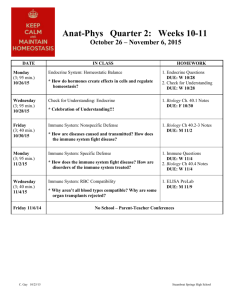
19_20_Microbe Immunity - V14-Study
advertisement

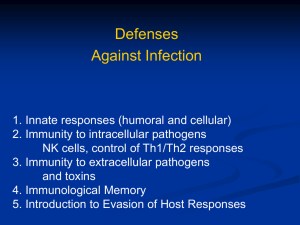
Immunity to Microbes Immunity to Viruses - Viruses are intracellular microorganisms that replicated within host cells - Innate and adaptive immune responses to viruses are aimed at blocking infection and eliminating infected cells - Innate immunity to viruses (0-96 hours of infection) Inhibition of infection by type I interferons (IFNs) o IFNα and IFNβ are produced by virus-infected as well as cells that protect neighboring cells that are not yet infected (i.e. fibroblasts, macrophages, dendritic cells) o Type I IFNs (via paracrine action) cause neighboring cells to synthesize enzymes that interfere with viral transcription and replication, preventing the virus from entering the host cell Killing of infected cells by NK cells o Inhibitory NK cell receptors interact with MHC class I molecules on normal host cells, which sends a signal to the NK cell that prevents it from killing normal host cells o Some viruses “turn off” MHC class I expression, leading to activation of NK cell killing NK cells kill infected host cells via perforin-granzyme mechanism - Adaptive immunity to viruses (from day 4 of infection until infectious agent is eliminated) Blockage of virus entry into host cells by antibodies o Antibodies have an important role in containing the spread of a virus in the acute phase of infection, but cannot typically eliminated the virus once infection has occurred o Anti-viral antibodies are mostly effective against viruses during their extracellular stage o Antibodies function as neutralizing antibodies Bind to virus surface proteins, preventing their attachment and entry into host cells o IgM is detectable at day 5 and peaks at 2 weeks IgM responses are not strong Half-life is short (~ 5 days) – disappears by 4-6 weeks o IgG is detectable at day 5-10 and peaks at 2-3 weeks IgG responses are strong Longer half-life (~25 days) – disappears in months to over a year o Secretory IgA is important for viral neutralization at mucosal surfaces Secretory IgA is detectable at day 5-10 and peaks at 2-3 weeks Half-life is 5-6 days – disappears in 6-8 weeks o Complement activation may participate in antibody-mediated viral immunity by promoting phagocytosis and direct viral lysis, though is not thought to be a major contributor as individuals with complement deficiencies are not predisposed to viral infections Destruction of virus-infected cells via ADCC (mediated by NK cells) o IgG-coated virus-infected cells are bound by NK cells via Fc receptors and rapidly destroyed via perforin-dependent killing Killing of infected cells (elimination of infection) by CTLs o CTLs are most important in host defense once a viral infection is established Arise at day 4 and peak at 1-2 weeks Utilized a perforin-granzyme mechanism of killing virus-infected cells o Within 7-10 days of primary infection, most virus particles are eliminated o Importance of CTLs in defense against viral infection is demonstrated by increased susceptibility to viral infections in animals deficient in CD8+ T cells Evasion of Immune Mechanisms by Viruses - Antigenic variation Viruses alter their antigens via many methods to escape neutralization by host’s pre-existing immunity o Antigenic drift Allows influenza virus to persist in a population because the new virus strain is resistant to immunity generated in the population by previous infection o Antigenic shift – reassortment of RNA genomes in RNA viruses Occurs via genetic reassortment between influenza viruses from two different species Vaccination against viruses that exhibit rapid antigenic variation is complicated by antigenic diversity o Equine infectious anemia (EIV) is a viral disease that has rapid antigenic variation Downregulation of MHC class I molecules Cytomegalovirus blocks the assembly and expression of stable MHC class I molecules and display of viral peptides, thus preventing CTLs (but not NK cells) from killing infected cells Viruses produce immunosuppressive molecules Poxviruses encode molecules that bind and block activity of cytokines o IFNγ, TNF, IL-1, and chemokines Viruses may infect and kill immunocompetent cells Simian immunodeficiency virus (SIV) and feline immunodeficiency virus (FIV) kill CD4+ cells Equine Herpes virus-1 (EHV-1) EHV-1 evades immune response and hides (goes latent) in trigeminal ganglion - Immunity to Intracellular Bacteria - Some bacteria (i.e. Brucella abortus, mycobacterium tuberculosis, etc.) can readily grow inside macrophages - Innate immunity can limit bacterial growth but usually fails to eradicate intracellular bacterial infections - Innate immunity to intracellular bacteria Principal effectors against intracellular bacteria are phagocytes and NK cells o Phagocytes (macrophages) can kill bacteria if sufficiently activated Macrophages secrete IL-12, a powerful activator of NK cells NK cells produce IFNγ, a potent activator of macrophages IFNγ promotes killing of phagocytosed bacteria - Adaptive immunity to intracellular bacteria Major protective adaptive immune response against intracellular bacteria is cellular immune response Killing of phagocytosed bacterial by macrophages o IFNγ released from Th1 cells results in macrophages activation o IFNγ also stimulates the production of antibody isotypes that activate complement and opsonize bacteria for phagocytosis, thus aiding in the effector