Renal - WordPress.com
advertisement
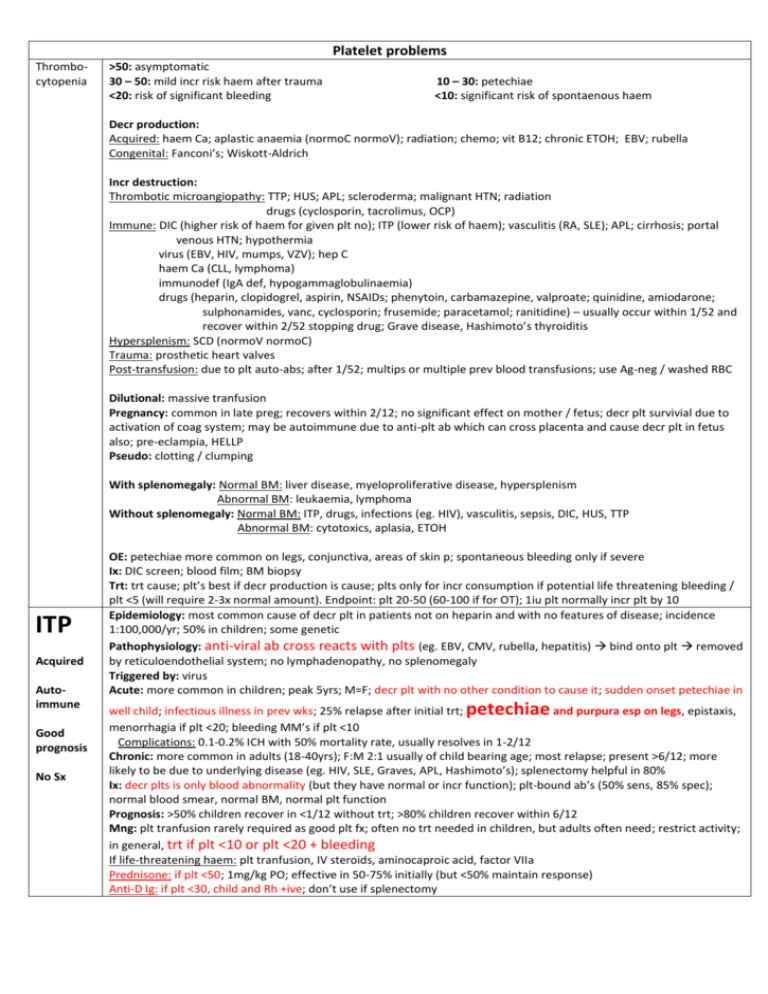
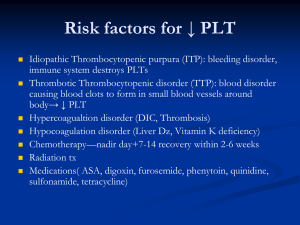
Platelet problems Thrombocytopenia >50: asymptomatic 30 – 50: mild incr risk haem after trauma <20: risk of significant bleeding 10 – 30: petechiae <10: significant risk of spontaenous haem Decr production: Acquired: haem Ca; aplastic anaemia (normoC normoV); radiation; chemo; vit B12; chronic ETOH; EBV; rubella Congenital: Fanconi’s; Wiskott-Aldrich Incr destruction: Thrombotic microangiopathy: TTP; HUS; APL; scleroderma; malignant HTN; radiation drugs (cyclosporin, tacrolimus, OCP) Immune: DIC (higher risk of haem for given plt no); ITP (lower risk of haem); vasculitis (RA, SLE); APL; cirrhosis; portal venous HTN; hypothermia virus (EBV, HIV, mumps, VZV); hep C haem Ca (CLL, lymphoma) immunodef (IgA def, hypogammaglobulinaemia) drugs (heparin, clopidogrel, aspirin, NSAIDs; phenytoin, carbamazepine, valproate; quinidine, amiodarone; sulphonamides, vanc, cyclosporin; frusemide; paracetamol; ranitidine) – usually occur within 1/52 and recover within 2/52 stopping drug; Grave disease, Hashimoto’s thyroiditis Hypersplenism: SCD (normoV normoC) Trauma: prosthetic heart valves Post-transfusion: due to plt auto-abs; after 1/52; multips or multiple prev blood transfusions; use Ag-neg / washed RBC Dilutional: massive tranfusion Pregnancy: common in late preg; recovers within 2/12; no significant effect on mother / fetus; decr plt survivial due to activation of coag system; may be autoimmune due to anti-plt ab which can cross placenta and cause decr plt in fetus also; pre-eclampia, HELLP Pseudo: clotting / clumping With splenomegaly: Normal BM: liver disease, myeloproliferative disease, hypersplenism Abnormal BM: leukaemia, lymphoma Without splenomegaly: Normal BM: ITP, drugs, infections (eg. HIV), vasculitis, sepsis, DIC, HUS, TTP Abnormal BM: cytotoxics, aplasia, ETOH ITP Acquired Autoimmune Good prognosis No Sx OE: petechiae more common on legs, conjunctiva, areas of skin p; spontaneous bleeding only if severe Ix: DIC screen; blood film; BM biopsy Trt: trt cause; plt’s best if decr production is cause; plts only for incr consumption if potential life threatening bleeding / plt <5 (will require 2-3x normal amount). Endpoint: plt 20-50 (60-100 if for OT); 1iu plt normally incr plt by 10 Epidemiology: most common cause of decr plt in patients not on heparin and with no features of disease; incidence 1:100,000/yr; 50% in children; some genetic Pathophysiology: anti-viral ab cross reacts with plts (eg. EBV, CMV, rubella, hepatitis) bind onto plt removed by reticuloendothelial system; no lymphadenopathy, no splenomegaly Triggered by: virus Acute: more common in children; peak 5yrs; M=F; decr plt with no other condition to cause it; sudden onset petechiae in petechiae well child; infectious illness in prev wks; 25% relapse after initial trt; and purpura esp on legs, epistaxis, menorrhagia if plt <20; bleeding MM’s if plt <10 Complications: 0.1-0.2% ICH with 50% mortality rate, usually resolves in 1-2/12 Chronic: more common in adults (18-40yrs); F:M 2:1 usually of child bearing age; most relapse; present >6/12; more likely to be due to underlying disease (eg. HIV, SLE, Graves, APL, Hashimoto’s); splenectomy helpful in 80% Ix: decr plts is only blood abnormality (but they have normal or incr function); plt-bound ab’s (50% sens, 85% spec); normal blood smear, normal BM, normal plt function Prognosis: >50% children recover in <1/12 without trt; >80% children recover within 6/12 Mng: plt tranfusion rarely required as good plt fx; often no trt needed in children, but adults often need; restrict activity; in general, trt if plt <10 or plt <20 + bleeding If life-threatening haem: plt tranfusion, IV steroids, aminocaproic acid, factor VIIa Prednisone: if plt <50; 1mg/kg PO; effective in 50-75% initially (but <50% maintain response) Anti-D Ig: if plt <30, child and Rh +ive; don’t use if splenectomy TTP Nonimmune Poor prognosis Neuro Sx HUS Microangiopathic Renal Sx Good prognosis Ig: if plt <5 / internal haem / extensive purpura; faster than above; 80% respond initially, but recurrence common Splenectomy: in adults requiring >20mg pred to keep plt >30 for >6/12; in children if severe ITP after 1yr; curative in 65% Epidemiology: 1:100,000-500,000/yr; F:M 2:1; most common 30-40yrs; mortality <20% Pathophysiology: deficiency of ADAMTS 13 (from liver; cleaves vWF on endothelial cells) plt clumping due to XS vWF activated by ET cell inj Triggered by: pregnancy (may need to differentiate from pre-eclampsia and HELLP); infection (eg. E coli, Shigella), inflammation, drugs (eg. OCP, clopidogrel), Ca, chemo, BM transplant Sx: Fever (rarely >39) Anaemia (haemolytic; Coomb’s negative; severely fragmented RBC; Hb <9 in 25%; reticulocytosis, schistocytes) Renal failure (in 25%) Thrombocytopenia (consumptive; plt <20 in 66%) Neuro Sx (in 75%; altered LOC, FND, seizures) Ix: normal fibrinogen, FDP, coag; decr ADAMTS activity; ADAMTS ab’s in 65% Prognosis: poor; 40% die within 2/52 if untreated; 20% mortality treated; 50% relapse Mng: plt tranfusion may worsen intravascular thrombosis so only used in emergency If life-threatening haem: plt transfusion Prednisone: 1-2mg/kg initial dose Plasma exchange: with FFP replacement (which contains normal ADAMTS); removed vWF and ADAMTS; 90% survival from acute episode FFP: can be used alone Splenectomy Epidemiology: usually children <4yrs; most common preventable cause of renal failure in children Pathophysiology: deposition of fibrin in walls of caps and arterioles due to microV inj (esp in renal) intraV consumption of plt Triggered by: E coli 0157:H7 (Shiga toxin), Shigella, yersinia, campylobacter, salmonella; often occurs 1/52 after gastro / URTI; strep pneumonia + EBV also cause atypical; varicella, echo, caxsackie chemo; Ca; familial (10%; due to factor H def); those not caused by infections are atypical = similar to TTP (no diarrhoea), worse prognosis Sx: Fever Anaemia (haemolytic; fragmented RBC; schistocytes; reticulocytosis; Coomb’s negative; Hb 8) Renal failure (oliguria 5-7/7 post-diarrhoea; severe HTN; nephropathy; incr Cr; 15% develop CRF; electrolyte