Med Chart – Final
advertisement

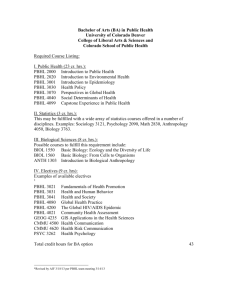
Medica/tion Chart Medications in the Anesthesia Cart Drug: Mech of action & Receptor: Onset: Duration of action: Normal Dose: Uses: Risks: Other: Alupent Stimulates ß2 receptors, resulting in relaxation of bronchial smooth muscle. Inhalation: 1 min. Inhalation: 3-6 hrs. MDI: Bronchodilator to Tx: - bronchospasm r/t asthma, chronic bronchitis, emphysema HTN, hypoTN Tachy, palpitations Hypo-K ↑ BP followed by a substantial ↓ in BP. Severe paradoxical bronchoconstriction. Drowsiness, cough N/V, tremor, HA nervousness, vertigo Insomnia Caution: isch. Heart, Facilitate tracheal intubation, Improve surgical working conditions during general anesthesia (produces skeletal muscle relaxation), used to facilitate mechanical ventilation in critically ill. HypoTN, vasodilation ST, SB Hypovent./apnea Broncho/larynospasm Dyspnea, urticaria Histamine SE rare at recommended doses. Prolonged infus. ↑ seizure risk. Caution: hx of asthma & anaphylax. Interactions: NM block ↑ w/: animogl. abx, LA, Mg, lithium, ganglionic blockers, hypothermia, hypo-K, resp acidosis, Succs, Volatile, loops, MG, adrenocort. dysf. Req ↓ & w/: Volatiles Recurrent paralysis w/ quinidine. Reversal effects ↓ w/: theophylline, paresis, anticonvul. Rx, burn pt. Category C Contra: obstruct. Uropathy/GI, NA glaucoma. Caution: additive effects w/ other Rx, Pts w/ tachy arrhyth, CHF, AMI, fever, GERD, GI infect. Antagonizes: Reglan & Antichol-ase Rxs. (metaproterenol sulfate) * Sympathomimetic Selective ß2adrenergic receptor agonist Atracurium Besylate Competes for cholinergic receptors at the motor end plate. Nicotinic receptors (Tracrium) * Non-depolarizing NMBA Atropine Sulfate Nebulizer: Inhal x 5-15 of 5% soln. (0.3ml/dose) Kids: Rx not recommended IV: <3 min. hydrolysis & Hoffman elim. - Temp & pH dep. IV: 45-60 sec ETT:10-20 sec IM: 5-40 min. Inhal: 3-5 min Calcium Chloride 3x ↑ Ca vs Ca gluc. *electrolyte & + inotrope Nerve and muscle fxn/contraction, cell memb. & cap. perm., renal fxn, resp., coagulation. Ca channel receptors. Intubation: Elim: Ester Anticholinesterase Rx w/ Atropine or Glycopyr. *Anticholinergic IV: 20-35 min. IV: 0.3-0.5mg/kg (add’l doses at 10-50% of intub. dose).monitor: w/ nerve stimulator to min. OD. Reversal: Competitively antagonizes Ach at Muscarinic receptor. Inhal. x 2-3 q 3-4 hrs. PRN (0.65mg/spray) **MAX:12 inhalations/24 hrs IV: <30 sec. Active Metabolite: Laudanosine can cause CNS stim. (give 10X the normal dose) IV/IM: antichol 1-2 hr antisialog 4hr. ACLS & Brady: Inhalation: antichol 3-6 hrs. IV/IM 0.4-1 mg IV/IM/SC 0.5-1mg, q 3-5 min x 3 Kids: 10-20 mcg/kg Pre-Op: Bronchodilation: Brady, ACLS, pre-med to ↓ secretion, NMBA reversal /emergence, bronchospasm. Cholinergic crisis. OP poisoning. Inhal 0.025 mg/kg q 4-6 hrs. (2.5 mg max) Emergence: Elim: Hepatic IV 0.015 mg/kg with… Edroph: 10mcg/kg Neo: 0.05-1 mg/kg & Renal IV: 10-20 min. Adult: IV 500-1000 mg Kids: Elim: GI & Renal IV 10-25 mg/kg Goal serum Ca: **8.5-10mg/dL Resp. dep., CNS effects, dry mouth. ↓ GI motility & LES tone,GERD(↑ asp risk) UO retention. High doses: tachy, anhydrosis Low doses: Brady Toxicity: tx w/ Benzo & physostigmine. HTN, arrhyth., ↑ thyroid, DM, Seizures, RF, liver dx Contra:pt w dysrhyth hypersensitivity, tachy r/t dig tox. Interactions: other Sympaths., MAOI’s, BB. Category C Crosses BBB Category C ACLS, hyper-K (w/ EKG changes), hyperMg, Lg. vol. Transf. (citrate), Ca antagonist OD. HTN, hypoTN, brady, Arrest, N/V, lethargy, hyper-Ca (weak, HA, fatigue, confusion, irregular HR). Arrhyth. w/ rapid IVP Antagonizes: CCB, Verapamil, Mg. ↑ Arrhyth: dig tox. Category C Dexamethasone (Decadron) * Synthetic Glucocorticoid ↓ inflammation by inhibiting the migration of leukocytes and reversal of increased capillary permeability. Suppresses normal immune response. IV/IM: Antiinflam. 2-5 min. IV/IM: Anti-inflam. 