anal crypts. Normal anatomy demonstrates anywhere from 4-10 anal glands drained by respective crypts at the level of the dentate line. Anal glands normally function to lubricate the anal canal. Obstruction of anal crypts results in stasis of glandular secretions and, when subsequently infected, suppuration and abscess formation within the anal gland results. The abscess typically forms in the intersphincteric space and can spread along various potential spaces. Common organisms implicated in abscess formation include Escherichia coli, Enterococcus species, and Bacteroides species; however, no specific bacterium has been identified as a unique cause of abscesses. Less common causes of anorectal abscess that must be considered in the differential diagnosis include tuberculosis, squamous cell carcinoma, adenocarcinoma, actinomycosis, lymphogranuloma venereum, Crohn's disease, trauma, leukemia, and lymphoma. These may result in the development of atypical fistula-in-ano or complicated fistulas that fail to respond to conventional surgical treatment. Presentation The classic locations of anorectal abscesses listed in order of decreasing frequency are as follows: perianal 60%, ischiorectal 20%, intersphincteric 5%, supralevator 4%, and submucosal 1%. These major types are illustrated in the image below. Clinical presentation correlates with the anatomic location of the abscess. Illustration of the major types of anorectal abscesses (submucos al not pictured). Patients with a perianal abscess typically complain of dull perianal discomfort and pruritus. Their perianal pain often is exacerbated by movement and increased perineal pressure from sitting or defecation. Physical examination demonstrates a small, erythematous, well-defined, fluctuant, subcutaneous mass near the anal orifice. Patients with an ischiorectal abscess often present with systemic fevers, chills, and severe perirectal pain and fullness consistent with the more advanced nature of this process. External signs are minimal and may include erythema, induration, or fluctuancy. On digital rectal examination (DRE), a fluctuant, indurated mass may be encountered. Optimal physical assessment of an ischiorectal abscess may require anesthesia to alleviate patient discomfort that would otherwise limit the extent of the examination. Patients with an intersphincteric abscess present with rectal pain and exhibit localized tenderness on DRE. Physical examination may fail to identify an intersphincteric abscess. Although rare, supralevator abscesses present a similar diagnostic challenge. As a result, clinical suspicion of an intersphincteric or supralevator abscess may require confirmation through computed tomography (CT) scanning, magnetic resonance imaging (MRI), or anal ultrasonography. Use of the last modality is limited to confirming the presence of an intersphincteric abscess. Indications As a rule, the presence of an abscess is an indication for incision and drainage. Watchful waiting while administering antibiotics is inadequate. Relevant Anatomy Classification of anorectal abscess Abscesses are classified based on their anatomic location. The most commonly described locations are perianal, ischiorectal, intersphincteric, and supralevator. The image below illustrates the different anatomic locations of anorectal abscesses. Perianal abscesses represent the most common type of anorectal abscesses, accounting for approximately 60% of reported cases. These superficial collections of purulent material are located beneath the skin of the anal canal and do not transverse the external sphincter. The next most common types of abscesses, in descending order of frequency, are ischiorectal, intersphincteric, and supralevator. An ischiorectal abscess forms when suppuration transverses the external sphincter into the ischiorectal space. Intersphincteric abscesses result from suppuration contained between the internal and external anal sphincters. A supralevator abscess results either from primary disease in the pelvis (eg, appendicitis, diverticular disease, gynecologic sepsis) or from suppuration extending cranially from an origin in the intersphincteric space, through the longitudinal muscle of the rectum and reaching above the levators. Horseshoe abscesses, while rare, result from circumferential infiltration of pus within the intersphincteric planes. The Goodsall rule for perianal fistulas The Goodsall rule states that the external opening of a fistulous tract located anterior to a transverse line drawn across the anal verge is associated with a straight radial tract of the fistula into the anal canal/rectum. Conversely, an external opening posterior to the transverse line follows a curved, fistulous tract to the posterior midline of the rectal lumen. This rule is important for planning surgical treatment of the fistula and is illustrated in the images below. Diagram illustrating the Goodsall rule for anorectal fistulas. Fistulas that exit in the posterior half of the rectum generally follow a curved course toward the posterior midline, while those that exit in the anterior half of the rectum usually follow a radial course to the dentate line. Illustration of the Goodsall rule for anorectal fistulas. Note the curved nature of the posterior fistulas and the radial (straight) orientation of the anterior fistulas. Contraindications Clinical suspicion of anorectal abscess warrants aggressive identification and surgical drainage. Delayed surgical intervention results in chronic tissue destruction, fibrosis, and stricture formation and may impair anal continence. Delayed incision and drainage of an anorectal abscess is contraindicated. Workup Laboratory Studies 1. No specific laboratory studies are indicated in the evaluation of a patient with a perianal or anorectal abscess. 