WEEK 15: Peripheral vascular system * History
advertisement
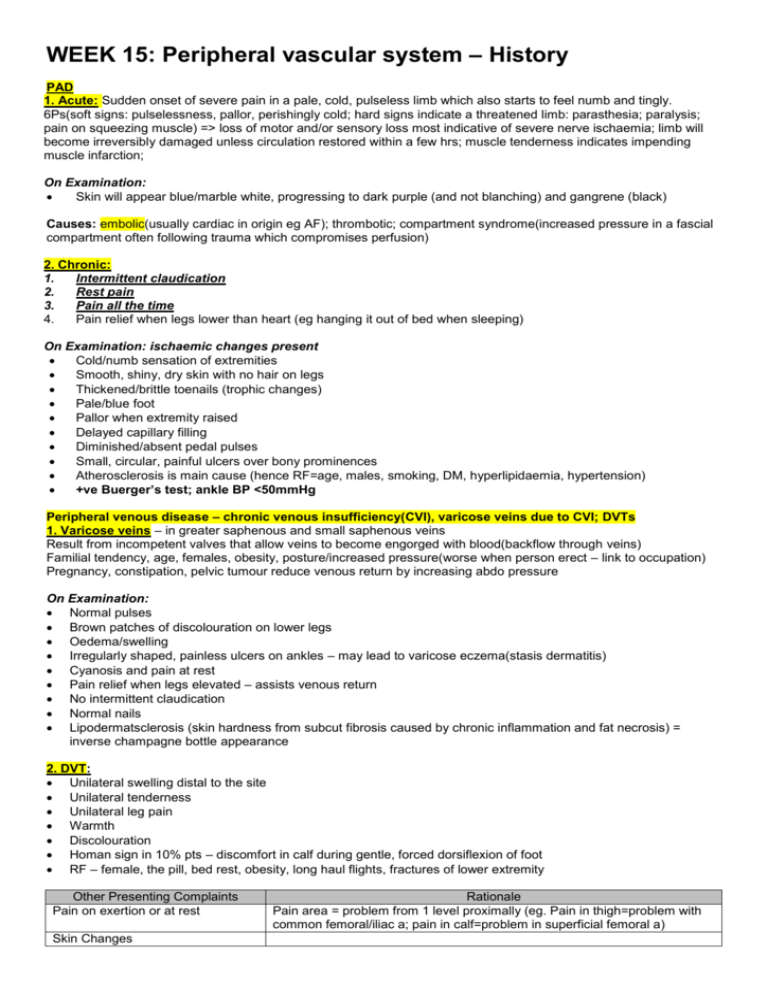
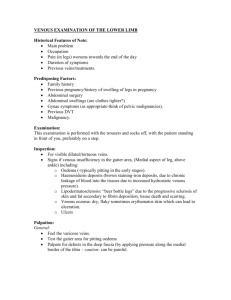
WEEK 15: Peripheral vascular system – History PAD 1. Acute: Sudden onset of severe pain in a pale, cold, pulseless limb which also starts to feel numb and tingly. 6Ps(soft signs: pulselessness, pallor, perishingly cold; hard signs indicate a threatened limb: parasthesia; paralysis; pain on squeezing muscle) => loss of motor and/or sensory loss most indicative of severe nerve ischaemia; limb will become irreversibly damaged unless circulation restored within a few hrs; muscle tenderness indicates impending muscle infarction; On Examination: Skin will appear blue/marble white, progressing to dark purple (and not blanching) and gangrene (black) Causes: embolic(usually cardiac in origin eg AF); thrombotic; compartment syndrome(increased pressure in a fascial compartment often following trauma which compromises perfusion) 2. Chronic: 1. Intermittent claudication 2. Rest pain 3. Pain all the time 4. Pain relief when legs lower than heart (eg hanging it out of bed when sleeping) On Examination: ischaemic changes present Cold/numb sensation of extremities Smooth, shiny, dry skin with no hair on legs Thickened/brittle toenails (trophic changes) Pale/blue foot Pallor when extremity raised Delayed capillary filling Diminished/absent pedal pulses Small, circular, painful ulcers over bony prominences Atherosclerosis is main cause (hence RF=age, males, smoking, DM, hyperlipidaemia, hypertension) +ve Buerger’s test; ankle BP <50mmHg Peripheral venous disease – chronic venous insufficiency(CVI), varicose veins due to CVI; DVTs 1. Varicose veins – in greater saphenous and small saphenous veins Result from incompetent valves that allow veins to become engorged with blood(backflow through veins) Familial tendency, age, females, obesity, posture/increased pressure(worse when person erect – link to occupation) Pregnancy, constipation, pelvic tumour reduce venous return by increasing abdo pressure On Examination: Normal pulses Brown patches of discolouration on lower legs Oedema/swelling Irregularly shaped, painless ulcers on ankles – may lead to varicose eczema(stasis dermatitis) Cyanosis and pain at rest Pain relief when legs elevated – assists venous return No intermittent claudication Normal nails Lipodermatsclerosis (skin hardness from subcut fibrosis caused by chronic inflammation and fat necrosis) = inverse champagne bottle appearance 2. DVT: Unilateral swelling distal to the site Unilateral tenderness Unilateral leg pain Warmth Discolouration Homan sign in 10% pts – discomfort in calf during gentle, forced dorsiflexion of foot RF – female, the pill, bed rest, obesity, long haul flights, fractures of lower extremity Other Presenting Complaints Pain on exertion or at rest Skin Changes Rationale Pain area = problem from 1 level proximally (eg. Pain in thigh=problem with common femoral/iliac a; pain in calf=problem in superficial femoral a) Cold hands and or feet Loss of/ reduced sensation/function Profound ischaemia(embolism) – no chance for collateral circulation to develop; thrombosis is more gradual Swollen ankles, palpitations, SOB HPC: SOCRACTES Past Medical history Any similar problems in the past? Any admissions to hospital? Any recent illnesses? Any chronic conditions? No.of pregnancies? AF JADE, TAB, MARCH, thyroid Drug History Allergy; drug dose/compliance Analgesia Anti-coagulant therapy Statins Anti-hypertensives Peripheral vasodilators GTN spray HRT Insulin Contraceptive pill; pregnancy Thyroxin (T3) Social History Smoking (pack years) Alcohol Occupation Exercise Diet Immobility Overseas / long distance travel Family History PVD Parents alive? Other Rationale Hip fracture – immobility leading to stasis May send emboli off Rationale DO NOT GIVE WARFARIN TO PVD PT WHO HAS HAD A STROKE If pt has AF; but this increases risk of PE Hypercoaguable blood Hypercoaguable blood so increased risk of DVT Rationale Stasis of blood