36-54 hours Anti-inflammatory: IV/IM 0.5-25mg/day ↑ ICP/Cerebral edema: IV 10-50mg initially → IV/IM 420mg q 6 hrs x 5-7 days. Airway Edema: Elim: IV 10-25mg q 6 hrs x 5 PRN (at least 24hrs prior to intub.) Inflamm. diseases ↑ ICP/cerebral edema, Aspir. pneumo. Bronchial asthma Prevent transplant rej. Replace. therapy w/ adrenalcortical insuff. Bronchospasm: Inhal 300mcg (3) 3-4 x day Glucocorticoid receptors 0.75mg Dex. = 20mg Cortisol Digoxin (Digitalis) (Lanoxin) *Cardiac Glycoside Diphenhydramine (Benadryl) Directly inotropic effect d/t inhibitor of the Na-K ATPase pump. Indirect vagomimetic effect ↓ conduction through the SA node & prolongs conduction at AV node. IV: 5-30 min. Antagonizes histamine H1 receptors. IV: 3-5 min. H1 receptors PO: 0.5-2 hrs. (Inapsine) * Neuroleptic - Butrophenone Edrophonium Chloride (Enlon) (Tensilon) (Reversol) Adults: CHF, SVT + inotrope - chronotrope Creat Cl. 10-79 & >65 y/o: ↑ contractility ↓ myocardial O2 consumption IV/PO 0.5-1mg divided: 50% → remaining in 25% x 4, then→ IV/PO 0.125-0.5mg/daily ↓ daily dose: IV/PO <0.25mg Monitoring: K & Dig levels Elim: Renal (must be 4-6 hr post dose; therep. takes up to 7 days) IV/PO: 4-6 hrs IV/IM 10-50mg **MAX: 400mg/day PO: <15 min. PO 25-50mg q 6-8 hrs Elim: Hepatic * Antihistamine Droperidol IV/PO: 3-4 days Antagonizes dopamine, NE, & serotonin at the NT synapses, incl. the CTZ. Producing tranquilization, antiemetic effects. IV/IM: 3-10 min. IV/IM: 2-4 hours IV/IM 2.5-10mg Antiemetic: IV 0.625-2.5 mg Neuroleptanesthesia: Elim: Hepatic & Renal Dopamine, NE, & Serotonin receptors Inhibits hydrolysis Ach by competitively binding to acetylcholinesterase. improves intestinal/ skeletal muscle tone, increases secretions, Pre-Op: Antiemetic, antivertigo, allergic rxn., EPS rxn (symptomatic), antichol Partially inhib. vasodil effects of histamine. Anaphylaxis after Epi. Anesth. pre-med - N/V Neuroleptic ↓ potentiation and SE of Opioid epidural. IV 0.2mg/kg with… Fentanyl 4mcg/kg Epidural: 1.25-2.5mg IV: 30-60 sec IV: 5-20 min. Emergence: Slow IVP 0.5-1mg/kg **MAX: 40mg with…. Atropine 0.015mg/kg Glycopyrrolate 0.01mg/kg PSVT: Slow IVP 2mg q 1-2 min. Reverse ND NMBA Dx of MG (↑ strength) DX & Tx PSVT - including WPW Short acting Arrhyth, HTN CHF (susceptible pts) Seizure, ↑ICP, psychosis ↑ Insulin req. ↓ wound healing Petechiae, erythema. ↑ IOP H2O/Na retention K depletion Myopathy, weakness Thromboembolism ↑ risk of infection (↑ masking of S&S) Avoid NSAIS’s Enhance ß-agonists Alters Counadin resp Caution: pt w/ HTN, CHF, emboli hx, MG, ↓ thyroid, cirrhosis, peptic ulcer, UC, diverticulitis, new GI anastomosis, psychosis, seizures, syst. fungal/viral inf. Contra: admin of live viral vaccines. Long-term: muscle wasting, spont. fx. Narrow therp. range CHB, arrhyth. (VT, VF, ect.) HA, psychosis, confs. N/V/D, gynecomastia Toxicity S&S: N/V, arrhyth., HA, ↑or↓ K (or normal), drowsy, Yellow-green haols. Category C HypoTN, palp., PVC. Wheezing, tightness. Paradox. CNS stimul. (more in kids) Sedation, conf., blur. vision, tinnitus, tremors, seizures. Urine frequency or retention. HypoTN, ↓SVR, Tachy (↓ upstroke), prolonged QT. Prolonged CNS dep. w/ neuroleptanesth. EPS, drowsiness, hyperactivity. “Fear of death” w/ preop admin. Caution: Sedative Brady, tachy, AV block, hypoTN ↑ secretions, resp ditress, bronchosp. Anaphyl, allergic rxn Seizures, dysarthria HA, miosis NO effect on depol NMBA (Succs) Interactions: effects ↓ with amino abx, steroids, Mg, hypo-K, hypothermia, resp & metabolic acidosis. Interactions: Toxicity ↑ w/ ↓ K, ↓ Mg, ↑ Ca, ↑ serum CCB levels, enzyme inhibitors. ↑ thyroid ↑ resistance ↑ arrhyth w/ Succs Contra: VF, cardioversion w/ dig toxicity. effects are additive, MAOI’s potentiate antichol. effects, NA glaucoma, ↑ IOP, seizures, GI or bladder neck obst. lower resp dx (incl. asthma). R/o hypoTN enduced N/V before admin. Contra: Parkinson’s Caution: potentiates other CNS dep. Rx, ↓ effects of Epi, ↑ threshold for Haloth. & Epi-induced arrhyth. Category C * Anticholinesterase salivation. Binds to acetylcholinesterase. Elim: Hepatic & Renal Tx Chol. Crisis: Ephedrine *Non-Catecholamine Sympathomimetic Epinephrine (Adrenaline) *Sympathommetic (Catecholamine) Atropine: IV 10mcg/kg q 3-10 min PRN Mixed direct & indirect stimul. of the ɑ- & ß-adrenergic receptors by ↑ the activity of NE at post-synaptic α- and βreceptors. Alpha and Beta adrenergic receptors A1 ↑ vasoconstriction A2 relax smooth muscle B1 ↑ bronchodilation B2 ↑ myocardial contract. And HR Agonist: alpha 1, alpha 2, beta 1, beta 2. (response dose dep.) IV: immed. IM: 2-5 min. IV: 30-60 sec SC: 6-15 min ETT: 5-15 sec Inhal: 3-5 min Esmolol (Brevibloc) * Beta Blocker Cardioselective Selectively antagonizes Beta1 receptors prod. negative inotropic & chronotropic effects: ↓ sinus HR, ↓ CO, ↓ BP. IV: 1-2 