2. Certain patients, such as individuals with diabetes and patients who are immunocompromised, are at high risk for developing bacteremia and possibly sepsis, as a result of an anorectal abscess. In such cases, complete laboratory evaluation is important. Laboratory evaluation of the septic patient is not the focus of this article. Imaging Studies Imaging studies rarely are necessary in the evaluation of patients with an anorectal abscess; however, clinical suspicion of an intersphincteric or supralevator abscess may require confirmation by CT scanning, MRI, or anal ultrasonography. Use of the last modality is limited to confirming the presence of an intersphincteric abscess. The ultrasound can also be used intraoperatively to help identify a difficult abscess/fistula. Diagnostic Procedures 1. Digital examination under anesthesia can be helpful in certain cases, because patient discomfort can significantly limit physical assessment. For example, optimal evaluation for an ischiorectal abscess is performed in this manner. A fistula tract can be injected with peroxide solution at the time of examination under anesthesia in order to facilitate the visualization of the internal opening of the fistula. 2. Evidence suggests that the use of endoscopic visualization (transrectal and transanal) is an excellent way to evaluate complex cases of perianal abscess and fistula. With the endoscopic technique, the extent and configuration of the abscess and fistulas can be clearly visualized. The endoscopic visualization has been reported to be as effective as fistulography. In experienced hands, endoscopic evaluation is the preferred diagnostic procedure in patients with perirectal pathology because of the low risk of bacterial dissemination and the low incidence of patient discomfort. Utilizing endoscopic evaluation after nonsurgical treatment is also effective for the documentation of the patient's response to therapy. Treatment Medical Therapy In most patients with anorectal abscess, adjuvant medical therapy with antibiotics generally is not necessary. However, the presence of a systemic inflammatory response, diabetes, or immunosuppression justifies the concomitant use of antibiotics. Surgical Therapy Treatment of anorectal abscesses involves early surgical drainage of the purulent collection.4,5,6,7,8 Primary antibiotic therapy alone is ineffective in resolving the underlying infection and simply postpones surgical intervention. Any delay in surgical drainage of anorectal abscesses prolongs infection, augments tissue damage, and may impair sphincter continence function, as well as promote stricture and/or fistula formation. The ability to drain an anorectal abscess depends on patient comfort and on the location and accessibility of the abscess. Drainage of perianal or superficial abscesses usually can be accomplished in the office or emergency department, using local anesthetics. A small incision is made over the area of fluctuancy in close proximity to the anal verge. Pus is collected and sent for culture. Hemostasis is achieved with manual pressure, and the wound is packed with iodophor gauze. The gauze is removed after 24 hours, and the patient is instructed to take sitz baths 3 times a day and after bowel movements. Postoperative analgesics and stool softeners are prescribed to relieve pain and prevent constipation. The patient typically will follow up with his/her physician in 2-3 weeks for wound evaluation and inspection for possible fistula-in-ano. (A short fistula-in-ano coursing through a minimal amount of external sphincter is best treated with a fistulotomy.) A potential complication of anorectal abscess drainage is the formation of fistulous tracts. Management of fistulas will be addressed later in this review. The type of organism cultured from an anorectal abscess is an important predictor of fistula formation following surgical incision and drainage. Underlying anal fistulas are present in 40% of abscess cultures that are positive for intestinal bacteria; however, cultures growing Staphylococcus species are associated with perianal skin infections and typically indicate that there is no subsequent risk that anal fistulas will develop. Treatment of ischiorectal, intersphincteric, and supralevator abscesses is performed best under general or regional anesthesia. In the case of ischiorectal abscess, a cruciate incision is made at the site of maximal swelling. Pus is drained and cultured. The ischiorectal fossa is probed with a finger or hemostat to disrupt loculations and facilitate drainage. Placement of a drain only is indicated for the management of complex or bilateral abscesses. To drain an ischiosphincteric abscess, a transverse incision is made in the anal canal below the dentate line posteriorly. The intersphincteric space is identified, and the plane between the internal and external sphincters is exposed. The abscess is opened to allow drainage, and a small mushroom catheter is sutured in situ to assist drainage and prevent premature wound closure. Location and etiology determine the drainage technique to be used for supralevator abscesses. Failure to manage supralevator abscesses