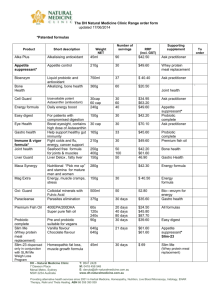
HLC Multi Strain is a 15 billion CFU probiotic
advertisement

HLC Multi Strain is a 15 billion CFU probiotic formula, providing four strains of proprietary human-sourced Lactobacillus acidophilus (CUL-60 & CUL-21), Bifidobacterium bifidum and Bifidobacterium animalis subsp. lactis that temporarily modify gut flora,* and have been tested in various human clinical trials. The capsules are 100% pure vegetable-sourced which makes the product ideal for vegans. Additional product info: The microbiota ensures intestinal structure and function and the homeostasis of the gut microbiota also maintains various functions, which are vital to the maintenance of human health. In fact, disruption of the intestinal ecosystem equilibrium (gut dysbiosis) is associated with a plethora of human diseases, including autoimmune and allergic diseases, and bacterial infections.(1) Colonic infection with Clostridium difficile, leading to pseudomembranous colitis, is a common complication of antibiotic therapy, especially in elderly patients. It has been suggested that nonpathogenic probiotic bacteria might prevent the development and recurrence of C. difficile infection. A double-blind, placebo-controlled study examined the role of probiotic administration in the prevention of C. difficile-associated diarrhoea (CDAD) in elderly patients receiving antibiotic therapy. Consecutive patients (150) receiving antibiotic therapy were randomised to receive either a probiotic containing both Lactobacillus and Bifidobacterium or placebo for 20 days. Each patient received one capsule/day for 20 days. The probiotic product (provided by Cultech, Swansea) comprised 2 x 1010 CFU Lactobacillus acidophilus and Bifidobacterium bifidum/capsule; the placebo comprised the inactive carrier. Upon admission to hospital, bowel habit was recorded and a faecal sample taken. Trial probiotic or placebo was taken within 72 h of prescription of antibiotics, and a second stool sample was taken in the event of development of diarrhoea during hospitalisation or after discharge. Of the randomised patients, 138 completed the study, 69 with probiotics in conjunction with antibiotics and 69 with antibiotics alone. On the basis of development of diarrhoea, the incidence of samples positive for C. difficile-associated toxins was 2.9% in the probiotic group compared with 7.25% in the placebo-control group. Toxin testing of the C. difficile-positive patients indicated that five of the 11 probiotic patients (46%) were toxin-positive with two of the five toxin-positive patients showing signs of diarrhoea. Seven of the nine placebo patients carrying C. difficile (78%) were toxin-positive, and six of these seven had diarrhoeal symptoms.(2) The effects of probiotic supplementation on the intestinal re-growth microbiota following antibiotic therapy were studied in another double-blind placebo-controlled study. The probiotic product (Cultech Ltd., Port Talbot, UK) comprised two strains of Lactobacillus acidophilus (CUL60 and CUL21) and two strains of Bifidobacterium spp. at a total of 2.5 X 1010 colony-forming units (CFU)/capsule, and the placebo comprised an inactive carrier (maltodextrin). Patients received one capsule daily. In the placebo group, numbers of facultative anaerobes and enterobacteria increased significantly, and at day 35 the numbers were significantly higher in the placebo group than in the active group; in the active group, the numbers of bacteroides increased significantly. Although the numbers of enterococci in both groups did not change, in the placebo group the number of patients harbouring antibioticresistant enterococci post therapy increased significantly. From this study, it would appear that daily supplementation with viable probiotic bacteria during and post antibiotic therapy reduces the extent of disruption to the intestinal microbiota as well as the incidence and total numbers of antibiotic-resistant strains in the re-growth population.