functions of macrophages Lysis of infected host cells by CTLs o Bacteria that escape from phagosome into cytoplasma are not longer susceptible to phagocytosis, but are eliminated by CTLs o CTLs destroy infected host cells and bacteria released from killed cells are then phagocytosed and eliminated by activated macrophages Evasion of Immune Mechanisms by Intracellular Bacteria - Blocking phagosome-lysosome fusion Mycobacterium tuberculosis and brucella abortus secrete molecules that inhibit fusion of lysosome with phagosome - Disruption of phagosome membrane and escape into cytoplasm Listeria monocytogenes releases toxin listeriolysin that lyses phagosome membrane, resulting in escape of Listeria into cytosol, effectively evading killing - Resistant cell wall The lipid cell wall of Corynebacterium pseudotuberculosis makes it resistant to lysosomal enzymes How does an adaptive immune response develop when pathogens enter through skin, blood, or mucosal surfaces? SEE CHAPTER 8 Mechanisms of Immunological Killing of Extracellular Pathogens - Humoral immune response is the main protective response against extracellular pathogens - Antibodies and complement act in several ways to protect host (summarized in figure below) Toxin neutralization o Antibody to a microbial toxin can bind to the toxin and neutralize it o Antibody-toxin complexes are cleared by phagocytes like any other antigen-antibody complex Opsonization and phagocytosis o Antibody (or complement component C3b) binds to accessible antigens on microbial surface and acts as an opsonin that increases phagocytosis and clearance of microbe o Other complement products serve as chemotactic factors for neutrophils and macrophages, therefore contributing to the buildup of phagocytic cells at the site of infection Anaphylatoxins mediate mast cell degranulation o Complement product C3a, C4a, and C5a act as anaphylatoxins that induce local mast cell degranulation, vasodilation, and extravasation of lymphocytes and neutrophils from blood Complement-mediated lysis African Trypanosomes - Extracellular single-celled, flagellated protozoan parasites that live in the bloodstream of several host species and are transmitted by the bit of a tsetse fly In the bloodstream, trypanosomes continually divide every 4-6 hours - - Cause African Trypanosomiasis The disease affects people, causing Human African Trypanosomiasis (HAT) or Sleeping Sickness The disease affects animals, causing Animal African Trypanosomiasis (AAT) or Nagana The disease occurs in 37 sub-Saharan countries covering more than 9 million km2 (corresponds to about one-third of the Africa's total land area) Human and animal disease are major obstacles to the development of rural regions of sub-Saharan Africa due to human loss, decimation of cattle, and abandonment of fertile land in areas of rife disease Trypanosoma gambiense – agent of human “Sleeping Sickness” in western and central Africa Trypanosoma rhodesiense – agent of human Sleeping Sickness in eastern Africa Trypanosoma brucei Causative agent of "Nagana" in Africa Found in different animals with different clinical signs Not a human pathogen and relatively benign for wild mammals Immune Responses to Trypanosome Infection - Trypanosomes are targeted by a robust humoral immune response Immune response is generated against portions of the trypanosome surface coat – variant surface glycoprotein (VSG) molecules o Anti-VSG antibodies promote complement-mediated lysis of the trypanososmes o Anti-VSG antibodies also promote parasite opsonization and phagocytosis o In this manner, the trypanosome population crashes and few parasites can be detected in the blood of infected individuals - Trypanosomes exhibit antigenic variation ~1% of the parasitic organisms bear an antigenically-different VSG and escape the antibody response to proliferate in the bloodstream, causing cyclic waves of parasitemia Trypanosome antigenic variation occurs via VSG switching o Individual trypanosomes carry a large repertoire of VSG genes (~10% of the trypanosome genome is devoted to VSG genes), each encoding a different VSG protein o A trypanosome only expresses a single VSG at one time o Activation of a new VSG gene displaces the previous one from the expression site - Recall that antibody production also involves gene rearrangement in host B cells. It is remarkable that both trypanosomes and their hosts use similar mechanisms of gene rearrangement to promote their survival Resistance to Trypanosomiasis While T. brucei brucei causes debilitating disease in cattle, killing millions annually, wild African ungulates (i.e. Cape buffalo) are resistant to infection o Cape buffalo only develop a single wave of parasitemia o Buffalo generate anti-VSG antibodies to suppress parasitemia, but cannot eliminate infection Results in chronic cryptic infection o These animals develop trypanosome-killing activity in their serum o The effector activity derives from the enzyme xanthine oxidase whose action generates hydrogen peroxide that is highly toxic for African trypanosomes o Efficacy of this mechanism is controlled by serum catalase (breaks down hydrogen peroxide), which becomes suppressed in infected Cape buffalo at the time of remission of the first parasitemic wave o Catalase activity is restored some weeks later at which time blood parasites reappear but are held at a level of 1 to 10 organisms/ml by an xanthine oxidase-independent process o Antibodies against