Think Family - Leicestershire Partnership NHS Trust

Perinatal Maternal Mental Health
Guidance to Support Health Visitors and their
Teams
Key Words:
Version:
Adopted by:
Maternal Mental Health and Perinatal
Period, Screening, Treatment and
Referral. Health Visitors
V8
Date adopted:
Name of originator/author:
Filippa Howells
Mandy Amin
Name of responsible committee:
Date issued for publication:
Review date:
Maternal Mental Health Task and
Finishing Group 2013
LM/MA/JP/AD
Expiry date:
Target audience: Trust Board, Directors of FYPC; Head of
Services, Locality Managers, Team
Leaders Health Visitors V/SN, Lead
Practice Teachers, Clinical Team
Leaders Liaison Psychiatry, CAMHS,
Type of Policy
(tick appropriate
Name Nurses Safeguarding.
Clinical
Yes
Non Clinical box)
NHSLA Risk Management
Standards if applicable:
State 00Relevant CQC
Standards:
Held on the Trust’s Clinical
Policies.
Guidance to support Health Visitors and their Teams with Perinatal Maternal Mental Health Page 1
CONTRIBUTION LIST
Key individuals involved in developing the document
Name
Mandy Amin(Pathway Lead)
Filippa Howells
Katherine Hammond
Linda Mills
Julie Pepper
Asha Day
Designation
Practice Educator
Practice Educator
Lead Practice Teacher
Lead Practice Teacher
Lead Practice Teacher
Health Visitor
Acknowledgement – Previous originator Filippa Howells and individuals involved in developing the document version 5
– Predicting detecting and managing maternal mental illness in pregnancies and post natal period – guidance for HV service. And also for their current contribution
Circulated to the following individuals for comments
Name
Theresa Farndon
Dr Renuka Lazarus
Dr Lina Gatsou
Chris Buzzard
Nicy Turney
Anthea Brooks
Kam Gill
Maureen Curley
Chris Davies
Dorothy Sebuliba
Filippa Howells
Review Contribution List
MA/LM/JP/AD/FH/KH
Designation
Locality Manager
Consultant Psychiatrist for Perinatal Services
Consultant Psychiatrist for Adult Services
HV and SN Service Manager
Senior Nurse Professional Lead for HV
Locality Manager
Locality Manager
Locality Manager
Locality Manager
Senior Primary Mental Health Manager
Practice Educator
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 2
4
5
6
7
Section
1
2
3
CONTENT
Content
Definitions and Abbreviations
Equality Statement
Corporate Responsibilities and Governance
Monitoring Compliance and Effectiveness
Summary
Introduction
Service Delivery
Purpose
Roles and Responsibilities
8
Appendix 1 Pathway for Identification, Management and Treatment of Perinatal Maternal Mental Health for HV Service
Appendix 2 Edinburgh Postnatal Depression Scale (EPDS) for
Postpartum Depression
Appendix 3 Edinburgh Postnatal Depression Scale (EPDS) Form
Appendix 4 Perinatal Psychiatry Service Referral Form
Appendix 5 Think Family (Whole Family Approach for LPT outline)
Checklist for Review and Approval
Board Adoption Template
Signature Sheet for Approved Policies and Procedures
Table for Process for Monitoring Compliance and
Effectiveness
References and Associated Documents
Page No
6
8
8
8
9
9
12
12
13
15
16
29
17
19
20-21
22
25
26
27
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 3
Version Control and Summary of Changes
Version number
Version 2
Version 3
Version 4
Version 5
Version 6
Version 7
Version 8
Date
April 2012
May 2012
June 2012
Comments
(description change and amendments)
Fuller title and re-arrangements of the chapter and definition – agreement to include wider interventions.
To include signs and symptoms list indicating mild moderate and severe depression based on a number of symptoms. Acknowledgement of limitation to non-
English speaking clients and how to manage this.
Clearly define the training elements required and evidence based intervention included so that it was n ot a totally passive intervention of solely ‘listening’.
Agree to put a flowchart into VISIO and define it as a pathway.
Highlight the proactive promotion of bonding and attachment via ‘Solihull’ approach.
Define how training will be taken forward and to keep the ‘Think Family’ and FNP as an evidence base interventions.
Strengthen levels of support required and by whom on ‘Roles and Responsibilities’. The intervention section highlights the wider determinants of health.
August 2012 Amended to reflect comments received.
9.8.2013 Title review and re-arrangements of the chapters and definitions. Acknowledgement of limitation to non –
English speaking clients and how to manage this.
Clearly defined the training elements MMH champions DH 2013
Revised pathway flow chart.
Content updated
Stronger integration of the ‘Think Family’ (Whole
Family Approach)
Includes amended flow chart/pathway
Includes ‘Think Family’ Whole Family and
‘Troubled Family’ into the Pathway
Addresses language barriers by using a likert scale to express the level of feeling unwell.
Includes the symptoms list to help gauge the severity of the illness and how it affect the individual.
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 4
All LPT Policies can be provided in large print or Braille formats, if requested, and an interpreting service is available to individuals of different nationalities who require them.
Did you print this document yourself?
Please be advised that the Trust discourages the retention of hard copies of policies and can only guarantee that the policy on the Trust website is the most up-to-date version.