(3) In a pilot-scale, double-blind, placebo-controlled trial, 30 patients with Helicobacter pylori infection were randomised into three groups prior to their 7 days eradication therapy, to study the effects of probiotic supplement comprising Lactobacillus acidophilusand Bifidobacterium bifidum on the intestinal microflora in response to antibiotic therapy. Group I received the placebo product from day 1 to day 15, Group II received placebo from day 1 to day 7 and probiotics from day 8 to day 15 and Group III received probiotics from day 1 to day 15. Patients took one probiotic or placebo capsule daily with food, according to their group. A commercially available probiotic product was provided by Cultech Ltd (Swansea, UK) and comprised two strains of Lactobacillus acidophilus (CLT60 and CUL21) and two strains of Bifidobacterium bifidum (CUL17 and B. bifidum Rhodia, New Jersey, USA) at a total of 2.5 x 1010 colony forming units (CFU)/capsule. The placebo comprised an inert carrier (maltodextrin, Cultech Ltd). Patients provided stool samples for analysis on days 1, 7, 12, 17 and 27. For patients in Groups I and II, significant increases in the facultative anaerobe component of the microflora occurred between days 1 and 7. In Group I, the numbers remained elevated to day 27 but in Group II, the numbers decreased significantly between days 7 and 27 back to the starting levels. In Group III, the facultative anaerobe population remained stable throughout. The total anaerobe numbers increased significantly at day 27 than at day 1 for Group I, were unchanged throughout for Group II and decreased significantly for the patients in Group III between days 1 and 7 before reverting to the starting levels by day 27. From these results, it can be seen that probiotic supplementation modulates the response of the intestinal microflora to the effects of antibiotic therapy. (4) The efficacy of probiotics in alleviating the symptoms of irritable bowel syndrome (IBS) appears to be both strain- and dose-related. The aim of a study was to investigate the effect of a multistrain probiotic preparation on symptoms of IBS. This probiotic preparation has not previously been assessed in IBS. Fifty-two participants with IBS, as defined by the Rome II criteria, participated in this double blind, randomized, placebo-controlled study. Participants were randomized to receive either a probiotic preparation comprising two strains of Lactobacillus acidophilus CUL60 and CUL21, Bifidobacterium lactis CUL34 and Bifidobacterium bifidumCUL20 at a total of 2.5 × 1010 cfu/capsule or a placebo for 8 weeks. Subjects were asked to complete a validated questionnaire to assess IBS symptoms at baseline and fortnightly throughout the 8 weeks study period. The questionnaire assessed severity and duration of abdominal pain (abdominal pain, days with pain), abdominal distension (bloating), satisfaction with bowel habits and quality of life. The following results were noted: 1. The number of days with pain improved significantly by week 2 in the probiotic group, but did not reduce significantly for the placebo group until 4 weeks into the study. 2. The severity of abdominal pain reduced significantly in both groups from week 4 onwards. 3. Significant improvements in quality of life were recorded for those receiving the probiotic at the end of the intervention period and this was associated with significantly improved satisfaction with bowel habit for the probiotic subjects over the placebo group at 6 weeks. Significant improvements from baseline for symptoms severity score were seen throughout the intervention period in both active and placebo groups from weeks 2. Comparison of the effectiveness of the probiotic in the presence of significant placebo effect in this study showed a significant difference in the Symptom Severity Score in favour of the probiotic at 6 weeks and 8 weeks but by 2 weeks after the 8 weeks of the intervention, no significant difference could be detected between the probiotic and placebo group. LAB4 multistrain probiotic supplement may benefit subjects with IBS.(4) References: 1. Prakash S, Rodes L, Coussa-Charley M, Tomaro-Duchesneau C. Gut microbiota: next frontier in understanding human health and development of biotherapeutics. Biologics. 2011;5:71-86. 2. Plummer, S., Weaver, M.A., Harris, J.C., Dee, P. and Hunter, J. “ Clostridium difficile pilot study: effects of probiotics supplementation on the incidence of C.difficile diarrhea.” International Microbiology. 2004; 7(1):59-62. 3. Plummer SF, Garaiova I, Sarvotharn T, Cottrell SL, LeScouiller S, Weaver MA et al. Effects of probiotics on the composition of the intestitinal microbiota following antibiotic therapy. Int J Antimicrob Agents. 2005; 26(1):69-74. 4. Madden JA, Plummer SF, Tang J, Garaiova I, Plummer NT, Herbison T, et al. Effects of probiotics on preventing disruption of the intestinal microflora following antibiotic therapy: a double-blind, placebo-controlled pilot study. Int Immunopharmacol. 2005; (6): 1091-7. 5. Williams EA, Stimpson J, Wang D, Plummer S, Garaiova I, Barker ME, Corfe BM. “Clinical trial: a multistrain probiotic preparation significantly reduces the symptoms of irritable bowel syndrome in a double-blind placebo-controlled trial.” Alimentary Pharmacology & Therapeutics. 2009. 29(1):97-103. 6. NHPD Abbreviated Labelling Standard – Live Microorganisms. August 30, 2011