Introduction to the Managed Care Annual Filing Process
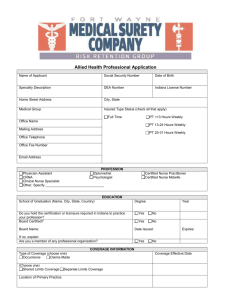
advertisement

NC Managed Care Annual Filing Training Manual March 2013 TABLE OF CONTENTS 1. INTRODUCTION TO MANAGED CARE ANNUAL FILINGS .................................... 1 2. INTRODUCTION TO THE MANAGED CARE ANNUAL FILING PROCESS............ 7 2.1. Exemptions:................................................................................................... 8 2.2. Abbreviated Filings: ...................................................................................... 8 2.3. Forms: ............................................................................................................ 9 2.4. Riders: ............................................................................................................ 9 2.5. Addition or Replacement of an Intermediary/New Product Line: ........... 10 2.6. Review Process: .......................................................................................... 10 3. INTRODUCTION TO THE CERTIFICATIONS ........................................................ 12 4. C1. COMPLIANCE CERTIFICATION: ANNUAL FILING CHECKLIST ................ 13 4.1. Initial Filers & New Intermediary Form (Supplemental Checklist) .......... 13 5. C2. COMPLIANCE CERTIFICATION: OVERALL ATTESTATION ....................... 14 6. C3A. COMPLIANCE CERTIFICATION: GRIEVANCE PROCEDURES / C3B. COMPLIANCE CERTIFICATION: EXTERNAL REVIEW RELATED TO GRIEVANCES ......................................................................................................... 15 7. C4A. COMPLIANCE CERTIFICATION: DELEGATED GRIEVANCE PROCEDURES / C4B. COMPLIANCE CERTIFICATION: DELEGATED EXTERNAL REVIEW RELATED TO GRIEVANCES .............................................. 20 8. C5A. COMPLIANCE CERTIFICATION: UTILIZATION REVIEW / C5B. COMPLIANCE CERTIFICATION: EXTERNAL REVIEW RELATED TO UTILIZATION REVIEW ........................................................................................... 26 9. C6A. COMPLIANCE CERTIFICATION: DELEGATED UTILIZATION REVIEW / C6B. COMPLIANCE CERTIFICATION: EXTERNAL REVIEW RELATED TO UTILIZATION REVIEW ........................................................................................... 32 10. C7 COMPLIANCE CERTIFICATION: INTERMEDIARY ARRANGEMENTS ......... 40 11. C8. COMPLIANCE CERTIFICATION: PROVIDER AVAILABILITY AND ACCESSIBILITY...................................................................................................... 47 12. C9. COMPLIANCE CERTIFICATION: DELEGATED PROVIDER AVAILABILITY AND ACCESSIBILITY ............................................................................................. 56 13. INTRODUCTION TO THE DATA GRIDS ................................................................ 66 14. COVER PAGES....................................................................................................... 68 15. D1. ENROLLMENT/DISENROLLMENT SUMMARY .............................................. 69 Managed Care Annual Filing Training Manual 3.2013 16. D2. ENROLLMENT BY COUNTY ........................................................................... 70 17. D3. GRIEVANCES, BY REASON ........................................................................... 71 18. D4. UTILIZATION REVIEW DECISIONS, BY REVIEW TYPE / D5. UTILIZATION REVIEW DECISIONS, BY SERVICE TYPE ............................................................ 73 19. D6. PROVIDERS BY COUNTY ............................................................................... 75 20. D7: UNIQUE PROVIDERS ON NETWORK ........................................................... 78 21. D8: UNIQUE PROVIDERS LEAVING NETWORK ................................................. 79 22. D9: UNIQUE PROVIDERS JOINING NETWORK .................................................. 81 23. D10. NETWORK DENSITY, TARGETS BY PROVIDER TYPE AND GEOGRAPHIC AREA....................................................................................................................... 82 24. D11. NETWORK DENSITY, ACTUAL PERFORMANCE, BY PROVIDER TYPE AND GEOGRAPHIC AREA .................................................................................... 85 25. D12. DRIVING DISTANCE, TARGETS BY PROVIDER TYPE AND GEOGRAPHIC AREA....................................................................................................................... 87 26. D13. DRIVING DISTANCE, ACTUAL PERFORMANCE BY PROVIDER TYPE AND GEOGRAPHIC AREA ............................................................................................. 90 27. D14. APPOINTMENT WAIT TIMES, TARGETS BY PROVIDER TYPE AND APPOINTMENT TYPE ............................................................................................ 93 28. D15. APPOINTMENT WAIT TIMES, ACTUAL PERFORMANCE BY PROVIDER TYPE AND APPOINTMENT TYPE ......................................................................... 96 29. D16. PERCENTAGE OF PROVIDERS UNDER EACH COMPENSATION MODEL / D17. RANGE OF WITHHOLDS AND BONUSES, BY COMPENSATION MODEL 99 30. D18. LIST OF PLAN’S DELEGATED ENTITIES AND NETWORK INTERMEDIARIES ................................................................................................ 101 31. SUMMARY OF “ERROR” AND “EXPLAIN” MESSAGES ................................... 