For further information contact:
Filippa Howells
Practice Educator: filippa.howells@leicspart.nhs.uk
Mandy Amin
Practice Educator: mandy.amin@leicspart.nhs.uk
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 5
Antenatal
Perinatal
Whooley
FNP
Definitions and Abbreviations that apply to this Policy
This is described as the period between conception and birth. The care provided during this period is varied in nature, but focuses on assessing whether the unborn baby is developing normally as well as monitoring the health of the mother http://www.drfosterhealth.co.uk/ medical dictionary
The perinatal period begins from the onset of pregnancy and extends to a year after birth.
The Whooley questions referred to in this document are named after
Dr Mary Whooley whose research in 1997 focused on the detection and treatment of depression in patients (screening of Veterans from the Vietnam War) (screening tool)
Family Nurse Partnership
– evidence based programme for teenage young parents (American Model).
E.I.S. Early Implementer Site (DH) programme.
Think Family This term refers to a variety of interventions with the focus on the effect of parental mental illness (PMI) on wider family members (in
LPT) and with child focus being paramount.
Think Family
Whole
Family
Approach
This is an LPT led piece of work offering early identification and intervention to support
‘children of parent’s with mental illness’.
(COPMI)
Think Family
– Troubled
Families
Agenda
This approach is led by the Local Authority which is government backed with payment by results. There is a criteria for receiving this level of service;
Criminal behaviour
Anti-social behaviour,
Being out of work
School attendance
EPDS also known as
EPNDS
This term refers to the Edinburgh Postnatal Depression Scale. It is an additional established evidence based tool which is to be used by skilled trained staff as part of a full assessment to support the screening identification and management of perinatal maternal mental health.
Listening
Visit
A listening visit gives individuals an opportunity to have their emotions ‘contained’ by the professionals involved. In addition it is an opportunity to increase a sense of wellbeing by exploring the issues causing the stressors.
That is non-directive counselling delivered in the home /clinic situation deemed suitable by the professional and acceptable to the service user.
This includes a contract between mother and professional.
Guidance to support Health Visitors and their Teams with Perinatal Maternal Mental Health Page 6
Agreed timings are essential.
Positive outcome for mother as the stressors are identified and managed constructively to alleviate possible compounding factors
This should be a time banded piece of work with a view to evaluate the effectiveness of continuation and further referral considered to more appropriate services.
Abbreviations
CPN Community Psychiatric Nurse
CMHT
NICE
CBT
IPT
Community Mental Health Team
National Institute for Clinical Excellence
Cognitive Behaviour Therapy
Interpersonal Psycho Therapy
OCD
PD
HV
CNN
Obsessive Compulsive Disorder
Personality Disorder
Health Visitor
Community Nursery Nurse
Perinatal Maternal Mental Health PMMH
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 7
Equality Statement
Leicestershire Partnership NHS Trust (LPT) aims to design and implement policy documents that meet the diverse needs of our service, population and workforce, ensuring that none are placed at a disadvantage over others. It takes into account the provisions of the Equality Act 2010 and advances equal opportunities for all. This document has been assessed to ensure that no one receives less favourable treatment on the protected characteristics of their age, disability, gender reassignment, marriage and civil partnership, pregnancy and maternity, race, religion or belief, sex (gender) or sexual orientation.
In carrying out its functions, LPT must have due regard to the different needs of different protected equality groups in their area. This applies to all the activities for which LPT is responsible, including policy development, review and implementation.
1.0 Corporate Responsibilities and Governance
1.1.1The Trust Board has a legal responsibility for ensuring this Trust policy is effectively carried out.
1.1.2 Trust Board should have key responsibility for partnership alignment with key stakeholders (including CCG, LETBS, LPT, Patient Public involvement and health watch) and ratifying this policy.
1.1.3 The Directors and Heads of Service are responsible for ensuring that staff are supported to access maternal mental health training and updates.
1.1.4 Managers and Team Leaders will be responsible for ensuring the staff competencies are reviewed through personal development review which demonstrates evidence into the governance process.
1.1.5 It is the individual responsibility of staff to refer to policy and ensure they have the competence to undertake various activities screening identification, management and treatment.
2.0 Monitoring Compliance and Effectiveness
2.1 Building upon existing audit.
Clinical audit cycle must be built in order that compliance and effectiveness is clearly demonstrated. Monitoring tools must be built in to all procedural documents in order that compliance and effectiveness can be demonstrated.
2.2 Ensure a baseline audit prior to the commencement of the PMMH training.
Regular audit will then be undertaken as per Trust policy.
Future clinical audits will have to be in line with national indicators including NICE and quality standards.
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 8
3.0 Summary
This Policy supports the early intervention of the prediction, detection and management/treatment of mental disorder in women during perinatal period. All staff working within Families, Young P eople and Children’s Services have a duty of care to assess prospective mothers for possible signs of mental illness at the earliest opportunity (refer to pathway in appendix 1).
4.0 Introduction
During pregnancy and the year following birth, women may be affected by one or more of a range of mental health problems, including anxiety and depression and postnatal psychotic disorders (though the more serious illnesses are rarer). These are collectively called perinatal mental illnesses.
Studies estimate that more than 1 in 10 women are affected by perinatal mental illness; however maternal mental illness also impacts on the infant and the rest of their families and pose an important public health challenge. (See appendix 5)
Maternal mental illness has important consequences for the impact on infant health and future behaviour and learning, and is one of the key factors determining life chances for children. Early identification, support and treatment can prevent the onset and escalation of maternal mental illness and limit the impact on the family to improve the wellbeing, health and achievement of the child (Hogg, 2013).