Illness, surgery, varicose veins, immobility of old age Stasis of blood Rationale DM, high cholesterol, hypertension, CVA, MI Ask ‘Have your parents ever suffered a clot in the leg(DVT)/lung(PE)? Inherited – protein C deficiency, protein S deficiency, Factor V Leiden mutation, anti-thrombin III deficiency, etc; Connective tissue diseases – Marfan’s syndrome(AAA) Increased blood viscosity: polycythaemia, myeloma, ? severe dehydration Hypercoaguable blood: Acquired: ‘Systemic’ : collagen diseases, Antiphospholipid syndrome, malignancy, nephrotic syndrome, tissue trauma (including surgery); ‘Local’ : compression / injury to venous system e.g. tumour in the pelvis Check ICE in pts with PVD as often presenting complaint 4 major ways in which PAD pts present: A. Limb symptoms Legs more commonly affected than arms due to more atherosclerosis and a less well developed arterial supply Stage Presenting Rationale complaint I Asymptomatic ABPI <0.8 at rest; asymptomatic because pt is limited by other pathology or they choose not to walk very far Arterial claudication: Most common symptom of PAD; cramp-like pain felt in the legs due II Intermittent claudication to arterial insufficiency after a relatively constant distance and sooner if uphill; pain (sensory loss disappears after a few mins of rest+restarts again on exercise; typical felt in the calf due to in foot – femoropopliteal disease but may be felt in thigh/buttock if aorto-iliac disease. Claudication ‘walking on distance = distance pt can walk before pain starts(often underestimated) Sharp pain, acute onset, pale whole leg, then no pain – most probably due to thrombosis pebbles’); Neurogenic claudication: leg pain due to neurological and musculoskeletal disorders of III Night/rest pain IV Tissue loss (ulcerartion/ gangrene) lumbar spine Venous claudication: leg pain due to venous outflow obstruction following extensive deep vein thrombosis Dull pain, chronic onset, local changes – most probably due to slow ischaemia (though DVT can be quite quick!) Pt goes to bed but is woken up 1-2hrs later with pain in their foot; due to the lost beneficial effects of gravity on lower limb perfusion; sleep also reduced HR, BP and CO. Pt often gets relief by hanging leg out of bed, or sleep in a chair. Ass symptoms: SOB(OE), erectile dysfunction Trivial injuries do not heal allowing bacteria to enter leading to ulcers/gangrene; may lead to amputation/death Chronic or acute arterial changes B. Neurological symptoms Presenting Complaint Carotid artery territory Vertebrobasilar artery territory C. Andominal symptoms Presenting Complaint Visceral ischaemia Abdominal aortic aneurysm(AAA) Rationale Half of TIAs+strokes are due to an embolism from an athermatous plaque at the common carotid bifurcation. Site somatic, speech, visual, Onset sudden, Duration <24hrs, crescendo? Character “like a shutter coming down” blackness, tunnel vision Association + tingling, speech disturbance, facial/limb weakness. See CNS exam and lecture notes for more info. Giddiness; collapse; transient occipital blindness. Subclavian artery stenosis/occlusion proximal to origin of vertebral artery may result in ‘subclavian steal’ syndrome: during arm exercise, blood travels up the carotids, via the Circle of Willis, down the vertebral artery, ‘stealing’ the blood from the posterior cerebral territory, causing stroke-like symptoms. Signs=asymmetry in pulses+BP in arms Rationale Chronic mesenteric ischaemia: 2 of 3 major visceral arteries need to be stenosed before pt develops chronic mesenteric arterial insufficiency as there is a very good blood supply by celiac axis, superior and inferior mesenteric arteries. Severe central abdo pain within 15mins of eating; food avoidance; ?diarrhoea. Acute mesenteric ischaemia: surgical emergency; pt has pain, shock, bloody diarrhoea, profound metabolic acidosis Increased risk if smoke or hypertensive; most pts are asymptomatic until aneurysm ruptures though may present with abdo/back pain(suggests renal colic but a 60yo