min. IV/IM: 10-60 min. Elim: Hepatic & Renal Resistant to: MAO & COMT IV: 5-10 min ETT: 15-25 min. Inhal/SC: 1-3 hrs. MAX: 10mg w/ Atropine avail (1mg/kg if > 90% twitch depression when reversal is intiated). Hypotension/ Bronchospasm: IV 5-25 mg IM/SC 25-50mg q 5-10 min PO 25-50mg q 3-4 hr PRN (PO for bronchospasm only) Vasopressor Bronchodilator ↑ CO, BP, HR, coronary BF, skeletal BF **MAX: 150mg/24 hrs ACLS: IVP 1mg q 3-5 min x2 (1:10,000 soln) Intra-Op: Infusion 2-20mcg/min. Anaphylaxis: ACLS, anaphylaxis, prolong LA Post-intubation & infectious Croup. IM/SC 0.1-0.5mg (1:1,000 soln.) Bronchodilation: Elim: MAO & Neb w/ O2: Dilute 1ml 2.25% racemic Epi OR 1% (1:100) Epi w/ 3ml NS, give 1-3 inhal q 5 min. COMT IV: 10-20 min. Induction: IV 500mcg/kg/1 min. → infus. 50-200mcg/kg/min (titrate) Elim: HTN, tachy, arrhyth. Pulm. edema Anxiety, tremors Insomnia (CNS stim.) Trans. hyper-K then results in hypo-K. Unpredictable effects: pt w/ depl. endrog NE Volatiles: co-admin ↑ arrhyth, ↑ MAC Potentiated: w/ TCA Caution: pt w/ HTN, ischemic heart dx. HTN, tachy, angina, arrhyth., pulm edema. hypo-K, & transient hyper-K. Anxiety, HA Cerebral hemorrhage. ↓ renal BF, ↓ UO. Caution: ↑ effects of SVT, peri/intra-op HTN Attenuate pressor response d/t intubation. IVP 25-100mg q 5 min. PRN Infus. 50-300mcg/kg/min. HypoTN, brady Confusion, N/V Urinary retention ↑ Dig. levels Mask ↓ BG IV site rxn. High-dose: Antag. B2 - Bronchospasm - ↓ BG Esterases Reversal: Pacemaker Etomidate (Amidate) Atropine IV 1-2mg Isoproterenol IV 0.02-0.15mcg/kg/min Glucagon IV 1-5mg Enhances the effects of GABA similar to barbs, propofol, and benzo’s. GABA receptor agonist Category C - Min alt. uterine BF TCA’s, ↑ arrhyth w/ volatiles & dig tox. Pt’s w/ HTN, CVD, DM, hyperthyroid. Contra: LA or reg. in Category C HTN: Beta1-adrenergic receptors Caution: brady, asthma, arrhyth., peptic ulcers. Contra: peritonitis, GI or urinary obst. Category C digits, nose, ect.. IV 25-100mg 2 min prior SVT: N/V/G, ↑ peristalsis Urticaria, rash OD: cholinergic crisis ↑ levels w/ co-admin: morphine, warfarin. Potentiates: myocar. dep. w/ inhal. or IV anesth.; NMB of Succs & Panc. Caution: AV-HB, nontachy HF, COPD Incompatable: Bicarb Category C IV: 30-60 sec IV: 3-10 min. Elim: Hepatic Induction: IV 0.1-0.4 mg/kg Infus 0.25-1mg/min. Induction Anesth. supplement - alt. to propofol/ Barbs esp. w/ CV instability. HypoTN, HTN Arrhyth., N/V Hypovent., hypervent Laryngospasm hiccup, eye/muscle movements. Adrenocortical supp. Thrombophlebitis Rapid IVP: ven.pain & myoclonus.↓w/ benzo/opioid pre-med Interactions: CV & CNS dep. ↑ w/ Narcs, sedatives, & volatiles Caution: pt w/ focal epilepsy Category C (Sublimaze) Activates Mu1 & Mu2 opioid receptors. *Opioid Reversal: Naloxone Fentanyl Flumazenil (Romazicon) *Benzo antagonist IV: 30 sec IM: <8 min. IV/IM/SC: 0.2-0.4 mg Antagonizes the effect of benzos at the GABA receptor. IV: 30-60 min. Pre-Op & Analgesia: IM: 1-2 hrs. IM/IV 25-100 mcg Induction: IVP 5-40 mcg/kg Elim: Hepatic & Pulm. IV/ETT: 1-2 min. GABA receptor antagonist. IV/ETT: 45-90 min. Elim: Hepatic **Reversal Rx** Inhibits reabsorp. of Na, Cl & K at the ascending medullary. * Loop Diuretic Na-K-2Cl cotransporter Ascending loop of Henle Glycopyrrolate (Robinul) * Anticholinergic Intra-Op: Inhibits action of ACh at post-ganglionic PNS receptors in smooth muscle, secretory glands, CNS. IV: 5-15 min. IV: 2 hrs PO: 6-8 hrs Reversal/OD: IV 0.2-1 mg at a rate of 0.2 mg/min. q 20 min PRN **MAX: 3mg/hr Kids: 0.01mg/kg, PRN 45 sec → 6sec.x 4. **MAX: 1mg Reversal of sedative effects of Benzo’s. - reverse NMBA first. IM/PO: 15-30 min. Muscarinic receptors IV: Vagal block 23hr ↓ secretions 7 hrs PO: Vagal block 8-12hrs. **Reversal Rx** Caution: MAOI’s N/V, confusion, HA, agitation, seizures. Arrhyth., tachy, brady, angina, HTN, flushing. Caution: Resedation Benzo OD: other Rx SE may emerge. Esp TCA’s Other: Diuresis: Slow IV/IM 5-40 mg PO 20-160mg/day Infusion 4mg/min or ↓ Kids: slow IV/IM 0.1-1mg/kg PO 1-2mg/kg daily Elim: Renal IV: <1 min. Resp. dep.