Mental Health for Children and Adolescents, Adults and Older Adults are considered separately in relevant guidance documents for LPT.
4.1 Facts, figures and trends
10% of all recently delivered women experience a mild or minor depressive illness (4.3 below)
Between 3% and 5% of delivered women meet the criteria for moderate to severe depressive illness as assessed by national and international studies.
2 per thousand delivered women are admitted to hospital with puerperal psychosis
Women with a history of obsessive compulsive disorders, social anxiety and panic disorder are at risk of relapse in the postnatal period.
There is gathering evidence that traumatic childbirth can cause posttraumatic stress disorder.
Antenatal mental illness is becoming more widely researched, highlighting that 15% of women will suffer from a psychiatric illness in the first trimester of pregnancy – mostly anxiety and depression
Baby Blues – This is experienced by an average of eight out of ten women, 3 to 4 days after the birth. The symptoms include feeling upset, mood swings, feeling mildly depressed and wanting to cry for no particular reason. These feelings tend to disappear after a few days.
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 9
Postnatal mental illness often occurs four to six weeks after birth, generally resembling the baby blues at first but is more intense and longer lasting. It can take up to 12 months to present. (RCN, 2013)
4.2 Risk factors associated with increased risk of perinatal mental illnesses
History of mental illness
Family history of mental illness
Antenatal psychological disturbance – e.g. anxiety or depression
Lone parent or poor couple relationships
Low levels of social support
Stressful life events
Low social status
Teenage parenthood
Early emotional trauma/childhood abuse
Unwanted pregnancy
(Hogg, 2013)
4.3 Indicators Regarding Severity
For most families the birth of a child is a joyous occasion; bringing new hope for the future. But, for some, events take a difficult turn a few weeks after birth (or sometimes before birth), when mothers start to feel one or more of the following symptoms:
Low mood/miserable most of the time
Constantly exhausted
Feeling unable to cope
Feeling guilty about not being able to cope about
not loving the baby enough
Overwhelming anxiety about the baby
Tearful for no reason
Difficulty in sleeping
No appetite or the urge to eat
Difficulties in bonding with the baby
Difficulties in their relationship with their partner
Low energy levels
Low sex drive
Withdrawal from family or friends
These are the most common symptoms for postnatal depression and can lead to a period of considerable uncertainty, anxiety and disruption. These are not just baby blues. ‘Baby blues’ is experienced by an average of eight out of ten women three or four days after birth and the symptoms include feeling upset, mood swings, being mildly depressed and wanting to cry for no particular reason. These feelings tend to disappear within a few days (ten days) after birth. Conversely, postnatal depression is an illness which occurs between four and six weeks after birth, resembles the symptoms of ‘baby blues’ at first, but is more intense and longer lasting.
If a new mother is experiencing around three of the above symptoms, she is considered to have mild postnatal depression. Having five or six of the symptoms is
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 10
considered moderate postnatal depression, and experiencing more than five or six is considered severe postnatal depression.(ref: www.givemestrength.org.uk)
4.4 The impact of perinatal mental illness
Mental illness is one of the leading causes of maternal deaths in the UK. The number of new mothers committing suicide during pregnancy, or in the 6 months after, has not fallen over the past decade. Psychiatric disorder is also associated with maternal deaths from other causes. (Oates, 2011)
Relapse or recurrence of previous post-partum mental illness is well established and believed to be a risk of between 33% and 55%.
Research shows that perinatal mental illness, most commonly depression, increases the likelihood that:
The baby will be premature or have a low birth weight
The baby may not develop a secure attachment relationship with the
mother
The child will experience behavioural, social or learning difficulties
The child will develop depression in adolescence (CHIMAT)
Maternal depression increases the risk of mental illness in children to the extent that they are five times more likely to have a mental health problem, more than three times more likely to have an emotional problem that persists for at least three years and almost seven times more likely to have conduct problems that persist for at least three years (DH, 2011).
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 11
5 Service Delivery
Universal Service
These are services for all families. Health visitors deliver the Healthy Child Programme to ensure a health start for children and families, including immunisations, health and development checks, support for parents and access to a range of community services/resources. The current health visitor contacts in the first year include:
Antenatal
New birth visit
6 weeks
10 months to 1 Year
5.1 Universal Plus
Targeted according to assessed or expressed needs, universal plus gives a rapid response from the health visiting team when families need specific expert help, for example all women identified with a mild to moderate mental health problems to be offered a range of support. For example, wellbeing advice, short term guided self-help such as solution focus approaches, motivational interviewing, cognitive behaviour therapy, ‘Think Family’ Whole Family Approach, (appendix 5) promotional interviewing, medication and baby massage. (Guidance (DH 2012) (Appendix 1)
5.2 Universal Partnership Plus
Targeted according to identified need. Universal Partnership Plus provides on-going support from the team or family nurse partnership plus range of local services working together with families to deal with more complex issues over a period of time. These include services from Sure Start Children’s Centres, the third sector, specialist mental health services, GP, housing, welfare and social care. (Appendix 1)
5.3 Safeguarding
This is a high level core objective. Safeguarding is of paramount importance and local areas need to ensure there are clear protocols in place, which offer clarity regarding the roles and responsibilities of health visitors and midwives.
