A cura di Rossella Iuliano THE LYMPHATIC SYSTEM
advertisement

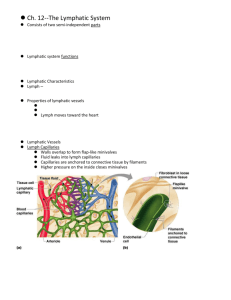
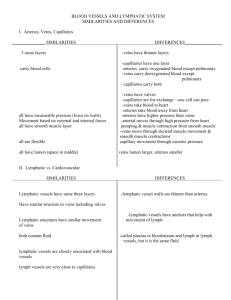
A cura di Rossella Iuliano THE LYMPHATIC SYSTEM INTRODUCTION The lymphatic system has always been known, since Hippocrates, as the “white blood” of organisms. It is a part of the immune system used to remove fluids and proteins from tissues and pour them back into the bloodstream. The parts identified as the ones it is composed of are : interstitium, lymphatic vessels, lymphatic organs and migrating cells[1]. It is involved in a lot of diseases, such as cancer, lymphedema, asthma and various inflammatory diseases. This is the reason why everyone works in the sanitary sector needs to pay attention on structure and function of lymphatic vessels, whit all of them branches directed to the ductus thoracicus and ductus lymphaticus dexter as far as large veins. Hodgkin’s Linphoma STRUCTURE AND FUNCTION Studies on bioptic and on necrotic human material had disclosed very difficulties into the differentiation of blood capillaries and lymphatic vessels, especially considering that also the second ones have a kind of valves [2]. Nevertheless in 1990 the lymphangiogenesis and the endothelium of lymphatic capillaries were analyzed and the vascular endothelial growth factor receptor-3 was discovered, among others specific molecule functional for this system, with its ligand VEGF-C [3]. Baruk et al. described the effect of growth factors on lymphatic vessels in mice affected by chronic respiratory tract infection. The inhibition of VEGFR-3 did not let lymphatic vessels grow up but it was different for blood vessels, while VEGF-C and VEGF-D were able to cause a contrary effect. Another important result was obtained by Banjeri et al. [4] when they visualized the endothelium of limphatic vessels thanks to LYVE-1 antibodies, i.e. markers for a protein on the surface of this tissue. However both blood and lymphatic vessels are essential for the microcirculation in the loose connective tissue [5], composed of the two types of vessels and of its own interstitium. The last one contains matrix, with fibers (collagen, elastic and reticular fibers) and amorphous substance (glycosaminoglycans, proteoglycans and glycoproteins). Hyaluronan is the glycosaminoglycan), which acts as a base of support for immune cells and is degraded in regional lymph nodes or in the liver after being let in bloodstream[6]. Leukocytes, instead, go away from blood and recognize antigens to defend the body from all the possible external attach by an outside being. But the filtration in blood capillaries and venules must be controlled because it can be dangerous, originating an edema if the lymphatic drainage is insufficient [7]. Edema is avoided because of filtration, readsorbition into blood capillaries, and clearance into lymphatic capillaries. They take plasma proteins when the edematous fluid has more than 10 g/L of proteins but, in this case, also macrophages can act and realize proteolysis. Lymphatic vessels also move fluid against hydrostatic gradient with them contractions, regulated by catecholamines, which stimulate adrenergic and cholinergic nerves in lymphatic vessels walls. Moreover this system transports blood cells, as it was seen in limbs and sheeps [8], and a lymphocytes physiological recirculation from postnodal lymph to the bloodstream in “endothelial venules” was described, too [9]. After the lymphocytes migrate from the bloodstream into the lymph [10]. The cycle is repeated for 12-24 hours, and if no antigens are found, the lymphocytes die [11]. In case of inflammatory affection, T lymphocytes enter into lymphatic vessels thanks to chemokine receptor CCR7 [12]; the same recirculation from peripheral tissues exists also during the ontogenetic development [13], just to assure a suited migration to the bloodstream