104 32. PLAN/INTERMEDIARY COMMENTS ................................................................... 105 Managed Care Annual Filing Training Manual 3.2013 1. INTRODUCTION TO MANAGED CARE ANNUAL FILINGS Statutory Requirements: It is important to note that as the term “health benefit plan” is defined in NCGS 58-3-191(c), the definition of “health benefit plan” found in NCGS 58-3-167 is NOT applicable. ALL insurers (medical, vision, dental) offering managed care products (HMO/POS/PPO) with NC membership must submit all the managed care annual filing requirements outlined in NCGS 58-3-191. NCGS 58-3-191. Managed care reporting and disclosure requirements. (a) Each health benefit plan shall annually, on or before the first day of May of each year, file in the office of the Commissioner the following information for the previous calendar year: (1) The number of and reasons for grievances received from plan participants regarding medical treatment. The report shall include the number of covered lives, total number of grievances categorized by reason for the grievance, the number of grievances referred to the second level grievance review, the number of grievances resolved at each level and their resolution, and a description of the actions that are being taken to correct the problems that have been identified through grievances received. Every health benefit plan shall file with the Commissioner, as part of its annual grievance report, a certificate of compliance stating that the carrier has established and follows, for each of its lines of business, grievance procedures that comply with G.S. 58-50-62. (2) The number of participants and groups who terminated coverage under the plan for any reason. The report shall include the number of participants who terminated coverage because the group contract under which they were covered was terminated, the number of participants who terminated coverage for reasons other than the termination of the group under which they were enrolled, and the number of group contracts terminated. (3) The number of provider contracts that were terminated and the reasons for termination. This information shall include the number of providers leaving the plan and the number of new providers. The report shall show voluntary and involuntary terminations separately. (4) Data relating to the utilization, quality, availability, and accessibility of services. The report shall include the following: a. Information on the health benefit plan's program to determine the level of network availability, as measured by the numbers and types of network providers, required to provide covered services to covered persons. This information shall include the plan's methodology for: 1. Establishing performance targets for the numbers and types of providers by specialty, area of practice, or facility type, for each of the following categories: primary care physicians, specialty care physicians, nonphysician health care providers, hospitals, and nonhospital health care facilities. Managed Care Annual Filing Training Manual 3.2013 Page 1 2. Determining when changes in plan membership will necessitate changes in the provider network. The report shall also include: the availability performance targets for the previous and current years; the numbers and types of providers currently participating in the health benefit plan's provider network; and an evaluation of actual plan performance against performance targets. b. The health benefit plan's method for arranging or providing health care services from nonnetwork providers, both within and outside of its service area, when network providers are not available to provide covered services. c. Information on the health benefit plan's program to determine the level of provider network accessibility necessary to serve its membership. This information shall include the health benefit plan's methodology for establishing performance targets for member access to covered services from primary care physicians, specialty care physicians, nonphysician health care providers, hospitals, and nonhospital health care facilities. The methodology shall establish targets for: 1. The proximity of network providers to members, as measured by member driving distance, to access primary care, specialty care, hospital-based services, and services of nonhospital facilities. 2. Expected waiting time for appointments for urgent care, acute care, specialty care, and routine services for prevention and wellness. The report shall also include: the accessibility performance targets for the previous and current years; data on actual overall accessibility as measured by driving distance and average appointment waiting time; and an evaluation of actual plan performance against performance targets. Measures of actual accessibility may be developed using scientifically valid random sample techniques. d. A statement of the health benefit plan's methods and standards for determining whether in-network services are reasonably available and accessible to a covered person, for the purpose of determining whether a covered person should receive the in-network level of coverage for services received from a nonnetwork provider. e. A description of the health benefit plan's program to monitor the adequacy of its network availability and accessibility