6.0 Purpose
This document supports national strategy for Health Visiting and the Healthy Child programme (DH 2009) supporting mothers during perinatal period and extending to one year post delivery. This also includes use of assessment tools e.g. Whooley questions (NICE), (EPDS) Edinburgh Postnatal Scale as per LPT Standard
Operational Procedures (2012)(SOP)
Prediction and Detection
At a woman’s first contact with services in both the antenatal and the postnatal periods, all health care professionals should ask questions about:
Past or present severe mental illness including schizophrenia, bipolar disorder, puerperal /psychosis and severe depression.
Previous treatment by a psychiatrist/specialist mental health team including inpatient care.
A family history of perinatal mental illness (including puerperal psychosis).
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 12
Other specific predictors, such as poor relationships with her partner, should not be used for the routine prediction of the development of the mental disorder. (NICE,45)
At a woman’s first contact with the health visiting service at the antenatal contact and in the postnatal period (at new birth visit and 6 weeks), health care professionals should ask two questions to identify possible depression. The woman should be informed of the reasons for asking the NICE 2007 questions and what is recorded on her records. Consent must be obtained in-line with Leicestershire Partnership Trust protocols with due regard to safeguarding and vulnerable adult priorities
Questions
During the past month, have you often been bothered by feeling down, depresses or hopeless?
During the past month, have you often been bothered by having little interest or pleasure in doing things?
A third question should be considered if the woman answers “yes” to either of the initial questions.
Is this something you feel you need or want help with? (NICE, 45)
The health visitor may also use the EPDS tool at this stage
When asking these questions the practitioner should consider the following;
The practitioner should ensure privacy
If there are language/cultural or communication difficulties that would make it difficult to ask the ‘Whooley’ questions verbatim, other methods of assessing maternal mental health should be considered. For example on a scale of 1 to 10 how are you feeling (10 being the worst) Many cultures express their emotional distress through physical symptoms.
If any serious mental health problems are identified women should be referred to their GP please see Pathway (appendix 6)
A risk assessment needs to be made to determine whether the mother is at risk of harming herself or her children. This should be done using the knowledge and skill acquired via the MMH training with the help of the various recommended assessment tools to help support your clinical judgment. (See pathway appendix 6)
If a woman has a pre-existing mental illness, she may need to continue input from the CMHT
7.0 Roles and Responsibilities
Evidence based mandatory specialist training and education for health visitors in early assessment, screening, treatment and management of postnatal depression is essential. All health visitors are expected to keep up to date with this sphere of practice. The health visitors will remain the key named health professional and will undertake any on-going assessments. It will be the Health V isitor’s clinical decision to refer to GP, other agencies, specialist and other support services, such as MIMS.
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 13
Standards to be achieved in the development of procedural documents
For Nursery Nurses (within the health visitor team) to be able to screen mothers at any contact where they may see the mother during the first year, for example at a weaning teaching session ; by appropriately asking the ‘Whooley’ questions they must be competent in interpreting the non-verbal responses as well as the verbal response and recording and reporting back any factors to the health visitor. They must not undertake this role unless they have undertaken the training.
The health visitors must respond in a timely manner to make an assessment of the predictive risk factors taking into account historical as well as present indicators of maternal mental health; including wider determinants of health that may be compounding the issues involved. The HV must take appropriate action to address the various issues documenting the rationale and action plans in concordance with the client and child/children being paramount and central in line with LSCB and early intervention expectation.
Mandatory Training
All Health Visitors will receive a two day Perinatal Maternal Mental Health recognised training programme as outlined nationally by Department of Health
(DH 2013) for Health visitors. Trainers who deliver the training will have undertaken the official training package (PND Champions
– IHV 2013, DH
2013).
All Health Visitors are expected to keep up to date with this sphere of practice with their continual practice development (The Code, Nursing Midwifery Council
2008)
Community Child Health Nurse and Community Nursery Nurse will receive one day (Day 1) awareness training to support HV’s on early screening and referring to family health visitors
Supervision
HV’s can access specialist clinical supervision. (LPT Clinical Supervision
Policy, 2012)
Partnership alignment with perinatal psychiatric team to provide joint specialist supervision with approved PND champion trainers. This supervision sits in line with existing trust’s supervision policy.
Any health professional that requires additional support must seek advice and support from their line manager or named nurse if required.
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 14
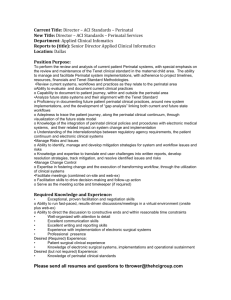
Appendix 1
Pathway for Identification, Screening, Management and Treatment of Perinatal Maternal
Mental Health for Health Visiting Services.
Universal Healthy Child Programme Contacts
Assessment as per Standard Operating Procedure.
Low Risk
(Universal)
Moderate Risk
(Universal Plus)
Agreed package of care
Up to 4-6 listening visits
Liaise with GP
Offer other support activities local to the
Neighbourhood
Monitor progress using professional judgment in line with Perinatal Mental
Health Guidelines using
Whooley Questions, EPDS
High Risk (Universal
Partnership Plus)
Emergency action:
Tel: 0300 3001010
Assess the risk of suicide
Get immediate specialist advice from
GP or Crisis team.
Take appropriate action:
Liaise with GP
CPN, CMHT, and
Psychiatrist and agree lead professional
No Improvement, refer to GP/Health Visitors can refer to Perinatal
Psychiatry Service
(appendix 4) using their professional judgment and a clear rationale.
