(a parita di nerve sparing dichiarata) agile (sulle 4 città che
advertisement

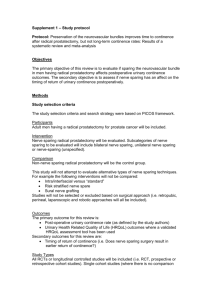
DOES PELVIC LYMPH NODE DISSECTION AFFECT CONTINENCE AND ERECTILE FUNCTION RECOVERY IN PATIENTS UNDERGOING MINI-INVASIVE RADICAL PROSTATECTOMY? A RETROSPECTIVE MULTICENTRE STUDY OBJECTIVES Considering the anatomic proximity of the internal iliac lymph nodes and the pelvic plexus, it may be expected that pelvic nodal dissection is associated with an increased risk of damage to the small pelvis neural and vascular structures. We investigated the impact of pelvic lymph node dissection (PLND) on functional outcomes after robot-assisted and laparoscopic radical prostatectomy (RARP and LRP) PATIENTS AND METHODS We retrospectively analyzed 1928 consecutive patients operated by 35 surgeons in 11 institutions between January 2008 and March 2014; 1029 patients had data for PLND status and 792 had data for both PLND and nerve sparing (NS) status. Patients were stratified in low, intermediate and high risk group (D’Amico classification). Urinary continence (UC) and erectile function (EF) were evaluated pre-operatively and at 1 year post-surgery. We considered only pre-operatively continent and potent patients. Patients who underwent radiotherapy after surgery were excluded. UC was defined as the use of 0-1 pads/day, EF was defined as an International Index of Erectile Function- 5 (IIEF-5) score > 20 RESULTS In our cohort of 1029 patients, 792 patients had available data for PLND and NS status: 183/792 (32,1%) underwent PLND. Patients with monolateral NS, bilateral NS and non NS were respectively: 37/183 (20,2%), 34/183 (18,5%) and 112/183 (61,2%) in the PLND group and 165/609 (27%), 297/609 (48,7%) and 147/609 (24,1%) in no PLND group. Patients from PLND group have 2,5 time higher risk of not doing NS (p < 0,01). PLND patients were14,7 % low risk, 53,5% intermediate risk and 31,8 % high risk. After a year from surgery, 401 patients had data on UC and 312 on EF. There was a significant difference between the two groups in UC: 93/110 (84,5%) patients were continent in PLND group and 276/291 (94,8%) in the no-PLND group (p<0.001). There was a difference, but not statistically significant, between the two groups in sexual function recovery: 1/78 (1,3%) was potent in PLND group and 28/203 (13,8%) in no-PLND group. Considering only the NS patients (mono or bilateral): 85,3% and 96,2% were continent (p=0,01) and 0% and 20% were potent (p=0,06) in no-PLND and PLND group DISCUSSION In this study, PLND was associated with worse continence and potency outcomes at one year after mini-invasive RP. Limits of our study are: it’s retrospective nature, the missing data across covariates, different surgeons with no information on their caseload, variation in surgical technique and extension level of PLND; this limitations make it difficult to generalize the functional outcome to PLND during mini-invasive RP. Patients in the lower D’Amico risk class, have low PLND rates and higher continence and potency recovery rates CONCLUSIONS: In this multicentre retrospective cohort of patients, we reported that PLND during mini-invasive RP reduces continence and sexual function recovery at one year after surgery. Other factors, such as D’Amico risk class and nerve sparing status are involved in the functional outcomes Tabella - Clinicopathologic characteristics stratified by pelvic lymph node disection (PLND) status Characteristic PLND NO PLND Patients, no. (%) Age, yr Mean (SD) PSA preoperative (ng/ml) Mean (SD) Clinical stage, no. (%) T1 T2 T3 D’Amico, no. (%) Low risk Intermediate risk High risk Nerve sparing, no. (%) Mono NS Bilateral NS Non NS 1 year after surgery, no. (%) Continent (0-1security, Pad) Yes No Potent ( IIEF-5 >20) Yes No 265 (25.7) 764 (74.3) P value = 0.145 65.4 (6.4) 64.8 (6.0) 10.33 (9.4) 7.26 (6.8) 117 (44.1) 145 (54.7) 3 (1.2) 502 (65.7) 261 (34.1) 1 (0.2) 39 (14.7) 142 (53.5) 84 (31.8) 486 (63.6) 225 (29.5) 53 (6.9) 37 (20.2) 34 (18.5) 112 (61.3) 165 (27.0) 297 (48.7) 147 (24.3) 93 (84.5) 17 (15.5) 276 (94.8) 15 (5.2) < 0.001 < 0,001 = 0.06 1 (1.3) 78 (98.7) 28 (12.1) 203 (87.9)