with consideration of the primary etiology may result in iatrogenic fistula formation. Evaluation with MRI or CT scanning can exclude intra-abdominal or pelvic pathology as possible sources. If the supralevator abscess evolved from the extension of an ischiorectal abscess, external drainage through the ischiorectal fossa would be indicated. If the abscess resulted from an upward extension of an intersphincteric abscess, appropriate drainage would be created through the rectal mucosa. In cases of posterior supralevator abscess collections, a transverse incision is made in the posterior anal canal below the dentate line. The dissection extends from the intersphincteric plane through the puborectalis sling and into the posterior anal space. A mushroom catheter then is sutured in place to ensure adequate drainage. Anterior supralevator abscesses are superficial and are more common in women than in men. Surgical drainage may be approached using an anteriorly directed transanal incision or by a transvaginal approach entering the posterior cul-de-sac. A mushroom catheter is placed to ensure adequate drainage of the abscess collection. Patients with systemic signs of toxicity are admitted to the hospital and treated with intravenous antibiotics. If the patient does not improve clinically over the next 24-48 hours, reevaluation of the supralevator abscess by CT scan or reoperation may be indicated. In the face of recurrent, severe supralevator abscesses, some patients may require a diverting colostomy for optimal management. The anal fistula is a common surgical ailment that has been reported since the time of Hippocrates, but little systematic evidence exists on its management. Different treatment modalities have been evaluated in 443 reported trials. Examples of various research studies include the following: 1. Treatment with fistulotomy versus the use of fistulectomy 2. Seton treatment 3. Marsupialization 4. Glue therapy 5. Anal flaps 6. Radiosurgical approaches 7. Fistulotomy/fistulectomy at time of abscess incision 8. Intraoperative anal retractors Two reported meta-analyses evaluated the use of incision and drainage alone vs the employment of incision + fistulotomy. Evidence suggests that following fistulotomy, marsupialization reduces bleeding and permits faster healing. Results from small trials indicate that healing rates after flap repair may be no worse than those following fistulotomy, although this has not yet been proven.11 Failure rates may increase in cases in which flap repair has been combined with fibrin glue treatment of fistulas.12 Radiofrequency fistulotomy results in less pain on the patient's first postoperative day and may permit faster healing.13 However, a great deal is not yet understood about the surgical treatment of anal fistulas. 7 Preoperative Details Because of the acute nature of anorectal abscesses, preoperative bowel preparation is not possible and typically is unnecessary. Intraoperative Details Decisive management of anal fistulas relies on therapeutic interventions. Healing rarely is spontaneous, and failure to achieve adequate treatment often results in recurrent abscess, persistent drainage, and even malignancy. The main paradigms to follow in the management of anorectal fistulas include the following: 1. Determine the anatomy of the fistula 2. Provide adequate drainage 3. Eradicate the fistula tract 4. Prevent recurrence 5. Preserve sphincter function - Preservation of sphincter function relies on maintaining the integrity of the anorectal ring. Once the external opening of the anorectal fistula has been identified and the surrounding tissue has been palpated, probing of the fistula tract is warranted. Aggressive probing of the fistula is discouraged to prevent formation of false channels. Using a blunt probe (eg, a small lachrymal probe), the internal origin of a primary fistula can be identified in the majority of cases. When searching for a fistula tract's opening in the anal canal, the Goodsall rule is an excellent guideline. This rule states that an external opening anterior to a transverse line drawn across the anal verge is associated with a straight radial tract into the canal. An external opening posterior to the transverse line follows a curved fistulous tract to the posterior midline rectal lumen. Horseshoe fistulas occasionally are associated with anterior and posterior openings in the anal canal. Treatment options for the management of fistulas are aimed at providing definitive therapy while minimizing the morbidity of the procedure. For example, 2 widely accepted treatment interventions include fistulectomy and fistulotomy. Studies have demonstrated that removal of the entire fistula tract along with the surrounding scar tissue (ie, fistulectomy) unnecessarily results in a larger wound, prolonged healing time, and higher risks of incontinence. As a result, the more conservative approach of unroofing the tract without excising all surrounding tissue (fistulotomy) usually is preferred and decreases the risk of incontinence and fistula recurrence; fistulotomy also shortens wound healing time. A fistulotomy is performed as a primary procedure for superficial fistulas that require minimal dissection of the fistula from the surrounding sphincter musculature. In contrast, simple fistulotomy for repair of high-level fistulas is contraindicated as the primary treatment. The use of loose setons is warranted in high-level fistulas (ie, transsphincteric and