Imbalance; haematuria, proteinuria, granular/hyaline casts) Thrombocytopenia (consumptive; plt usually <100) Neuro Sx GI Sx (diarrhoea in 90%, often bloody; hepatomegaly) HSP Not plt prob Also: SOB due to pul oedema; weakness; URTI (10%); bleeding rare; purpura; atrial arrhythmia; pericardial effusion Ix: decr haptoglobin; incr LDH; mild incr bil (unconjugated); normal coag; test stool for WBC and Shiga toxin; Mng: careful fluid and electrolyte mng; immunoperfusion; other trt’s not helpful; plt tranfusion given before procedures, but otherwise not helpful; plasma exchange if severe; avoid Abx for E coli as it increases Shiga toxin release; 50% need dialysis; trt HTN Prognosis: good (worse in adults); 60-80% complete recovery; 5-10% mortality; recurrence has 30% mortality rate Epidemiology: 2:1000; more Asian / Indian; usually 4-6yrs (2-11yrs) Cause: Allergic vasculitis, follows URTI, IgA mediated; assoc with infection, drugs, vaccines; may be post Grp A strep Pathology: Small vessels (skin, GIT, kidneys, jts) Sx: Palpable purpura on buttocks and legs (extensor surface) – presenting Sx in 50%; maybe also erythematous, urticarial, echymoses, petechaie AP (+N+V+D; in 60-80%; diffuse and colicky; occurs after rash; 50% have blood in stool; 5% get acute GI haemorrhage; 3% get intussusception) Migratory polyarthralgia (66-80%; presenting Sx in 25%; usually resolves after 24-48hrs; in gravity dependent jts) Renal failure (in 20-50%) – nephritic syndrome Generalized oedema (eg. Feet; often painful) Ix: Haematuria and proteinuria in 90%; urine, FBC (plts normal), U+E Complications: Nephritic / nephrotic syndrome, ARF (<1%), HTN; if proteinuria = more severe and needs FU; Intussusception (5%); bowel perf Other causes of petechiae / purpura Plt function probs Trt: Usually resolves in 3-4/52; supportive; monitor BP and urine for 6/12; IVF if ill; NSAIDS; Consider prednisone 1mg/kg for 2/52 (if abdo, jt or scrotal disease; may prevent renal complications (2% get long term renal impairment); helps jt pain, abdo pain, oedema) Admit if: Abdo, renal complications; symptomatic relief Small vessel disease / decr plt petechiae: decr plts, SBE, vasculititis, meningococcal, measles, steroids, Cushings, PAN, HSP, RMSF Coag probs / trauma non-palpable purpura: vit K def, anticoags, liver disease, haemophilia, vWD, DIC Vasculitis palpable purpura: idiopathic (50%) viral (enterovirus), bacterial (eg. Meningococcus, gonococcal, staph, ricketssia, G-ives) autoimmune (SLE, RA, WG, PAN, IBD), CT disease, HSP Ca, drugs Usually on lower limbs; DD = pyoderma gangrenosum (painful haemorrhagic pustule ulcerate and grow; assoc with IBD, RA, blood dyscrasia, Behcet’s disease, Ca) Vasculitis screen: FBC, ESR, CRP, U+E, LFT, Hep B+C, ANA, ANCA, ASO, cryoglobulin screen, APL ab’s screen, serum protein electrophoresis, C3+4; check urine for RBC’s and casts Other causes of palpable purpura: vasculitis (see below), SBE, cryoglobulinaemia, allergic, embolic Drugs: aspirin, NSAIDs, SKA Diseases: myeloproliferative; CRF; vWD (due to VII-vWF def); paraproteinaemia Notes from: Dunn