The GP should always be notified
Situation improved / resolved - back to
Universal Services
Non-Emergency
Action
Liaise with GP within 24 hours
Liaise with
Psychiatric services as required
Mother’s mental health should be assessed at all Universal Contacts in the perinatal period
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 15
Appendix 2
Edinburgh Postnatal Depression Scale (EPDS) for Postpartum Depression
Edinburgh Postnatal Depression Scale (EPDS) was developed by J.L. Cox and J.M.
Holden in 1987 for screening postpartum women in outpatient, home visiting settings, or at the 6 – 8 week postpartum examination. It has been utilised among numerous populations, including USA and Spain. The scale has since been validated, and evidence from a number of research studies has confirmed the tool to be both reliable and sensitive in detecting depression.
The EPDS consists of 10 questions and can usually be completed in less than 5 minutes.
Validation studies have utilised various threshold scores in determining which women were positive and in need of referral. Cut – off scores range from 9 – 13 points. A woman scoring
9 or more points or indicating any suicidal intention
– that is, she scores 1 or higher on question 10 – should be referred immediately.
The EPDS score should not override clinical judgement. A careful clinical assessment should be carried out to confirm the diagnosis. The scale indicates how the mother has felt during the previous week. In doubtful cases it may be useful to repeat the tool after 2 weeks.
The scale will not detect mothers with anxiety neuroses, phobias, or personality disorders.
SCORING
Questions 1, 2, and 4 (without an *) are scored 0, 1, 2, or 3, with the top score as a 0 and the bottom box scored as a 3.
Question 3 and 5-10 (marked with an *) are reverse – scored, with the top box scored as a 3 and the bottom box as 0.
Maximum score: 30
Possible Depression: 10 or higher
Always look at question 10, which indicates suicidal thoughts. If this is highlighted immediate action is required
INSTRUCTIONS
1. The mother is asked to underline 1 of 4 possible responses that comes the closest to how she has been feeling the previous 7 days.
2. All 10 items must be completed.
3. Care should be taken to avoid the possibility of the mother discussing her answers with others.
4. The mother should complete the scale herself, unless she has limited English or has difficulty with reading.
*Source: Cox JL, Holden JM, Sagovsky R. Detection of Postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. BR J Psychiatry. 1987;150:782-786.
Users may reproduce the scale without further permission providing they respect copyright by quoting the names of the authors, the title, and the source of the paper in all reproduced copies.
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 16
Appendix 3
Edinburgh Postnatal Depression Scale (EPDS) Form
Name:____________________________________
Address:__________________________________
Your Date of Birth:__________________________
Baby’s Date of Birth:________________________
Phone:___________________________________
SIMPLE QUESTION:
As you are pregnant or have recently had a baby, we would like to know how you are feeling. Please check the answer that comes closest to how you have felt IN THE PAST 7 DAYS, not just how you feel today.
Here is an example, already completed.
□
I have felt happy:
□
Yes, all of the time
□
Yes, most of the time
□
No, not very often
□
No, not at all
ₓ
This would mean: “I have felt happy most of the time” during the past week. Please complete the other questions in the same way.
In the past 7 days:
I have been able to laugh and see the funny side of things
□
As much as I always could
□
Not quite so much now
□
Definitely less than I used to
□
Not at all
I have looked forward with enjoyment to things
□
As much as I ever did
□
Rather less than I used to
□
Definitely less than I used to
□
Hardly at all
I have blamed myself unnecessarily when things went wrong
□
Yes, most of the time
□
Yes, some of the time
□
Not very often
□
No, never
I have been anxious or worried for no good reason
□
No, not at all
□
Hardly ever
□
Yes, sometimes
□
Yes, very often
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 17
I have felt scared or panicky for no good reason
□
Yes, quite a lot
□
Yes, sometimes
□
No, not much
□
No, not at all
Things have been getting on top of me
□ Yes, most of the time I haven’t been able to cope at all
□ Yes, sometimes I haven’t been coping as well as usual
□
No, most of the time I have coped quite well
□
No, I have been coping as well as ever
I have been so unhappy that I have had difficulty sleeping
□
Yes, most of the time
□
Yes, sometimes
□
No, most of the time I have coped quite well
□
No, I have been coping as well as ever
I have felt sad or miserable
□
Yes, most of the time
□
Yes, quite often
□
Not very often
□
No, not at all
I have been so unhappy that I have been crying
□
Yes, most of the time
□
Yes, quite often
□
Only occasionally
□
No, never
The thought of harming myself has occurred to me
□
Yes, quite often
□
Sometimes
□
Hardly ever
Administered/Reviewed
By:__________________________________
Date:_________________________________
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 18
Appendix 4
PERINATAL PSYCHIATRY SERVICE REFERRAL FORM
Request for: Maternity ward assessment / Out-Patient appointment (Please delete as appropriate)
PLEASE COMPLETE ALL THE SECTIONS BELOW IN DETAIL AND IN BLOCK LETTERS
Title: ………. Surname:…………………… GP Name:……………………………………...
Forename:…………………………………... GP Address…………………………..…….....
Address:…………………………………….. ………………………………………….…….....
………………………………………………… ………………………………………………......
Patient’s Postcode:………………………. GP’s Post code:……………………………….