(dose dep), Rigidity(high dose), Brady, HypoTN Urinary retention N/V Category C - Crosses placenta IV 2-20 mcg/kg ETT 1 mg/10ml NS (adult) (Lasix) Furosemide Analgesia, pre-med., anesthesia. Pre-med: IV/IM 0.1-0.2mg PO 1-2mg (dilute in 3-5ml of apple juice or soda). Emergence: IV 0.01mg/kg with… Neo IV 0.05mg/kg Pyridostigmine IV 0.25mg/kg (0.2 mg Glyco. per 1mg Neo, or 5mg of Pyridostigmine) Diuretic, HTN, ↑ ICP CHF edema, Hepatic cirrhosis Nephrotic syndrome CRF pts. Diuretic resistant pts ↓ prod. of CSF Dx acute oliguria Ortho-hypoTN Hypo-K, ↑ BG, ↑ uric Hypo-Cl alkalosis Ototox. (rapid IVP) Tinnitus, vertigo N/V/D ↓ clearance of: salicylates & lithium. Phototox. (1-2 weeks post exposure) Bladder spasm Pancreatitis TCP, neutropenia, aplastic anemia. Pre-med (vagolysis) - ↓ secretions, relax bronch., ↓ GI tone/motility, ↓ LES tone, ↑ IOP. Reversal of NMBA Adjunct w/ peptic ulcer, & bronchospasm. Tachy, brady, palp. Confusion esp elderly Dizzy, HA, dry mouth Urinary hesit/retent. N/V, urticaria, ↑ IOP Poor PO absorption vs. Atropine: ↓ tachy & ↓ secretions. may occur (up to 2 hrs. after reversal). More potent Benzo’s req ↑ dose Category C Diuretic of choice w/ acute CHF Periph vasodil occurs before diuresis Safe w/o BBB Contra: co-admin w/ aminoglycoside abx & ethacrynic acid, oliguria d/t hypovol. Potentiates:antiHTN Hypo-K ↑ dig tox. & potentiates NMBA. Caution: ↓ effects if coadmin w/ NSAID’s & indomethacin, Liver dx. Category C DOESN’T cross BBB Devoid of sed. effects Small doses may prod. paradox brady. Caution: glaucoma, asthma, CAD, GI or urinary obst. Category B Elim: Renal & Heparin Sodium * Anticoagulant Inhibits thrombosis by inactivating. factors: IX, X, XI, XII. Inhibites conversion of prothrombin to thrombin, forms complexes with thrombin to inactive. and prevent stable fibrin formation. IV: immed. SC: 20-30 min. Hepatic IV/SC: 1-3 hrs (1/2 life) Elim: Hepatic IV Flush: 10-100 units Prophylaxis: Low-dose: SC 5000U 2hrs preop → q 12 hrs Full-dose SC: IV 5000U & SC 10-20K U → SC 8-10K U q 8 hrs or 15-20K U q 12 hrs. Full-dose IV: IV 5000U → infusion 20-40K U/24 hrs. Bypass Surgery: Prophylaxis/Tx of thrombus/emboli Anti-coag for Bypass Dx and Tx DIC ↑ bleeding/ hemorrh. (monitor: plt, HCT, occult stool & urine). TCP, ↑ AST/ALT Injection site rxn. Hypersensitivity Priapism Erratic SC absorption NO IM admin. ↑ risk of bleed w/ coadmin of plt. aggreg. inhibitors. Caution: effects ↓ w/ Dig, Propran., Tetracyc., Nicotine, Antihistamine. Contra: TCP, non-DIC uncontrolled active IV 350-450U/kg Goal ACT : 400-480 sec Goal aPTT: 1.5-2 x control (control normal: 25-35 sec) Reversal: Protamine slow IV 1mg per 100U Hydralazine (Apresoline) * Antihypertensive Vasodilator Keterolac (Toradol) * NSAID IV: 2-4 hours Dilation: IM/PO: 2-8 hrs. IV/IM 2.5-40 mg PO: 10-100mg 4 x daily (↑ dose w/ rapid acetylators) Direct relaxant effect on arteriolar smooth muscle. Interferes with Ca transport in vascular smooth muscle. ↓ BP & SVR ↑ CO & SV IV: 5-20 min. PO: 0.5-2 hrs Elim: Hepatic Inhibits prostaglandin synthesis. Casues analgesia, ↓ inflamm., ↓ plt aggregation & ↑ bleeding time, & antipyretic. IV: <1 min. IV/IM: 3-7 hrs IM: 10-30 min. bleed. HTN ↓ afterload w/ CHF HTN secondary to preeclampsia, eclampsia, primary pulmonary HTN. (acetylation) Analgesic: IV/IM 30mg q 6 hrs. PRN **MAX: 120mg daily IM: <10 min. Analgesia - mild to moderate pain >65 y/o, RF, Kids, <50kg: Elim: Renal & Hepatic IV 15mg q 6 hrs. PRN IM 30mgq 6 hrs PRN **MAX: 40mg daily NOT recomm. as pre-med Tachy, hypoTN, angina, palpitations Dyspnea, congestion HA, dizzy, anxiety Periph neuritis N/V/D, urticaria SLE-like syndrome Splenomegaly Leukopenia, esinoph. Agranulocytosis GI bleed, peptic ulcer ↑ risk RF w/ ↓ renal fxn, HF, LF, elderly, on diuretics. Vasodil, pallor, angina, N/V/D Dyspnea, asthma Drowzy, dizzy, HA, sweating, euphoria Puritis, urticarial. 30mg = 9mg Morphine - w/ ↓ SE Labetolol ( Normodyne ) (Trandate) *Antihypertensive Blocks adrenergic receptors at ɑ1, ß1, & ß2. IV: ɑ-ß blockade ratio of 1:7 PO:ɑ-ß blockade ratio of 1:3 IV: 2-5 min. PO: 20 min.2hrs. Lidocaine * Class Ib Antiarrhythmic PO: 8-24 hrs. Elim: Hepatic, HTN: Slow IVP 2.5-20mg/2 min. (titrate to desired response) Infus 0.5-2mg/min. ** MAX: 1-4mg/kg PO 100-400mg 2 x daily HTN (dose dep. ↓) - w/o profound ↓ HR Bronchoconstriction - prior hyper airway. Dyspnea Maskes ↓ BG HypoTN, brady, CHF VT/VF, angina, HA Drowsiness, vertigo Paresthesia, tremor Cognitive dep., rash Numbness, fatigue Dizziness, diarrhea Cholestasis, ↑ LFT’s. Ventricular arrhyth. LA, epidural/spinal. Attenuate pressor resp. or Succs induced fasciculation. HypoTN, brady, arrhyth. CHB. Resp dep. Seizures Potentiates