man with ‘renal colic’ has a AAA until proved otherwise by ultrasound), shock and pulsatile mass; aorta bifurcates at L4/5(belly button): can palpate a AAA here. Acute rupture may present as sudden death in a previously asymptomatic individual. Thoracic aneurysms: usually asymptomatic. Large ones may cause compression symptoms : dysphagia, stridor, compression of the Superior Vena Cava ( SVC ). May result in aortic incompetence; may cause angina due to encroachment on coronary artery orifices. Rupture, with sudden death is a common occurrence. Dissecting aneurysm: most commonly of the ascending aorta, presents with a very severe, tearing sort of pain in the chest, neck, arms and BACK. Pulses may be weak and BP may be low in the right arm. Initially the patient may be suspected of having a heart attack. D. Vasospastic symptoms PC Rationale Raynaud’s Intermittent digital ischaemia induced by cold and emotion; has 3 stages: Pallor: due to digital artery spasm and/or obstruction phenomena Cyanosis: due to deoxygenation of static venous blood (fingers may feel cold, numb, tingling) Redness and painful: due to reactive hyperaemia (with intense tingling in fingers) Acrocyanosis Usually bilateral but may be unilateral; may affect both hands and feet; may be primary (Raynaud’s disease): idiopathic digital artery vasospasm; or secondary(Raynaud’s syndrome): Manifestation of a collagen disease : scleroderma, SLE, Rheumatoid disease, dermatomyositis May be associated with occupational trauma : chain saw operators, pneumatic hammer operators, pianists. Thoracic outlet compression – often unilateral - ? Cervical rib Cold, blue extremities ( not intermittent) worse during the cold weather, usually in young women – cause not known WEEK 16: Peripheral vascular system - Examination Perform an arterial vascular examination Introduction: Intro, confirm pt, explain and gain consent General inspection: Pt well at rest? Around bed: mobility aids, meds, cigs, O2 Pt: age, signs of HF, cyanosis or pallor Unlikely to do be asked to do – ‘please begin at the abdomen’ Hands: Temp, clubbing (liver failure = low vit K), peripheral cyanosis (Raynaud’s), CREST, tar staining, cap refill, tendon xanthoma, radial pulse, brachial pulse, carotid pulse, BP in both arms Radial Allen’s Test: Ulnar Radio-radio delay: coarctation of aorta Brachial Carotid Note that carotid sinus massage provokes decrease in HR so be gentle if pt has had TIA/stroke/stenosis/carotid sinus disease Face: Xanthelasma, corneal arcus, conjunctival pallor, chronic anaemia?, hydration status JVP/prominent veins in neck or chest Axiallary/subclavian vein occlusion Horner’s syndrome Carotid artery dissection or aneurysm Hoarse voice Thoracic aorta aneurysm Abdomen inspection: Obvious pulsations, masses, scars, mottling/ discolouration to abdomen (ruptured AAA) Abdomen palpation: check for pain first Pulsatile mass: is the AA present? Press midline above umbilicus with one hand Expansile mass: if pulsatile mass found, is it expansile? Press deeply with both hands either side Place palmar surface of 4 fingers either side of umbilicus, quite near the flanks and work your way into the umbilicus feeling for an expansile mass. If find one, measure distance between fingers on skin surface. Is it tender too? Leg inspection: compare both legs Dressings Discolourations – blue, brown, red Skin – dry, hair loss, Scars - LSV harvest, groin incision Swelling/ oedema Missing hair, nails (or changes), toes Ulcers/ non-healing injuries around pressure points Muscle wasting Ask pt to wiggle toes (checks for motor dysfunction in acute PAD) Look in between toes and lift up feet 1. Acute PAD: Skin will appear blue/marble white, progressing to dark purple (and not blanching) and gangrene (black) Leg palpation: work distal to proximal, check for pain 2. Chronic PAD: Cold/numb sensation of extremities Smooth, shiny, dry skin with no hair on legs Thickened/brittle toenails (trophic changes) Pale/blue foot Pallor when extremity raised Delayed capillary filling Diminished/absent pedal pulses Small, circular, painful ulcers over bony prominences Atherosclerosis is main cause (hence RF=age, males, smoking, DM, hyperlipidaemia, hypertension) +ve Buerger’s test; ankle BP <50mmHg 1. 