Transdisciplinary Approaches to Diabetes Care for Children
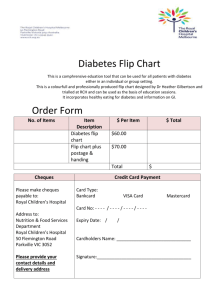
advertisement

Transdisciplinary Approaches to Diabetes Care for Children Written by Yael Shaked Diabetes is a chronic illness, in which the body either cannot properly use the insulin it produces or cannot produce insulin at all. Insulin is a hormone that controls the amount of glucose (sugar) in the blood, which the body requires as an energy source. Diabetes leads to high blood glucose levels that can cause severe long-term complications by damaging organs, blood vessels and nerves. If untreated, diabetes may result in death. There are more than 10 million Canadians living with diabetes or pre-diabetes today [1]. With respect to young children, there are two types of diabetes which should be taken into consideration: type 1 and type 2 diabetes. Type 1 Diabetes Type 1 diabetes (T1D) occurs when pancreas cell which produce insulin, called beta cells, are mistakenly attacked and killed by the immune system. As a result, no or very little insulin is released into the body, thus necessitating insulin administration as treatment [1]. A growing number of individuals worldwide have T1D [2], with approximately 70,000 newly diagnosed cases each year, an increase rate of 3-4% annually [3]. Only about 5-10% of those with diabetes have T1D [1]. T1D is commonly diagnosed in childhood although it is not uncommon for it to manifest later in life among adults as well [1, 4, 5]. It has previously been demonstrated that pediatric illnesses have negative health and mental health implications on adult outcomes. Such implications include lower levels of education and income among those with illnesses diagnosed in childhood, in comparison to the general population [6]. T1D is unique among chronic illnesses of children in terms of the complexity of its treatment. Its therapeutic regimen consists of blood glucose monitoring, insulin administration, diet management, and physical activity [7]. The degree of family involvement required for the successful management and prevention of long-term complications is high as well, since diabetes affects virtually every aspect of daily living. Thus, its ongoing management is often burdensome and often complicates other challenges faced by individuals with T1D and their caregivers [8]. As a result, conflict is often observed among families caring for a child with T1D, as parents and caregivers have much added stress, responsibilities, and demands to their daily regimen [9]. In addition to the normal developmental tasks and milestones which all children must meet, those with T1D and their caregivers have additional healthcare priorities that must be dealt with. For young children, these include, among others, preventing and treating extreme fluctuations in blood glucose levels, coping with unpredictable appetite and activity, and trusting others with care for the child in settings such as preschools [10]. Family conflict has previously been found to be negatively related to T1D treatment adherence [11]. Thus, it is crucial for health professionals take an active role in mediating these conflicts and supporting individuals and families through various life transitions. Type 2 Diabetes Type 2 diabetes (T2D) occurs when the body cannot properly use the insulin that is released or does not make enough insulin. Depending on its severity, T2D can often be managed through physical activity and meal planning, but it may also require medications and/or insulin [1]. T2D usually develops among adults and is not typically diagnosed among children [1], although there is increasing incidence of T2D diagnosis among children above the age of 10 [12]. Factors related to increased probability of a child developing T2D are the same as those seen among adults. They include overweight and obesity, physical inactivity, a family history of diabetes, certain ethnicities, maternal gestational diabetes and insulin resistance [13]. As todays childhood population is becoming increasingly overweight, T2D incidence is expected to rise among younger pre-pubertal children [12, 14]. Thus, it is crucial to identify children at risk, as early as possible, in order to intervene and reduce incidence of T2D and to prevent further complications later in life [15]. Transdisciplinary Approaches to Diabetes Care for Children Written by Yael Shaked Transdisciplinary Care for Children with Diabetes & their Families: The traditional medical model of care, considers the physician as active and responsible for the patient’s care and wellbeing, while the patient is viewed as passive and dependent on the physician's medical knowledge [16, 17]. This model has received much criticism, especially with respect to management of chronic conditions such as diabetes, in which the vast majority of the health care is provided by the patients and caregivers themselves [17]. One improved patient care model is called the Patient Empowerment Model. This model uses a patient-centred approach and views the patient as the one in charge of their own healthcare regime [17]. In this model, the patients and their parents/caregivers are seen as the experts on their own life and individual needs, while the healthcare team is viewed as the expert on the condition and the resources available [18]. Moreover, previous literature has emphasized the importance of self-management in pediatric care, indicating that self-management interventions must be delivered across multiple contexts with interlocking influences including the individual, family, community, and health care systems (an ecological approach). These must all be taken into account for the sustainment of self-management and treatment adherence. Viewing the