Succs Urine & Feces Slows HR, decreases SVR, cardiac output, B/P. ɑ1, ß1, and ß2 receptors Blocks Na Channel receptors. IV: 2-4 hrs. IV: 45-90 sec LT: 10-15 sec IV: 10-20 min. Induction (attenuate): LT: 30-50 min. IV 1.5-2 mg/kg 2-3 min prior to intub/Sux LT 2 mg/kg Infiltration: 30-60 min. Infiltration: 0.5-1 min. Elim: Hepatic & Pulm. LA: Topical 0.6-3 mg/kg Infiltration/periph NB 0.5-5 mg/kg Anti-Arrhythmic: Slow IVP: 1-1.5 mg/kg → 0.5 mg/kg q 2-5 min Category C - NO cross placenta NO ↓ in renal, uterine, or cereb. BF. Interactions: ↓ rxn to Epi, ↑ hypotn w/ MAOI’s, diuretics, dizoxide, anti-HTNs, ↑Desfl & Enflurane. Category C NO ↓ in MAC Use limit: 5 days No effect on plt. count, PT, or PTT. Interactions: ↑ tox. of Lith. & methotrexate Contra:ASA, NSAID, anti-coags, (↑ bleed) salicylates (↑ effects), Hx PUD & GI bleed, hypovol risk, any bleeding Hx or acute. Incomp: morphine, meperd., hydrolazine Promethazine. Category C - contra in L&D NO change in CBF or ICP. Interactions: ↑ bioavail. w/ cimetidine, ↑ resist. to ß2 dilators hypoTN ↑ w/ Volities. Contra: asthma, HF, >1sr deg. HB, cardioshock, severe brady. Caution: abrupt d/c ↑ isch/MI risk w/ CAD. Caution: hypovol., CHF, Shock, all heart blocks. Category B Magnesium Sulfate *mineral Presynaptic: regulates release of Ach at nerve endings, enzyme active., req. for ox. phos. (ATP). NMJ: ↓ Ach release, ↓ motor end plate Ach sensitivity, ↓ amplitude of MEP potential. IV: immed. IV: 30 min. IM: <1hr. IM: 3-4 hrs. Torsades: IV 1-2g over 30-60 sec q 5-15 min. PRN Metoclopramide ( Reglan) * Antidopaminergic Hypo-Mg, toxemia/ eclampsia/tocolytic, epilepsy, nephritis. Torsades, AMI, hypo-K w/ arryth. Resp. dep., CNS dep., brady, hypo, CHB, wide QRS-I, vasodil., loss of deep tendon reflexes, flaccid paralysis. hypothermia Hypo-Ca High dose: ↓ ABP Pregnancy: transient ↓ uterine vasc. resist., ↑ uteroplacental BF. Potentiates: depol & ↑ gastric emptying antiemetic Tx DM gastroparesis, Tx symptomatic GERD HTN, hypoTN, arrhyth. ↑ catechol. release Drowsiness, anxiety insomnia, akathisia Minimal sedation EPS rare N/D, ↓ BG Caution: pt w/ HTN, Analgesia (potent) Anesthesia Reverse resp dep. of Opioid agonists. ↑ withdrawl S&S (w/ Narc-dep. pts) HTN, hypoTN Tachy, brady. Resp dep, dyspnea, asthma. Sedation, confusion Euphoria, dysphoria. Cramps, dyspepsia Puritis, burning. Urinary urgency ↑ gallbladder pain ↑ SNS activity (HTN, tachy, arrhyth, pulm. edema) Goal plasma Mg: **1.5-2.2mEq/L Reversal: Ca Gluc. 5-10 mEq (10-20ml of 10%) - fluid loading & diuretic Sensitizes GI smooth muscle to Ach causing ↑ motility of upper GI tract & ↑ LES tone. Antagonism of dopamine receptors & inhib of CTZ result in ↓ N/V. **MAX: 300mg/hr Hypo-Mg: (10-20% soln.) IV 10-15mg/kg/15 min→1g/hr. IM 10-15mg/kg q6 x 4 PO 3g q 6 hrs. x 4 IV: 1-3 min. Elim: Renal Toxemia/Eclampsia/Tocolysis: - maintain UO at 100ml q 4hrs. Slow IV 1-4g → Infus. 1-2g/hr Therapeutic plasma Mg: IV/IM/PO: 1-2 hrs. Aspiration Risk: IM: 10-15 min PO: 30-60 min. **4-6mEq/L IV/IM 10mg/ 1-2 min. PO: 10mg 30 min. before meals & at bedtime. Elim: Renal Dopamine receptor antagonist, selective cholinergic agonists. Nalbuphine (Nubain) * Synthetic Opioid agonist-antagonist Binds to opioid receptors within the CNS, narcotic agonistantagonist. IV: 2-3 min. IV/IM/SC: 3-6 hrs. IM/SC: <15 min. Mu, Kappa & Delta receptors (Narcan) **Reversal Rx** Neostigmine (Prostigmine) Competitively inhibits opiates at Mu, Delta, & Kappa receptor sites, & prevents or reverses the effects of opiate Opioid Mu, Delta, & Kappa receptors Inhibits hydrolysis of Ach by competing w/ Ach for attachment to Ach-esterase at the Induction: ↓ dose: w/ elderly, hypovol., coadmin of Narcs & sedatives. Analgesic Potency: = to Morphine Antagonist Potency: IV/IM/SC 0.2-0.4mg or ↑ Naloxone IV/IM/SC 5-10mg IV 0.3-3mg/kg Elim: Hepatic Reversal: Narcan Analgesia/Sedation: 1/4th of Nalorphine IV/ETT: 1-2 min. IM/SC: 2-5 min. IV/IM/SC/ETT: 1-4 hrs. Elim: Hepatic Reversal/OD: IV/IM/SC 0.1-2mg q 2-3 min. PRN ETT dilute 1:1 in NS **MAX: 10 mg Kids: 10-100mcg/kg Prophylaxis/SE Tx: IV/IM/SC 0.1-0.8 mg IV: <3 min. IV: 40-60 min. ST or SVT: IV 0.25-0.5mg (tx cause) Reversal of NMBA: Slow IV 0.05mg/kg with… Reversal of opioid Narcotic dep/sedation. Adjunt for other Rx OD’s, Narcotic SE prophylaxis/tx. Help reverse hemodyn. instability in septic & cardiogenic shock