2. 3. 4. 5. Temp: compare both legs using back of hands Sensation: ask pt to close their eyes whilst testing Cap refill: hold for 5s and release; refill normal in <2s Pulses: normal/ reduced/ absent: compare one side to the other o Femoral: mid-point of inguinal ligament (ASIS to pubic tubercle) o Popliteal: flex knee; diffuse feeling o Radio-radio and radio-femoral delay Allen Test Identify both radial and ulnar pulses and apply pressure simultaneously in order to occlude the arteries. The patient should clench and unclench the hand until the palm goes pale. Release pressure from the ulnar artery and observe for the distinct pink colouration (reactive hyperaemia) of the palm. If the recolouration of the palm is ≤ 5 seconds, then the circulation to the hand via the ulnar artery is adequate The procedure can then be repeated to check the patency of the radial artery by releasing the radial artery first Auscultation: Femoral bruits Aortic bruits Renal bruits Carotid bruits; if carotid bruits found – think of neurological assessment and fundoscopy To finish: Thanks pt, ask if they have questions, allow them to redress in private, ?further tests and investigations Blood tests: FBC (anaemia); U and E (renal failure); fasting lipid profile; glucose (DM) Buerger’s test: With the patient lying supine, stand at the foot of the bed. Ask about pain. Raise both legs to 45°. Hold for a minute. Ask the patient to sit up and swing the legs over the edge of the bed. o A positive Buergers Test indicates critical limb ischaemia and the following signs will be elicited: o When the legs are elevated there is extreme pallor of the sole of the foot develops along with emptying (or ‘guttering’) of the superficial veins eg dorsal foot veins. Normally the veins will still hold blood and so you can still compress them with your finger. o Within 2-3 minutes of the legs becoming dependent the foot will turn from a bluish colour (as deoxygenated blood refills the veins) to a deep red (‘sunset foot’) due to reactive hyperaemia (from post-hypoxic vasodilation). ABPI: Duplex US: assess whether angioplasty may be of benefit Perform a venous vascular examination: DVT Introduction: Intro, confirm pt, explain and gain consent General inspection: Pt well at rest? Around bed: mobility aids, meds, cigs, O2 Pt: fractures, signs of surgery or injury, pregnancy, Leg inspection: compare both legs Redness Swelling and pitting oedema Varicose veins Ulceration Missing digits Leg palpation: work distal to proximal Temp Tenderness Pitting oedema Pulses (as for arterial) Measure: Using measuring tape, measure mid-calf 10cm below tibial tuberosity comparing both legs at the same point; if >3cm difference, then this is significant for a DVT Auscultation: Lung bases (for any signs of a PE = reduced breath sounds) To finish: Thank pt, cover him up, mention investigations DD: Cellulitis, ruptured Baker’s cyst, lymphoedema, compartment syndrome Investigations: Well’s score: if low, do D-dimer Bloods: FBC, U and E, Clotting Duplex scanning (Doppler and USS) Venogram? Perform a venous vascular examination: varicose veins Introduction: Intro, confirm pt, explain and gain consent General inspection: pt is supine Front of thigh to medial aspect: caused by long saphenous vein Back of knee to lateral malleolus: causes by short saphenous vein Look for: asymmetry, swelling, scars, pigmentation (brown haemosiderin), lipodermatosclerosis, Instructions to pt: Do you have any difficulty standing? Can you please stand for me with your legs uncovered? = makes varicosities more prominent Re-inspect leg Palpation: Gently press on them and watch them refill (confirms they are vascular) Hard veins = thrombosis Painful veins = phlebitis Use back of hand to feel around varicosities, as they are