non-VSG molecules contribute to this protection Antibodies are thought to bind to receptors for host macromolecules and inhibit trypanosome growth T. brucei brucei infects a wide range of mammals but is unable to infect humans o Humans are innately immune to T. brucei brucei (but not the human agent of trypanosomiasis) because these parasites are lysed by components of normal human serum Apolipoprotein L-1 can mediate trypanosome killing Immunity to Worms - Parasitic helminths (worms) comprise a diverse group of long-lived organisms that can cause chronic infections - Helminthiases are generally caused by species of Nematodes and Platyhelminths These worm parasites are typically extracellular and occupy numerous niches within their mammalian hosts (i.e. bloodstream, intestinal lumen) Unlike microbial pathogens, helminths do not multiply within hosts - Immune responses to different types of worms are very similar, defined by several characteristics Type Th2 immune response High levels of IgE Strong eosinophil and mast cell responses Production of significant quantities of IL-4, IL-5, IL-10, IL-13, IL-14 induces B cells to class switch to IgE production and, with IL-3, stimulates growth of mast cells Immune Response to Schistosomes - Extracellular parasitic blood worms that infect several wildlife species, livestock and people Infection occurs through contact with freeswimming larvae, cercariae, which are released from infected intermediate snail hosts. When cercariae contact the skin of their final, vertebrate host, they secrete digestive enzymes that help them bore through the skin into local capillaries. The parasites migrate in the blood to the lungs, liver, and finally to the primary site of infection (varies with species). Eggs produces by adult females are released into the environment. - - - Immune response to schistosome infection Adult schistosomes live feely in the bloodstream where they are accessible to immunological effectors Characteristic Th2 response is generated against these parasites o IL-4 produced early in response plays an important role in Th2 consolidation and amplification o Degranulation of mast cells causes release of mediators that increase infiltration of inflammatory cells (eosinophils and macrophages) o Inflammatory cells express Fc receptors for IgE and IgG may bind to antibody-coated parasites Once antibody is bound the parasite, eosinophils can participated in ADCC-mediated killing of helminths Pathology of schistosome immunity The immune response against long-lived schistosome that develops with time often causes pathologic changes that can be the primary cause of disease Immune response to parasite eggs lodged in internal tissues leads to the formation of granulomas o The Th2-generated granuloma segregates pathogen from hepatic tissue and though permitting continued liver function can, in the long term, promote fibrosis and accompanying pathology Studies implicate Th2 cytokines (particularly IL-13) in development of fibrosis o Fibrosis can lead to increased portal blood pressure and development of portal varices Though granuloma formation is responsible for pathology, it can also permit survival of individual o Proven through study of animals that cannot make granulomas, which die due to toxic effects of infection o Absence of IL-4 during infection results in lethal inflammatory condition How schistosomes avoid immune elimination Sequestration of immunogenic surface antigens in an immunologically-inert, carbohydrate covering Outer surface membranes are rapidly renewed, resulting in constant shedding of immune effectors that assemble on parasite surface Production of factors that modify destructive immune response o Proteases that cleave host effectors associated with the surface of the parasite o Surface receptors that bind to and inactivate components of host’s complement cascade Parasites then inhibit the formation of MACs that destroy their outer membranes Gastrointestinal Nematode Expulsion - Susceptibility of hosts to gastrointestinal nematode infection correlates to development of Th1 response - Ability of hosts to physically expel gastrointestinal nematodes is linked to the development of a Th2 response In the gut environment, Th2 cytokines act on mast cells, epithelial cells and goblet cells to create an inhospitable environment for gastrointestinal helminths, which induces their expulsion Mucus secretion by goblet cells plays a protective role by trapping incoming worms and preventing them from establishing infection Mediators (i.e. mast cell proteases) disrupt cell junctions, increasing mucosal permeability, which can increase the fluid content of the gut lumen and allow access of protective host molecules to the worms Anti-worm antibodies may inhibit parasite mobility or orientation by cross-linking larvae into aggregates Th2-mediated local smooth muscle contractility is increased, allowing for increased expulsion These effectors have been collectively termed a “weep and sweep” response; parasites appear to be “flushed out” by increased fluid and mucus secretion and the increased propulsive activity of the gut Work with mice has shown that different helminths are expelled by somewhat different effector mechanisms Mucosal mast cells underpin resistance to Trichuris muris Goblet cells mediate resistance to Nippostryongylus braziliensis Both goblet and mast cell activation are dependent on signaling through Th2 cytokine, IL-4