pts. Reversal of nondepolarizing NMBA. Tx Myasthenia Gravis Tx post-op urinary N/V d/t rapid admin. non-dep NMBA, CSN dep w/ seds, narcs, & volatiles. Monitoring: assess patellar reflex before repeat dose. Contra: CHB & extensive heart damage. Life-threatening hyperMg can be Tx w/ Ca Gluconate. MAOI’s, ↑ GI motility antagonized w/ Antichol Rx & Narcs. Potentiated: ↑ sedative effects ETOH, sedationhypnotics, tranq, Narcs. Prolongs Sucs Contra: Parkinson’s, Peds, HTN crisis w/ PheoCC pt., GI bleed, epilepsy, GI obst/perf Category B Good CV stability Potentiates: dep. effects of Narc. Rx, volatiles, sedative-hypnotics, phenothiazides. Category B - crosses placenta Caution: Resedation may occur, pt w/ cardiac disease, pt/newborns physically dep on opioids → Acute Abstinence synd. HypoTN, trembling, seizures, sweating. Brady, tachy, AV block, hypoTN. ↑ secretions, rep dep., Bronchospasm NMBA reversal ↓ w/: animoglyc abx, hypo-K, hypothermia, resp & metabolic acidosis. * Anticholinesterase esteratic site. Causes ↑ Ach Atropine: IV 0.015mg/kg Glycopyrrolate: IV 0.01mg/kg Elim: Hepatic Binds to Ach-esterase. Tx Chol. Crisis: Pentothal (sodium thiopental) *Barbiturate Phenylephrine ( Neosynepherine) *Sympathomimetic Atropine: IV 10mcg/kg q 3-10 min PRN Enhances action of GABA receptors. IV: 10-20 sec IV: <1 min. IM/SC: 10-15 min. (Diprivan) * Sedative Hypnotic * LMW Protein Puralube (Lubricant tears) Forms an occlusive film on eye surface. Lubricates/protects eye from drying. ↓ SVR, CO, BP, CPP. ↓uterine BF N/V Resp dep. May ↓ plasma Cortisol Anaphylaxis Intra-Op: IV 0.5-1 mg/kg Barb. Narcosis: - slow IVP 8mg/kg → drip @ 0.05-0.35 mg/kg/min. IV: 15-20 min. Hypotension during anesth.: IM/SC: 0.5-2 hrs. IV 50-100mcg SC/IM 2-5mg Infusion 10-200mcg/min. Kids: IV 1-2mcg/kg Periph vasoconstriction HypoTN. shock PSVT R-to-L shunt Prolongs anesth. (LA’s) Reflex brady, palp., arrhyth., hypoTN, HTN, precordial pain Acute pulm. edema, resp distress N/V, HA, anxiety cerebral hemorrhage Hepatic necrosis Tissue necrosis IV 0.5-1mg rapid, wait 1-1.5 min.→ if same, 2mg IV slow Maint SBP <160mmHg Elim: Hepatic IV: <40 sec IV: 5-10 min. Shunt Reversal: Induction: Intra-Op: IVP 25-50mg Infusion 100-200mcg/kg/min. Sedation: Elim: Hepatic IV: 0.5-1 min. ↓ BF to: renal, skin, splanchnic & uterine. ↑ PAP IV 50-100mcg Slow IV 2-2.5mg/kg/ 30 sec GABA receptor agonist Combinds with Heparin to form a stable complex devoid of anti-coag activity. Results in ↓ of anticoagulant activity of Heparin Induction: IV 3-5mg/kg - high Vol. distrib. - rapid elim. Protamine sulfate Induction, to ↓ ICP, anticonvulsant, cerebral protection (Barb coma). IM/SC 0.25-1mg q 4-6 hrs PSVT: Extravasation: Propofol IV: 5-15 min Elim: Hepatic No analgesia Phentolamine SC 5-10mg in 10ml NS Produces sedative/ hypnotic effects via interaction with GABA. Seizures, HA N/V/F, ↑ peristalsis ↑ urinary frequency Anaphylaxis OD: cholinergic crisis & plasma esterases Ultra short-acting Activates alphaadrenergic receptors of the vascular smooth muscle. Causing vasoconstriction of the arterioles. Little ß effects. Alpha-adrenergic receptors Post-Op Retention/Ileus: retention & ileus. Adjunct Tx: ST or SVT IVP 25-50mg (titrate slowly desired effect slurred speech) Maintenance of anesthesia: 100300 mcg/kg/min (typical ICU max dose is 50 mcg/kg/min) IV: 2 hrs. IV: slow 1mg neutralizes 90-115 Elim: Hepatic units of Heparin > 30-60 min: give ½ dose > 2 hrs: give ¼ dose Induction/maintenance of anesthesia. - blunts resp. to intub. Chemotherapy or postop N/V. HypoTN, ↓ SVR, apnea. ↓: cerb. BF, MBR, ICP. Tx severe Heparin OD **MAX: 50mg/10 min. Place small amount in the conjunctival sac PRN Protection/lubrication of eye during and following surgery Post removal of a HypoTN, HTN, fever arrhyth. tachy, brady Resp dep., apnea Broncho/larynospasm Hiccups, HA, dizzy. confusion, euphoria. Seizures, clonic/ myoclonic movement. N/V, abd cramps. Pain at IV site Erythema, urticaria. Histamine release poss.: prod. anaphyl. HypoTN, HTN, brady Pulm. HTN, dyspnea Bronchospasm Anaphylaxis (or rxn) N/V, flushing, TCP Hyperheparinemia Temp. blurring post admin. Caution: pt w/ brady, asthma, epilepsy, arrhyth., peptic ulcer. Contra: pt w/ peritonitis, bowel or urinary obstruction. Category C Incomp: Succs & Rx w/ acid pH. Contra: status asthmaticus, & all Porphyria’s. Caution: MAOI’s, HTN, Hypovol., cardiac