Patient’s Phone No:……………………… GP’s Phone No:……………………..……......
Dob:………………………………………… NHS No……………………………….…….......
Ethnicity:…………………………………… Weeks Pregnant/Postnatal:.…………….......
Religion:……………………………………. Expected date of delivery:…………………..
Marital Status:…………………………….. Expected place of delivery:…………………
Main Language:…………………………… Translator Needed: Yes / No
Current Medication:…………………………………………………………………………………
Reason for Referral (Please continue on separate sheet if necessary):
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
………………………………………………………………………………………………………………………
Referred by: GP / Midwife / Consultant / HV / Other…………
Name of referrer:……………………………………………
Contact Address:……………………………………………
…………………………………………………………………
Contact Phone No……………………Date……………………
.
Please fax completed form to:
O116 2314833
Dr R Lazarus
Consultant, Perinatal Psychiatry
Farm Lodge, c/o Bradgate Unit
Glenfield Hospital
Tel. 0116 2256846
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 19
Appendix 5
Think Family (Whole Family Approach)
Think Family/Whole Family: Supporting Mentally Ill Parents and their Children
Significance for Maternal Mental Health and Health Visitors Practice
(Summary document for inclusion in the Perinatal Maternal Mental Health Guidance document for Health Visitors)
Leicestershire Partnership Trust (LPT) Think Family/Whole Family Approach (definition): An
Approach used to support Parents with Mental Illness and their Children through multiagency collaboration and work with the whole family
Lead: Dr Lina Gatsou, Consultant Child and Adolescent Psychiatrist and LPT Named Doctor for Safeguarding Children
Summary of theory, research, and relevant policies:
Parental Mental Illness is a family matter – the presence of a parent and especially a mother with mental illness in the family with dependent children may lead to many alterations in its system
– such as changes in family structure and interpersonal relationships that can cause adverse outcomes for children (Rose et al., 2002). Several studies indicate that children where a mother has a mental illness may be at twice the risk of developing a mental illness diagnosis compared to other children (Black et al., 2003; Park et al., 2003; Cunningham et al., 2004; Leschied et al., 2005; Edwards et al., 2006) and might face a range of behavioural, interpersonal, academic and other difficulties (Rutter & Quinton 1984; Farahati et al. 2003;
Maughan et al. 2007; Reupert & Maybery 2007; Reupert et al. 2011). In turn
– since maternal and children’s mental health and emotional wellbeing are intertwined and closely related, particularly during the early years of child’s life – difficulties with parenting, mother–child relationship, and children’s behavioral, emotional and social difficulties can cause worsening of the maternal mental health (Falkov, 2012). Similarly, the NICE Clinical Guideline 45:
‘Antenatal and Postnatal Mental Health: Clinical Management and Service Guidance’ (2007) states: ”Mental disorders during pregnancy and the post natal period can have serious consequences for the health and wellbeing of a mother and her baby, as well for her partner and other family members”.
Guidance to support Health Visitors and their Teams with Perinatal Maternal Mental Health Page 20
In conclusion, any attempt to improve the life chances for the mentally ill mothers and their babies must consider their family context and must be based on a good understanding of the needs of children and their mentally ill parents (Falkov, Royal College of Psychiatrists, 2011).
The above noted issues surrounding living with a mother with mental illness emphasise the need for programmes that recognise parental responsibilities of adults with mental illness and assess and support the whole family (Oscouie et al., 2011). Such programs have benefits for the parent with mental illness, the children, and other family members, and they can reduce future costs to the health care system (Mi-halopoulos, Magnus, Carter, & Vostanis, 2004).
Implementing such programs can improve medication adherence and reduce symptom relapse of the parents with mental illness (Re-upert, Green, & Maybery, 2008); in addition, by working on childparent interactions, such programs can reduce the child’s burden and eventually improve their functioning (Miklowitz, George, Richards, Simo¬neau, & Suddath,
2003) and prevent further decline in their emotional wellbeing.
Leicestershire Partnership Trust approach in supporting mentally ill parents and their children has been named Think Family/ Whole Family Approach. The development of the programme started in 2010, and its implementation started in 2011. This approach is crucial in supporting maternal mental health and its relevant elements to the health visitors practice, in summarised form, are the following:
1. Strategic Development: Think Family /Whole Family Strategy and Think Family /Whole
Family Divisional Action Plans (2011/2012)
2. Screening, Assessment and Service Delivery Review for Parents with Mental Illness and their Children: Think Family/ Whole Family Audit of CAMHS, AMHS and LD
(2012-2013)
•
•
•
3. Workforce Development and Training: Think Family / Whole Family Training and
Intervention
Basic training incorporated in the LPT Induction & Safeguarding Training / Interagency
Training for all LPT staff (started in 2011)
½ day Awareness Training for newly qualified and existing Health Visitors (started in
2012)
2-day HIEC Think Family/ Whole Family Multi-agency Training and Family Intervention
(100 multi-agency professionals – and amongst them a substantial number of HV – have been trained in 2012); ongoing role and roll out of the training is being discussed
(LPT safeguarding and divisional leads)
February 2014
Dr Lina Gatsou (Consultant Child and Adolescent Psychiatrist and LPT Named Doctor for
Safeguarding Children)
Filippa Howells (Practice Educator for FYP&C)
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 21
Checklist for the Review and Approval of Procedural Document
To be completed and attached to any document which guides practice when submitted to the appropriate committee for consideration and approval.