normally warm Special Tests: Trendelenburg’s test (SFJ is located 2cm inferior and 2cm medial to femoral pulse) This tests for level of incompetence in veins 1. Ask patient to sit on edge of examination couch. Check for pain 2. Elevate the limb as far as is comfortable for the patient and empty the superficial veins by ‘milking’ the leg. 3. With the leg still elevated exert digital pressure (or apply a tourniquet) over the saphenofemoral junction. (2-3cm below and 2-3cm lateral to the pubic tubercle) 4. Ask the patient to stand 5. if varicosities refill then the incompetent vein is lower eg in the presence of saphenofemoral junction incompetence the varicose veins will not refill until the digital pressure (or tourniquet) is removed. Special Tests: Morrisey’s/ Cough test Ask pt to stand Place fingers over SFJ and ask them to cough If a thrill is felt, it suggests incompetence Pratt’s Test: Occlude SFJ, bandage legs, slowly unravel and look for level of incompetent perforators Tap (Schwartz’) Test: pt stands, one hand on SFJ, one hand on varicosities, tap SFJ and feel for thrill in other hand. If thrill present – backflow between SFJ and varicosities Special Tests: Doppler US probe test: Place a Doppler at the SFJ Squeeze the calf Normal leg produces a single Doppler ‘whoosh’ as blood goes back to the heart A leg with incompetent veins will give a second ‘whoosh’ as you stop squeezing when blood flows backwards ino the veins Can repeat at the saphenopopliteal junction To finish: Thank pt, cover them up, mention any investigations, check peripheral pulses, PR exam (ovarian tumour), history Combined venous vascular examination: Introduction: Intro, confirm pt, explain and gain consent General inspection: pt is supine Pt well at rest? Around bed: mobility aids, meds, cigs, O2 Pt: fractures, signs of surgery or injury, pregnancy, Front of thigh to medial aspect: caused by long saphenous vein Back of knee to lateral malleolus: causes by short saphenous vein Look for: asymmetry, swelling, scars, pigmentation (brown haemosiderin), lipodermatosclerosis, Unlikely to do be asked to do – ‘please begin at the legs’ Hands: Temp, clubbing (liver failure = low vit K), peripheral cyanosis (Raynaud’s), CREST, tar staining, cap refill, tendon xanthoma, radial pulse, brachial pulse, carotid pulse, BP in both arms Radial Allen’s Test: Ulnar Radio-radio delay: coarctation of aorta Face: Xanthelasma, corneal arcus, conjunctival pallor, chronic anaemia?, hydration status JVP/prominent veins in neck or chest Axiallary/subclavian vein occlusion Horner’s syndrome Carotid artery dissection or aneurysm Hoarse voice Thoracic aorta aneurysm Leg inspection: compare both legs Dressings Discolourations – blue, brown, red Skin – lipodermatosclerosis, Scars - LSV harvest, groin incision Swelling/ oedema Nails changes or missing toes Varicosities Ulcers Muscle wasting Look in between toes and lift up feet 1. Varicose veins: Normal pulses Brown patches of discolouration on lower legs Oedema/swelling Irregularly shaped, painless ulcers on ankles – may lead to varicose eczema(stasis dermatitis) Cyanosis and pain at rest Pain relief when legs elevated – assists venous return No intermittent claudication Normal nails Warm Lipodermatosclerosis (skin hardness from subcut fibrosis caused by chronic inflammation and fat necrosis) = inverse champagne bottle appearance 2. DVT: Unilateral swelling distal to the site Unilateral tenderness Unilateral leg pain Warmth Discolouration – red Homan sign in 10% pts – discomfort in calf during gentle, forced dorsiflexion of foot RF – female, the pill, bed rest, obesity, long haul flights, fractures of lower extremity Instructions to pt: Do you have any difficulty standing? Can you please stand for me with your legs uncovered? = makes varicosities more prominent Re-inspect leg Palpation: Gently press on them and watch them refill (confirms they are vascular) Hard veins = thrombosis Painful veins = phlebitis Use back of hand to feel around varicosities, as they are