ischemia, Septic. Category C ↑ pressor effects w/: oxytocics, bretylium, guanethidine, MAOI’s & other sympathomimetics. Caution: elderly, ↑thyroid, brady, partial HB, severe arteriosclerosis. ↑ arrhyth w/ volatiles Contra: IV regional, LA of end organs. Category C Interactions: ↑ CNS & CV effects w/ Narcs, sed-hypnotics, Volatiles. ↓ resp. cl. w/ Afent/fentanyl. Caution: pt w/ ↑ ICP, Hx seizure/epilepsy, Csection, generic has ↑ allergic rxn. Contra: allergy to eggs &/or soybean oil. Category B Rapid IV:↑ histamine - anaphyl., hypoTN Interaction: ↑ effects of vasodilators. Incomp: PCN, Cephlo Caution: fish allergy, Insulin w/ protamine. Category C * Eye Lubricant Rocuronium Bromide (Zemuron) foreign body. Competes for cholinergic receptors at the motor end plate. Nicotinic receptors IV: 1-2 min. IV: 15-120 min. (dose dependant) Intubation: IV 0.6-1.2mg/kg (add’l doses at 10-50% intub. dose). **base on actual body weight Facilitate tracheal intubation. - esp. if can’t use Succs Rapid acting * Non-depolarizing NMBA Sodium Bicarbonate *Buffer Sodium Nitroprusside (Nipride) (Nitropress) *Antihypertensive Vecuronium (Norcuron) Elim: Renal & Reversal: Monitor: w/ nerve stimulator to Tachy, arrhyth. Hypovent./apnea Bronchospasm Pulm. HTN Pruritis, rash Edema at IV site Histamine SE rare min. OD. Hepatic Anticholinesterase Rx w/ Atropine or Glycopyr. Dissociates to form HCO3- & Na. Buffers excess H ions, promotes cell uptake of K. IV: 2-8 min. Potent peripheral vasodilator at arterial & venous smooth muscle. Generates NO, which activates smooth muscle guanylate cyclase forming ↑ IC cGMP. To cause relaxation: cGMP inhibits Ca from moving into the cell. NO causes hyperpol. at K channels leading. cGMP also acts on myosin at the sarcomere. ↓PVR, preload, afterload & ↑ CO. Competes for cholinergic receptors at the motor end plate. Nicotinic receptors IV: 30-60 sec IV: 30-60 min. Elim: Renal IV: 1-10 min. Correct Metabolic acidosis, urinary alkalization, ACLS. Alkalization of urine: Peripheral vasodilation: IV: 25-30 min. ↑ w/: animogl. abx, LA, Mg, lithium, ganglionic blockers, hypo therrmia, hypo-K, resp acidosis, Succs, Volatile, loops, MG, adrenocort. dysf. Req ↓ & w/: Volatiles Recurrent paralysis w/ quinidine. Reversal effects ↓ w/ & theophylline, anticonvul. rx, burn pt, & paresis. Category C Incomp: Ca ↑ EtCO2 Category C HTN Crisis, HTN, controlled hypoTN, acute CHF, pre-heart transplant. HypoTN, tachy, circ. collapse, palpitations. ↑ ICP, HA, ↓ thyroid. N/V-retching Methheme., Cyanide tox., thocy. tox. antiplt effect. May ↑ V/Q mismatch ↓ uterine BF Cyanide Tox S&S: Tachyphylaxis, ↑ MvPO2, metab acid Thiocy. tox S&S: Elim: Hepatic IV: <3 min. Metabolic alkalosis, hypo-K Carpopedal spasm w/hypo-Ca pt. IV 48mEq, → 12-24mEq q 4 hrs. **1 AMP = 50mEq **MAX: 10mcg/kg/min for 10 min. **Protect from light Caution: RF ↑ tox risk, ↑ fetal cyanide risk if mother under gen. anesth. HypoTN poten. by: Volatiles, antiHTN , ganglionic BA, circulatory dep Rx. Contra: pt w/ compensatory HTN, inadequate cerebral BF. (> 10mg/100ml) Sk. muscle weakness N/V, confusion. - lab req if inf >48hrs Intubation: IV 0.08-0.1mg/kg Intra-Op: Hepatic Reversal: 0.5mEq/kg q 10 min. Acidosis: IV (kg x mEq/L deficit x 0.3) /2 IV infusion: 10-300mcg/min. Elim: Renal & * Non-depolarizing NMBA ACLS: IV 1mEq/kg, → Interactions: NM block IV 0.01-0.0mg/kg initially Infusion 1-2 mcg/kg/min Monitor: w/ nerve stimulator to min. OD. Facilitate tracheal intubation. Hypovent./apnea Prolonged paralysis w/ long-term infusion - RF, ↓K, ↓Ca, ↑Mg, amino abx, corticoster. Brady w/ co-admin of potent opioids. Histamine SE rare Interactions: NM block ↑ w/: animogl. abx, LA, Mg, lithium, ganglionic blockers, hypo therrmia, hypo-K, resp acidosis, Succs, Volatile, loops, MG, adrenocort. dysf. Req ↓ & w/: Volatiles Recurrent paralysis w/ Verapamil (Calan) (Isoptin) * CCB Anticholinesterase Rx (Neostigmine) w/ Antichol. (Atropine or Glycopyrrlate). Selectively inhibits influx of Ca ions into cardiac & smooth muscle Antiarrhythmic effects are d/t inhibition of Ca influx through slow channels in pacemaker cells. AV conduction is slowed & the effective refractory period is prolonged. Calcium channel receptors IV: 2-5 min. PO: 30 min. IV: 30-60 min. PO: 3-7 hrs. (1/2 life) PSVT, A-Fib or A-Flutter: IV 5-10 mg/ 2 min q 30 min PRN HTN: IV 2.5-10mg (titrate) PO 40-80mg (RR) 3 x daily Chronic A-Fib (on Digoxin): Elim: Renal PO 240-320mg/day (RR) - taken in 3-4 divided doses PSVT (NOT on Digoxin): PO 240-480mg/day (RR) - taken in 3-4 divided doses Tx SVT (PSVT) Temp. control of A-fib or A-flutter w/RVR not assoc. w/ accessory pathway. HTN, angina Migraine prophylaxis ↓: Contractility, HR, SVR, ABP, myocardial demand. HypoTN Brady, tachy Worsen HF w/ poor LV fxn pts. Bronchospasm Laryngospasm HA, dizzy, seizures N/V, Abd pain Urticaria, puritis Tx RVR with WPW: Procainamid, Lidocaine, cardioversion. quinidine. Reversal effects ↓ w/ theophylline. Category C Interactions: ↑ effects of ALL NMBA, CV dep effects are additive w/ Volatiles & Anti-HTN Rx’s, ↑ cardiac risk w/ co-admin of BB, ↑ cardiac dep effects of Bupiv. & LA’s, ↓ Lithium effects, ↓ cl. w/ cimetidine, levels ↑ w/ grapefruit. Enzyme Inhibitor Incompatible: Bicarb & Nafcillin Caution: pt on highly protein-bound Rx’s. Tx Brady or AV block: Versed (Midazolam) *Benzo Isopro., CaCl, NE, Atropine, Pacing. Enhances action of GABA receptors. GABA receptor agonist. IV: 0.5-1 min. IM: 15 min. PO: <10 min. Reversal: Flumazenil IV/IM: 15-80 min. Pre-Op: IM 2.5-10 mg PO 0.25-0.5mg/kg (kid) Conscious Sedation: PO: 2-6 hr. IV 0.5-5 mg Elim: Renal Infusion 2-15 mg/hr Induction: 0.25mg/kg IVP 1-2.5 mg PO 0.5 mg/kg slow IV 0.2-1 mg Deep sedation: Pre-med, sedation, induction, anxiolytic, amnesia, anticonvulsant. ↓ RR, Possible ↓ BP Contra: NA glaucoma ↓ dose >60y Category D ↓ MAC req. Other Meds not listed on the REQ sheet Drug: Mech of action & Receptor: Onset: Duration of action: Normal Dose: Uses: Risks: Other: Succinylcholine Combines w/ chol. receptors at the motor end plate to depol.observed as fasciculations. Prod. flaccid paralysis. IV: 30-60 secs. IV: 5 mins Induction: Sleletal muscle relaxation Induction ↓or↑ BP, ↓or↑ HR, arrhyth. ↑ LES press. (Aspir.) Prolonged blockade w/: ↓K, ↓Ca, ↓ pseudochol-ase, phenelzine, BB, lidocaine, procainamide, reglan, , Mg, oxytosin, Volitiles, trimethaphan, Anticholase,pre-tx w/ Panc, MAOI’s, BCP. Blockade ↓ w/: pre-tx ND Will ↑ K (0.5mEq in normal pt) Unpred resp w/: MG Contra: severe burns, ↑ K, -lyte imbal., trauma, ↑ IOP, paraplegia, sp.cord injury. Histamine r not signif. Inconp. w/ Alkaline soln. Repeat dose: ↑ brady Preg: ↑ sensitivity, NO (Anectine) *DEPOL. NMB Reversal: Anticholinesterase Rx (Neostigmine) w/ Antichol. (Atropine or Glycopyrrlate). Peak: 60 secs 0.7-1mg/kg (1.5mg/kg w/ ND pre-tx) Elim: plasma pseudochol-ase Neonates & Infants: 2-3mg/kg Children: 1-2mg/kg Ultra-short acting Monitor w/ nerve stimul MH: Tx w/ Dantroline 2.5mg/kg Methergine (Methylergonovine Maleate) * Semisynthetis Ergot Alkaloid Metoprolol (Lopressor) Act directly on uterine smooth muscle: ↑ tone, rate, & amplit. of contractions. ↓ 3rd stage of labor & ↓ bleeding IV: immed IM: 2-5 mins IV:.45 mins IM: 4-6 hrs Peak: IV: <5 min IM: <30 min Elim: Hepatic Cardio-selective BB Can block ß2 in high doses IV: immed IV/PO: 5-8 hrs *Antihypertensive IV/IM: 0.2mg over 60 secs Repeat q 2-4 hrs HTN & Angina: PO: 50-400mg daily PO: <15 mins Elim: Hepatic AMI: Tx postpartum uterine atony & bleeding HTN, SVT, AMI, antianginal, ETOH withdrawal IV: 5mg q 2mins x 3 Peak: IV 20 mins. NMB. MH: ridgidity (esp jaw), tachy, tachypnea, unresp to ↑ Volatiles. ↑or↓ BP, chest pain, dyspnea, ↑ CVP & PAP, tinnitus, HA, SZ, N/V/D, hematuria, extremity necrosis D/C w/ c/o: tingling in extremities ↓ BP, arrhyth, rebound angina, bronchospasm, dyspnea, cough, N/V, TCP purpura, arthralgia. Mask S&S of ↓ BG effect on Uterus or other smooth muscle. Category C Vasoconstr. potent. w/: ephedrine, phynel., nicotine Caution: preeclampsia, HTN, heart disease. Avoid in pt w/: PVD Limits lactation, IS in breast milk. ↓ BP worse w/: Volatiles, ↓ catechol. Potentiates: ALL NMBA ↑ levels: Dig & morphine Rebound HTN w/ abrupt d/c Contra: brady, HB >1°, cardio shock Propranolol Indigo carmine Methylene Blue Oxidation-reduction rxn IV: immed Peak: <1 hr Varies Elim: Renal IV: 1-2mg/kg over minutes PO: 65-130mg q TID (Urolene Blue) Solu-cortef ancef Decadron Oxytosin Physostigmine Promethazine Zofran Nitroglycerine Pepsid Nitrobid 2% Tx Rx induced methemoglobinemia ↑ HR, HTN, cyanosis, confustion, HA, N/V/D, abd pain False ↓ in SaO2 <85% or false ↑ SaO2 >85% Hemolytic Anemia Hyperbilirubinemia BLUE skin color Discolor. of UO & feces Contra: RF pt