Title of document being reviewed:
Yes/No/Not applicable
Comments
Will any sections of this Policy satisfy one or more criteria of the NHSLA Risk Management Standards?*
If Yes – Have you attached the relevant self-assessment(s) for those criteria as an appendix?*
* for further guidance consult the Trust Lead for Corporate Risk Assurance:
Richard.Apps@leicspart.nhs.uk
1. Title
2.
Is the title clear and unambiguous?
Is it clear whether the document is a guideline, policy, protocol or standard?
Key Points / Changes to the Policy
Yes
Yes
States it is guidance on the title
3. Rationale
4.
5.
Are reasons for development of the document stated?
Development Process
Does the front page include a sentence which summarises the contents of the policy?
Is the method described in brief?
Are people invited in the development identified?
Do you feel a reasonable attempt has been made to ensure relevant expertise has been used?
Is there evidence of consultation with stakeholders and users? (with representatives from all relevant protected characteristics)
Content
Is the objective of the document clear?
Is the target population clear and unambiguous?
Are the relevant CQC outcomes identified?
Are the intended outcomes described?
Yes
Yes
N/A
Yes
Yes
Yes
Yes
Yes
Yes
Yes
Develop proficiencies in this specialised area of work
It is in the title
Flowchart
Wide range evident
Audit undertaken in the
County
In the introduction
Training will reinforce this
Care
Pathway
From A3 copy
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 22
Are the statements clear and unambiguous? Yes
6. Evidence Base
Is the type of evidence to support the document identified explicitly?
Are key references cited?
Are the references cited in full?
Is there evidence to show that there has been due regard under the Equality Act 2010, and in working towards the
Trust’s equality objectives? (e.g. attach the equality analysis as summary of evidence)
Are supporting documents referenced?
Yes
Yes
Yes
7. Approval
Does the document identify with committee/group will approve it?
If appropriate have the joint Human Resources/staff side committee (or equivalent) approved the document?
8. Dissemination and Implementation
Is there an outline/plan to identify how this will be done?
Does the plan include the necessary training/support to ensure compliance?
9. Document Control
Does the document identify where it will be held?
Have archiving arrangements for superseded documents been addressed?
10. Process to Monitor Compliance and Effectiveness
Are there measurable standards or KPIs to support the monitoring of compliance with and effectiveness of the document?
Is there a plan to review or audit compliance with the document?
11. Review Date
Is the review date identified? 3 years. 2016
12. Overall Responsibility for the Document
Is it implicit who will be responsible for co-ordinating the dissemination, implementation and review of the document?
Is the frequency of review identified? If so it is acceptable?
No
Individual Approval
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams
It has been widely circulated
It is fully referenced
Page 23
If you are happy to approve this document, please sign and date it and forward to the chair of the committee/group where it will receive final approval.
Name Date
Signature
Committee Approval
If the committee is happy to approve this document, please sign and date it and forward copies to the person with responsibility for disseminating and implementing the document and the person who is responsible for maintaining the organisation’s database of approved documents.
Name Date
Signature
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 24
Board Adoption Template
The following documents have been reviewed by the Policy Group to ensure compliance with relevant standards and legislation.
Name of Policy Committee Responsible for Approving Policy
Identification, screening, treatment and referral of perinatal MMH Policy for the HR
Service.
Date Policies Adopted by Board:
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 25
Staff Authorise Document Receipt
Signature Sheet for Approved Policies and Procedures
Name of Policy:
Statement:
I have read the above and understand its contents. If there any difficulties regarding implementation or any training needs, I have raised and resolved these with my line manager.
I agree to implement the content of the above policy.
Staff Name Signature Date
On completion this sheet will be kept by the line manager and become part of the training record.
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 26
Table for Process for Monitoring Compliance and Effectiveness
Systems
Criteria Measurables Frequency
Monitoring and/or Audit
Reporting to
P.A.E. Systems in place to ensure that
Policy Leads follow the process outline in this guidance document
Systems in place for:
Distribution (including version control)
Monitoring of implementation
Plan
Implementation
Timely review of all policies and procedures including equality analysis
Archiving/Retention/Destruction of policies
Criteria for preliminary approval are met as per
Checklist
Database showing status of all current policies
How implemented?
Gaps in information
Timescales met?
How many achieved?
Result of Audit
As required by policy review
Quarterly P.A.E.
Guidance to support Health Visitors and their Teams with Perinatal Maternal Mental Health Page 27
Action Plan / Monitoring
Monitoring/Action Plan
Monitoring/Action Plan
Systems
Criteria
Systems in place to monitor comments received regarding the viability of policy in the services
Measurables
Number of comments received
Frequency
Quarterly
Monitoring and/or Audit
Reporting to
P.A.E.
Action Plan/Monitoring
Action Plan to address comments
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 28
8.0 References & Associated Documentation
This policy was drafted with reference to the following:
Adams H (March 2012) Maternal Mental Health Pathway, can Health Visitors succeed in delivering maternal mental health service in the absence of fidelity to a model/pathway?