normally warm Temp Tenderness Pitting oedema Pulses (as for arterial) Measure: Using measuring tape, measure mid-calf 10cm below tibial tuberosity comparing both legs at the same point; if >3cm difference, then this is significant for a DVT Auscultation: Lung bases (for any signs of a PE = reduced breath sounds) Special Tests: Trendelenburg’s test (SFJ is located 2cm inferior and 2cm medial to femoral pulse) This tests for level of incompetence in veins 6. Ask patient to sit on edge of examination couch. Check for pain 7. Elevate the limb as far as is comfortable for the patient and empty the superficial veins by ‘milking’ the leg. 8. With the leg still elevated exert digital pressure (or apply a tourniquet) over the saphenofemoral junction. (2-3cm below and 2-3cm lateral to the pubic tubercle) 9. Ask the patient to stand 10. if varicosities refill then the incompetent vein is lower eg in the presence of saphenofemoral junction incompetence the varicose veins will not refill until the digital pressure (or tourniquet) is removed. Special Tests: Morrisey’s/ Cough test Ask pt to stand Place fingers over SFJ and ask them to cough If a thrill is felt, it suggests incompetence Pratt’s Test: Occlude SFJ, bandage legs, slowly unravel and look for level of incompetent perforators Tap (Schwartz’) Test: pt stands, one hand on SFJ, one hand on varicosities, tap SFJ and feel for thrill in other hand. If thrill present – backflow between SFJ and varicosities Special Tests: Doppler US probe test: Place a Doppler at the SFJ Squeeze the calf Normal leg produces a single Doppler ‘whoosh’ as blood goes back to the heart A leg with incompetent veins will give a second ‘whoosh’ as you stop squeezing when blood flows backwards ino the veins Can repeat at the saphenopopliteal junction To finish: Thank pt, cover them up, mention any investigations, check peripheral pulses, PR exam (ovarian tumour), history 1. Ankle: Brachial Pressure Index (ABPI): to exclude PAD ABPI is measured using a hand-held Doppler and a sphygmomanometer. 1. The patient must be rested in the supine position or ankles raised to the same height as the heart. 2. The systolic pressure is measured in the dorsalis pedis and posterior tibial arteries of the same leg by holding the Doppler probe over the pedal artery while a blood pressure cuff wrapped around the ankle is inflated. 3. The pressure at which the Doppler signal disappears gives the systolic pressure in that artery (or re-appears when pressure released THINK! Just like taking a BP and Korotkoff sounds appear). 4. The blood pressure should be taken in both arms and the ABPI is calculated as follows: ABPI = Highest ankle systolic pressure Highest brachial systolic pressure sBP(leg) sBP(arm) A value for ABPI can be obtained for each leg. Normally the systolic BP in legs ≥ arms so a normal ABPI should be ≥1 in the supine position. ABPI is a sensitive marker of arterial insufficiency. Typical values of ABPI are: >1.3 = Calcification due to DM or atherosclerosis 0.9-1.3 = Normal 0.8 = 20% mortality in 10 years 0.6-0.9 = Mild-mod claudication 0.4 = 80% mortality in 10 years 0.3-0.6 = Severe claduication <0.3 = Critical ischaemia and renal problems N.B. In diabetics the systolic BP in the lower limbs is sometimes not measurable as the arteries are calcified and difficult to compress leading to a falsely raised ankle pressure (possibly giving false normal result). Pole test can be used in this case – foot is raised slowly whilst auscultating pedal pulses and systolic BP value is read from a specially calibrated pole at the level where pulse disappears. 2. Handheld Doppler US – investigate bypass grafts Uses the Doppler effect. Triphasic flow = normal artery; monophasic = past a stenotic area Triphasic: o Phase one - During systole, blood flow accelerates in a forward direction within the blood vessel. o Phase two - A drop in peak systolic pressure leads to a reverse flow of blood within the blood vessel. o Phase Three - Elastic recoil of the vessel at the end of diastole leads to a further forward flow of blood in the vessel. Biphasic: o Vessels naturally lose their elasticity as part of the ageing process, making the signal biphasic. Monophasic: o Monophasic signal produces only one sound and usually denotes vessel disease. The sound heard is usually lower in pitch. 