to make an immune response. For these reason it is very important afferent lymphatic vessels’rule, because they transport cells to the regional lymph nodes, also the dendritic cells, which present antigens to T lymphocytes before entering prenodal lymph. The afferent lymph contained apoptotic cells and there are cell debris in the lymphatic capillaries of the synovial membrane [14]. But the drainage function recognized to this system also in synovial membrane has been described as a consequence of specialized inter-endothelial junctions, too [15 ]. The externals extension of the endothelial cells are, in fact, anchored to the connective tissue but the internal ones can enter the lymphatic capillaries and create a communication among them and the interstitium. When the pressure in the connective tissue exceeds, the internal extension cover up the external one. Because of this function, but also for them morphology, inter-endothelial junctions are called primary valves. Fig1. Lymph node CONCLUSION Lymphatic system is the guardian of tissues’ fitness, because it guarantees the immune response by transporting lymphocytes, stimulating antibodies production and evoking the activation of lymphonodes. Moreover it is involved into the migration of neoplastic cells because they pass into its vessels but are degraded, in the best of chances, before causing a metastasys. Fig 2. Infiltration of a lymph node capsule by neoplastic cells. BYBLIOGRAPHY 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. Olszewski WL. Interrelationships within the lymphatic system. In: Olszewski WL, ed. Lymph Stasis. Pathophysiology, Diagnosis and Treatment. Bocca raton: CRC Press, 1991: 512. Emìlia Rovenskà MD PhD and Jozef Rovensky MD DSc FRCP, National Institute of Rehumatic Diseases, Piestany, Slovak Republik. Lymphatic Vessels: Structure and Function. Kulek E, Lymboussaki A, Taira S, et al. VEGF-C receptor binding and pattern of expression with VEGFR-3 suggests a role in lymphatic vascular development. Development 1996; 122: 3829-37. Banjeri S, Ni J, Wang SX et al. LYVE-1, a new homologue of the CD44 glycoprotein, is a lymph-specific receptor for hyaluronan. J Cell Biol 1999; 144:789-801. Skobe M, Detmar M. Structure, function and molecular control of the skin lymphatic system. J Invest Dermatol Symp Proc 2000; 5:14-19. Liu EN. Trafficking of hyaluronan in the interstitium and its possible implications. Lymphology 2004; 37: 6-14. Witte MH, Whitte ChL. Lymph formation > lymph absorption: the formula of edema. Lymphology 1973; 6:101-9. Smith JB, McIntosh GB, Morris B. The traffic of cells through tissues: a study of peripheral lymph in sheep. J Anat 1970; 107: 87-100. Gowans JL, Knight EJ. The route of recirculation of lymphocytes in the rat. Proc R Soc B 1964; 159:257. Hall JG. An essay in lymphocytes circulation and the gut. In Trnka Z, Cahill RN, eds. Essays on the anatomy and physiology of lymphoid tissues. Basel: S. Karger, 1980: 100-11. Salmi M, Jalkanen S. How do lymphocytes know where to go: current concepts and enigmas of lymphocytes homing. ADV Immunol 1997; 64: 139-218. Debes GE, Arnold CN, Young AJ, et al. Chemokine receptor CCR7 required for T lymphocytes exit from peripheral tissues. Nature Rev Immunol 2005; 6: 889-94. Cahill RNP, Kimpton WG, Washington EA, et al. the ontogeny of T cell recirculation during foetal life. Semin Immunol 1999; 11: 105-14. 14. Rovenka E, Rovenska E jr, Neumuller J. Structure of synovial lymphatic capillaries in rheumatoid arthritis and juvenile idiopathic arthritis. Int Tissue React 2003; 24: 29-38. Rovenska E, Stvrtina S, Greguska O, et al. Conspicuous synovial lymphatic capillaries in juvenile idiopathic arthritis synovitis with rice bodies. Ann Rheum Dis 2005; 64:328-9. 15. Leak LV, Burke JE. Fine structure of the lymphatic capillary and the adjoining connective tissue area. Amer J Anat 1966; 118: 785-810.