Acute Change of Condition Reporting Guide
advertisement
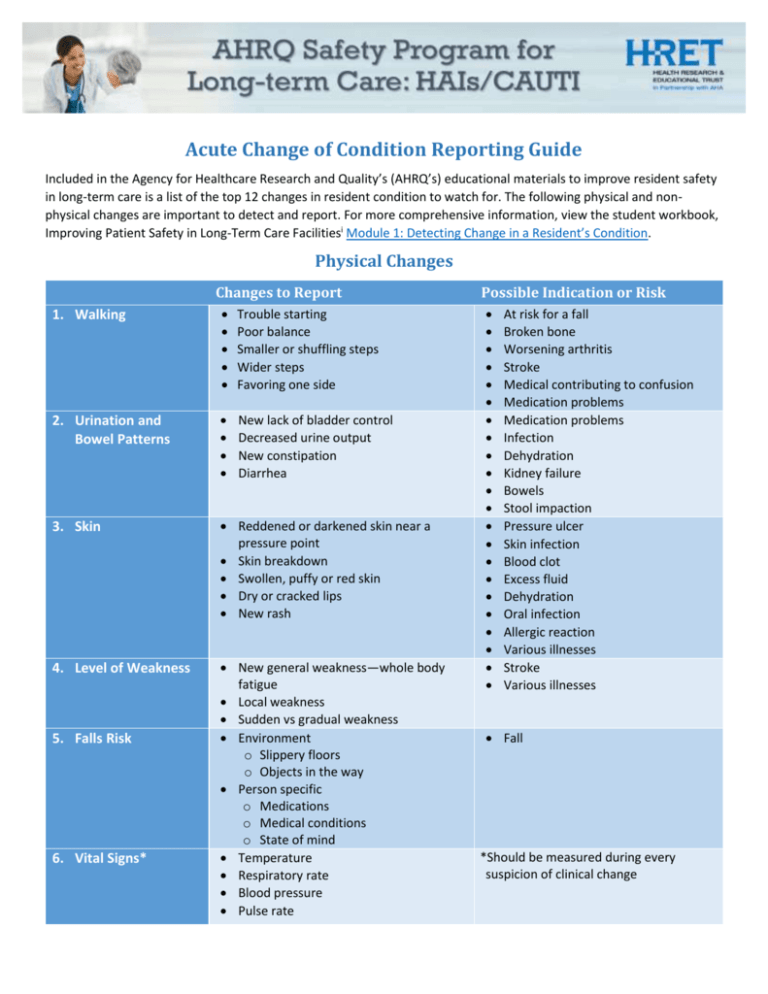
Acute Change of Condition Reporting Guide Included in the Agency for Healthcare Research and Quality’s (AHRQ’s) educational materials to improve resident safety in long-term care is a list of the top 12 changes in resident condition to watch for. The following physical and nonphysical changes are important to detect and report. For more comprehensive information, view the student workbook, Improving Patient Safety in Long-Term Care Facilitiesi Module 1: Detecting Change in a Resident’s Condition. Physical Changes Changes to Report 1. Walking Trouble starting Poor balance Smaller or shuffling steps Wider steps Favoring one side 2. Urination and Bowel Patterns New lack of bladder control Decreased urine output New constipation Diarrhea 3. Skin Reddened or darkened skin near a pressure point Skin breakdown Swollen, puffy or red skin Dry or cracked lips New rash 4. Level of Weakness New general weakness—whole body fatigue Local weakness Sudden vs gradual weakness Environment o Slippery floors o Objects in the way Person specific o Medications o Medical conditions o State of mind Temperature Respiratory rate Blood pressure Pulse rate 5. Falls Risk 6. Vital Signs* Possible Indication or Risk At risk for a fall Broken bone Worsening arthritis Stroke Medical contributing to confusion Medication problems Medication problems Infection Dehydration Kidney failure Bowels Stool impaction Pressure ulcer Skin infection Blood clot Excess fluid Dehydration Oral infection Allergic reaction Various illnesses Stroke Various illnesses Fall *Should be measured during every suspicion of clinical change Acute Change of Condition Reporting Guide Non-Physical Changes Changes to Report 7. Demeanor (i.e., appearance or way of acting) 8. Appetite Changes from baseline o Withdrawal o Passivity o Not wanting to socialize o Talkative o Inattentive Loss of appetite Increased hunger Change in food preferences Pain from eating 9. Sleeping Not feeling rested Unable to fall asleep Difficult to rouse from sleep Difficulty breathing 10. Speech New slurred speech New garbled speech Speaking loudly Difficult finding the right words New levels of confusion or delirium Talking more or less than normal Not making sense Refusing or resisting care 11. Confusion or Agitation Note: Many residents may have some confusion at baseline. 12. Resident Complaints of Pain New or worsening chronic pain Acute pain Possible Indication or Risk Bloodstream infection Stroke Depression Medication problems Infection Chronic congestion Stomach problems Dental problems Depression Dementia Delirium Pain Anxiety Depression Lung problems Medication Stroke Sleep deprived Pain Medication Pneumonia Urosepsis Dehydration Stroke Arthritis Heart attack Major blood vessel weakening Weakening of the bowel wall i Improving Patient Safety in Long-Term Care Facilities. July 2012. Agency for Healthcare Research and Quality, Rockville, MD. http://www.ahrq.gov/professionals/systems/long-term-care/resources/facilities/ptsafety/index.html. 2