3. MRA – investigate deep arteries of leg Take image before and after contrast agent and build up an arterial map of body 4. CT scan – exclude AAA Can give dye – arteries appear white 5. Catheter angiography Small tube into artery with wire in which you can inject X-ray contrast down it; have to do so over a bony prominence do can put pressure over it for 10mins after to stop bleeding; then do digital subtraction where –ve and +ve images subtracted from each other showing only the images of the lumen of the vessel Examining a patient with Peripheral Vascular Disease Case to illustrate: Presenting complaint: Students: past medical history PAINFUL LIMBS (ischaemic limb) Pamela Valerie Davies, a 56-year-old lady who is overweight, presents to her GP with a painful, cold right leg. How do you approach this? You should concentrate on the history of the presenting complaint: painful cold limb. Associated features. The characteristics are: - the pain started 3 months ago and has been getting worse - the calf feels tight and painful whilst walking and was relieved entirely by resting for approximately 10mins - Previously, it would return when she walked again, after about 200m - However, today the leg suddenly became very painful and cold. nothing makes it better. - she has had no previous pain in either limb WHAT OTHER FEATURES IN THE HISTORY SHOULD YOU ASK ABOUT? - hypertension; non-insulin dependent diabetes mellitus family history - mother & father died from heart disease, both in their 60s; younger brother, in his 50s, has angina drug history - atenolol, glibenclamide allergies - none known review of systems - CVS: no specific features RS: no specific features GIT: no specific features GU: no specific features CNS: no specific features Locomotor: no specific features social history Comment: - housewife, limited mobility due to obesity - alcohol: none - smoking: 15 cigarettes per day This patient has presented with an intermittent claudication. She has a number of predisposing factors for limb ischaemia, eg hypertension, diabetes mellitus, family history and smoking. The discussion with the students should include risk factors and the preventative measures that can be taken. Features on examination of this patient which could be discussed and which would be evident if you examined such a patient on the ward after admission include: - cold, pale foot - the presence or absence of pulses - the use of the Doppler probe Specific examination features for students to practise: examination of peripheral pulses changes due to poor arterial flow examination of venous system examination with a Doppler probe PULSES AND BRUITS Clinical Features of Venous and Arterial Ulceration PMH Cause Location Base Edge Arterial Smoker, ID, PVD, DM Venous Varicose veins, DVT Arterial ischaemia Distal foot, tips of toes, heels, bony prominences Dry, necrotic, gangrenous base with little/no evidence of healing Punched out Venous hypertension ‘Gaiter area’ = maleoli and lower calf, predominantly medial malleolus Active evidence of chronic granulation, bleeds, Sensation Skin Painful Pale, poorly diffused, previous amputations CRT Prolonged Shallow or sloping irregular healing edge Normal Haemosiderrin, lipodermatosclerosis, shiny/tight Normal with Friable base that may extend deeply into the tissues and expose tendons or bones Punched out Marjolin’s Long standing ulceration Malignant change Anywhere at site of previous ulcer, usually venous Irregular areas of cellulitis or wet gangrene appearance Irregular Insensitive Callous formation Satellite lesions Normal Normal Neuropathic DM, peripheral neuropathy, burning pain Loss of sensation Pressure areas, base of feet, 4th and 5th MTPJ