Barlow J, Coe C (2013) New ways of working: Promotional interviewing in health visiting practice. Journal of Health Visiting, 1(1), p44-50
Brugha TS, Morrell CJ, Slade P and Walters SJ (2011)Universal prevention of depression in women postnatally, cluster randomized trial evidence in primary care. Psychological
Medicine, v295, p449-507
Cowley S, Whittaker K, Grigulis A, Malone M, Donetto S, Wood H, Morrow E and Maben
J (2013)Why Health Visiting? A review of the literature about key health visitor interventions, processes and outcomes for children and families. London: National
Nursing Research Unit, King’s College London.
Cox JL, Holden JM, Sagovsky R (1987) Detection of postnatal depression.
Development of the 10 item Edinburgh PND scale. BR J Psychiatry 150: 782-6
Cubison J and Munroe J (2005) Acceptability of using the EPDS as a screening tool for depression in the postnatal period. In Screening for Perinatal Depression (eds C
Henshaw and S Elliot), London: Jessica Kingsley Publishers.
Department of Health (DH) (2009) Healthy Child Programme: pregnancy and the
First five years of life. London: DH
Department of Health (2009) Healthy Child Programme; Pregnancy and the first five years of life
Department of Health (2011) No Health without Mental Health: A cross-Government mental health outcomes strategy for people of all ages. Analysis of the Impact on Equality
(AIE) Annex B - Evidence Base Supporting document
Dr Foster http://en.wikipedia.org/wiki/Category:Department_of_Health_(United_Kingdom)
Hogg,S. (2013) Prevention in Mind All Babies Count: Spotlight on Perinatal Mental Health.
NSPCC
Joint Commissioning Panel for Mental Health (2012) Guidance for commissioners of perinatal and mental health services
Leicestershire PT., Clinical Supervision Policy (2012)
Lewis G (ed) (2011) Saving Mothers’ Lives. Reviewing maternal deaths to make motherhood safer: 2006 –2008. Confidential Enquiries into Maternal Deaths in the UK –
Eighth report. Centre for Maternal and Child Enquiries (CMACE)
Murray L et al (2011)Maternal Postnatal depression and the development of depression in offspring up to 16 years of age. J of the American Academy of Child and Adolescent
Psychiatry. 50L5) 460-470
National Institute for Health and Clinical Excellence (2007) Antenatal and postnatal mental health: clinical management and service guidance. London NICE
Guidance to support Health Visitors and their Teams with Perinatal Maternal Mental Health Page 29
National Institute for Health and Excellence (NICE) (2007) Antenatal and postnatal mental health: Clinical management and service guidance CG45.
National Mental Health Development Unit (2011) National Perinatal Mental Health Project
Report Perinatal Mental Health of Black and Minority Ethnic Women: A Review of Current
Provision in England, Scotland and Wales.
Nursing and Midwifery Council 2008, The Code, NMC
Oates M., & Cantwell, R. (2011). Deaths from psychiatric causes. Centre for Maternal and
Child Enquiries (CMACE), BJOG 118 (Suppl. 1) 132-203.
Perinatal mental health; Key aspects and evidence base Royal College of Nursing
Available at http://www.rcn.org.uk/development/communities/rcn_forum_communities/mental_health/f orums/womens_mental_health_group/specialist_pages_on_best_practice/perinatal_ment al_health.%20Accessed%20July%202013
Royal College of Obstetricians and Gynaecologists (RCOG) (2011) Management of women with mental health issues during pregnancy and the postnatal period. Good practice No.14
Royal College of Obstetricians and Gynaecologists. TOG release: Managing teenage pregnancy. Available at http://www.rcog.org.uk/news/tog-release-managing-teenagepregnancy. Accessed July 2013
Whooley MA, Avins AL, Miranda J, Browner WS (1997) Case finding instruments for depression. Two questions are as good as many. J Gen Intern Med 12 (7): 439 -45
Wisner K et al (2013)Onset Timing, Thoughts of Self-harm, and Diagnoses in Postpartum
Women with Screen-Positive Depression Findings, JAMA Psychiatry, p1-9.
Cunningham, J., Harris, G., Vostanis, P., Oyebode, F. & Blissett, J. (2004) Children of mothers with mental illness: attachment, emotional and behavioural problems. Early Child
Development and Care, 174, 639
–650
Park, R.J., Senior, R. & Stein, A. (2003) The offspring of mothers with eating disorders.
European Child & Adolescent Psychiatry, 12, 110 –119.
Maughan, A., Cicchetti, D., Toth, S. & Rogosch, F. (2007) Early-occurring maternal depression and mat ernal negativity in predicting young children’s emotion regulation and socioemotional difficulties. Journal of Abnormal Child Psychology, 35, 685
–703.
Falkov A., (2011) Parents as Patients, Royal College of Psychiatrists, London
Oscouie, F. Zeigham, R. Joolaee, S. (2011) Outcomes of Parental Mental illness on
Children; A qualitative study from Iran. Journal of Psychosocial Nursing, 49: 9, 2011
Rutter, M. & Quinton, D. (1984) Parental psychiatric disorder: effects on children.
Psychological Medicine, 14, 853 –880
Reupert, A.E. & Maybery, D.J. (2007) Families affected by parental mental illness: issues
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 30
and intervention points for stakeholders. American Journal of Orthopsychiatry, 77, 362 –
369
Reupert, A. Foster, K. Maybery, D. Eddy, K. Fudge, E (2011) Keeping families and children in mind: an evaluation of a web-based workforce resource, Child and Family
Social Work. Child and Family Social Work, 16, 192 –200
Perinatal Maternal Mental Health Guidance to support Health Visitors and their Teams Page 31