suprasphincteric) to reduce the risk of incontinence or in cases in which poor wound healing is anticipated. Setons may also be used as temporary initial intervention in the management of a fistula. A seton is a nonabsorbable nylon or silk suture that is guided through the fistula tract and tied exteriorly, in this way compressing and maintaining suture placement in the tract. Other material frequently used for seton placement include soft vessel loop. The seton suture must be left in place for a prolonged period of time (weeks to months). The ischemic compression by the seton and the local inflammatory reaction of adjacent tissues initiates fibrosis. Once fibrosis of the surrounding tissue develops, it helps to maintain the integrity of the sphincter musculature during subsequent fistulotomy. Setons often are used in patients with fistulas secondary to inflammatory bowel disease (IBD). In addition, the seton allows epithelialization of the fistulous tract, thereby preventing secondary closure and facilitating the drainage of abscesses. Another commonly used type of seton is the cutting seton, which can be used to gradually transect the anal sphincter musculature underlying the fistula by externally tightening the suture to induce pressure necrosis. Typically, retightening the seton over a period of several days is necessary (this can be performed in the outpatient setting). The cutting seton may eliminate the need for subsequent fistulotomy. While the cutting seton is used as an effective therapeutic option for high-level fistulas, it is contraindicated in patients with IBD. Other treatment modalities include resection with coverage using advancement tissue flaps (used for more complex cases) and bioprosthetic fistula plug (made of surgisis porcine submucosa). The plug technique is indicated in selected cases with long fistulous tracts. The success rate is variable (5070%). Patients with anal fissures can be treated with nifedipine gel (calcium channel blocker - topical use) and Botox injections. Occasionally, sphincterotomy (lateral internal anal sphincter muscle) may be necessary. Postoperative Details Postoperatively, administer analgesics for pain, stool bulking agents, and stool softeners to prevent constipation. Followup evaluation of an incised anorectal abscess is important not only for determining whether healing is adequate, but also for assessing the potential development of anorectal fistulas. The patient typically will follow up with his/her physician in 2-3 weeks for wound evaluation and inspection for possible fistula-in-ano. Antibiotics are used as adjuncts to surgical therapy for patients with a comorbidity, such as diabetes, valvular heart disease, or immunodeficiency. Follow-up The patient typically will follow up with his/her physician in 2-3 weeks for wound evaluation and inspection for possible fistula-in-ano. Complications Anorectal fistulas Anorectal fistulas occur in 30-60% of patients with anorectal abscesses. The intersphincteric glands lie between the internal and external anal sphincters and are associated most commonly with abscess formation. Anorectal fistulas arise through obstruction of anal crypts and/or glands and are identified by purulent drainage from the anal canal or from the surrounding perianal skin. Other etiologies of anorectal fistulas are multifactorial and include diverticular disease, IBD,14 malignancy, and complicated infections, such as tuberculosis and/or actinomycosis. The Parks classification system defining the 4 major types of anorectal fistulas in order of decreasing frequency is as follows15 : intersphincteric (70%), transsphincteric (23%), extrasphincteric (5%), and suprasphincteric (2%). An intersphincteric fistula is found between internal and external sphincters. A transsphincteric fistula extends through the external sphincter into the ischiorectal fossa. An extrasphincteric fistula passes from the rectum to the skin through the levator ani. Lastly, the suprasphincteric fistula extends from the intersphincteric plane through the puborectalis muscle, exiting the skin after traversing the levator ani. The Goodsall rule states that an external opening of a fistulous tract that is anterior to a transverse line drawn across the anal verge is associated with a straight radial tract of the fistula into the anal canal/rectum. Conversely, an external opening that is posterior to the transverse line demonstrates a curved fistulous tract to the posterior midline rectal lumen. This rule, which is important for the planning of surgical treatment of the fistula, is illustrated below. Approximately two thirds of patients with rectal abscesses who are treated by incision and drainage or by spontaneous drainage will develop a chronic anal fistula. The recurrence rate of anorectal fistulas after fistulotomy, fistulectomy, or the use of a seton is about 1.5%. The success rate of primary surgical treatment with fistulotomy appears to be fairly good.16 The overall incidence of major fecal incontinence after the surgical management of complex suprasphincteric fistulas is estimated to be approximately 7%. Future and Controversies Some surgeons advise performing a complementary colostomy to facilitate the management of complex anal fistulas. This may be of some benefit in selected cases, but the perirectal infection may continue despite a diverting colostomy. Adequate drainage of the abscess is the most important factor in controlling progressive perirectal infection.