child with diabetes within the contexts of their life and working with all of the relevant contexts in a coordinated manner will have greater impact on long-term health outcomes and healthcare costs [19]. Transdisciplinary healthcare providers are advised to work within the framework of the Patient Empowerment model, while taking into account the multiple additional contexts with which a child with diabetes deals, as this serves as an ideal care model for children with diabetes and their families. Diabetes among young children is a complex condition, which has both health and mentalhealth implications not only for the children with diabetes, but for their and caregivers as well. Thus, whenever possible, management of diabetes for this population should be conducted within a transdisciplinary healthcare setting to include doctors, dieticians, nurses, and mental-health professionals (such as social workers and psychologists). It is advised for the transdisciplinary team to work collaboratively in order to try to anticipate situations which may be encountered by the child and caregivers, specific to each patient. They should be available to assist in finding quick solutions to any situation that may arise, in order to aid in keeping the children and their families in full control. By doing so, self-efficacy will be improved and future medical and emotional complications will be reduced. The interventions should be provided not only to the diagnosed children, but also to their extended family, as they are all in higher risk of developing diabetes and complications related to this illness. Various healthcare professional can deal with the different aspects of diabetes. For instance: Doctors Dealing with the medical aspects of the illness as well as with the management of non-routine situations and their impact on blood glucose levels. For instance: stress from situations such as family conflict, moving to a new environment, weening from pacifier… etc. Dieticians Nurses Social & Mental health Assisting with lifestyle Focusing not only on Being routinely changes relating to patient and family, but involved in the care nutrition and also on community process to continually exercising, including caregiver education monitor coping of all those involved in within the various child and caregivers. the child’s care. settings that the child Varied interventions participates in, in should be put in place order to increase for newly diagnosed family support, children and families decrease burnout, and and for those who have reduce missed days been dealing with that can affect the diabetes on an ongoing child’s progress and basis as their unique integration within needs differ these settings. substantially [9]. Transdisciplinary Approaches to Diabetes Care for Children Written by Yael Shaked 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. References Canadian Diabetes Association. About Diabetes: Types of Diabetes. 2015; Available from: https://www.diabetes.ca/about-diabetes/types-of-diabetes%20-%20sthash.yO2l48NJ.dpuf. Gale, E.A.M., The Rise of Childhood Type 1 Diabetes in the 20th Century. Diabetes, 2002. 51(12): p. 3353-3361. Tuomilehto, J., The emerging global epidemic of type 1 diabetes. Curr Diab Rep, 2013. 13(6): p. 795-804. Borchers, A.T., R. Uibo, and M.E. Gershwin, The geoepidemiology of type 1 diabetes. Autoimmun Rev, 2010. 9(5): p. A355-65. Imayama, I., et al., Determinants of quality of life in adults with type 1 and type 2 diabetes. Health Qual Life Outcomes, 2011. 9: p. 115. Ahlfield, J.E., N.G. Soler, and S.D. Marcus, The young adult with diabetes: impact of the disease on marriage and having children. Diabetes Care, 1985. 8(1): p. 52-6. American Diabetes Association, Standards of medical care in diabetes. Diabetes Care, 2010. 33 Suppl 1: p. S11-61. Hanna, K.M. and D. Guthrie, Parents' and adolescents' perceptions of helpful and nonhelpful support for adolescents' assumption of diabetes management responsibility. Issues Compr Pediatr Nurs, 2001. 24(4): p. 209-23. Anderson, B.J., Family Conflict and Diabetes Management in Youth: Clinical Lessons From Child Development and Diabetes Research. Diabetes Spectrum, 2004. 17(1): p. 22-26. Chiang, J.L., et al., Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes Care, 2014. 37(7): p. 2034-54. Schafer, L.C., K.D. McCaul, and R.E. Glasgow, Supportive and nonsupportive family behaviors: relationships to adherence and metabolic control in persons with type I diabetes. Diabetes Care, 1986. 9(2): p. 179-185. American Diabetes Association, Type 2 diabetes in children and adolescents. Diabetes Care, 2000. 23(3): p. 381-9. Public Health Agenct of Canada. Chapter 5 – Diabetes in children and youth Diabetes in Canada: Facts and figures from a public health perspective 2011; Available from: http://www.phac-aspc.gc.ca/cd-mc/publications/diabetes-diabete/facts-figures-faits-chiffres2011/chap5-eng.php. Tremblay, M.S., Major initiatives related to childhood obesity and physical inactivity in Canada: the year in review. Canadian Journal of Public Health/Revue Canadienne de Sante'e Publique, 2012: p. 164-169. D’Adamo, E. and S. Caprio, Type 2 Diabetes in Youth: Epidemiology and Pathophysiology. Diabetes Care, 2011. 34(Supplement 2): p. S161-S165. Laing, R.D., The politics of the family, and other essays. 1999, London: Routledge. Anderson, R.M., Patient empowerment and the traditional medical model. A case of irreconcilable differences? Diabetes Care, 1995. 18(3): p. 412-5. Funnell, M.M., et al., Empowerment: an idea whose time has come in diabetes education. Diabetes Educ, 1991. 17(1): p. 37-41. Modi, A.C., et al., Pediatric self-management: a framework for research, practice, and policy. Pediatrics, 2012. 129(2): p. e473-e485.