methodologies and performance targets, plan performance, and network provider performance. f. A summary of the health benefit plan's utilization review program activities for the previous calendar year. The report shall include the number of: each type of utilization review performed, noncertifications for each type of review, each type of review appealed, and appeals settled in favor of covered persons. Managed Care Annual Filing Training Manual 3.2013 Page 2 The report shall be accompanied by a certification from the carrier that it has established and follows procedures that comply with G.S. 58-50-61. (5) Aggregate financial compensation data, including the percentage of providers paid under a capitation arrangement, discounted fee-for-service or salary, the services included in the capitation payment, and the range of compensation paid by withhold or incentive payments. This information shall be submitted on a form prescribed by the Commissioner. The name, or group or institutional name, of an individual provider may not be disclosed pursuant to this subsection. No civil liability shall arise from compliance with the provisions of this subsection, provided that the acts or omissions are made in good faith and do not constitute gross negligence, willful or wanton misconduct, or intentional wrongdoing. (b) Disclosure requirements. – Each health benefit plan shall provide the following applicable information to plan participants and bona fide prospective participants upon request: (1) The evidence of coverage (G.S. 58-67-50), subscriber contract (G.S. 58-65-60, 58-65-140), health insurance policy (G.S. 58-51-80, 58-50-125, 58-50-126, 58-50-55), or the contract and benefit summary of any other type of health benefit plan; (2) An explanation of the utilization review criteria and treatment protocol under which treatments are provided for conditions specified by the prospective participant. This explanation shall be in writing if so requested; (3) If denied a recommended treatment, written reasons for the denial and an explanation of the utilization review criteria or treatment protocol upon which the denial was based; (4) The plan's formularies, restricted access drugs or devices as defined in G.S. 58-3-221, or prior approval requirements for obtaining prescription drugs, whether a particular drug or therapeutic class of drugs is excluded from its formulary, and the circumstances under which a nonformulary drug may be covered; and (5) The plan's procedures and medically based criteria for determining whether a specified procedure, test, or treatment is experimental. (b1) Effective March 1, 1998, insurers shall make the reports that are required under subsection (a) of this section and that have been filed with the Commissioner available on their business premises and shall provide any insured access to them upon request. (c) For purposes of this section, "health benefit plan" or "plan" means (i) health maintenance organization (HMO) subscriber contracts and (ii) insurance company or hospital and medical service corporation preferred provider benefit plans as defined in G.S. 58-50-56. (1997-480, s. 1; 1997-519, s. 1.1; 2001-334, s. 2.2; 2001-446, s. 2.1; 2006-154, s. 13; 2008-124, s. 10.1.) Managed Care Annual Filing Training Manual 3.2013 Page 3 NCGS 58-50-56. Insurers, preferred provider organizations, and preferred provider benefit plans. (a) Definitions. – As used in this section: (1) “Insurer" means an insurer or service corporation subject to this Chapter. (2) "Preferred provider" means a health care provider who has agreed to accept special reimbursement or other terms for health care services from an insurer for health care services on a fee-for-service basis. A "preferred provider" is not a health care provider participating in any prepaid health service or capitation arrangement implemented or administered by the Department of Health and Human Services or its representatives. (3) "Preferred provider benefit plan" means a health benefit plan offered by an insurer in which covered services are available from health care providers who are under a contract with the insurer in accordance with this section and in which enrollees are given incentives through differentials in deductibles, coinsurance, or copayments to obtain covered health care services from contracted health care providers. (4) "Preferred provider organization" or "PPO" means an insurer holding contracts with preferred providers to be used by or offered to insurers offering preferred provider benefit plans. (b) Insurers may enter into preferred provider contracts or enter into other cost containment arrangements approved by the Commissioner to reduce the costs of providing health care services. These contracts or arrangements may be entered into with licensed health care providers of all kinds without regard to specialty of services or limitation to a specific type of practice. A preferred provider contract or other cost containment arrangement that is not disapproved by the Commissioner within 90 days of its filing by the insurer shall be deemed to be approved. (c) At the initial offering of a preferred provider plan to the public, health care providers may submit proposals for participation in accordance with the terms of the preferred provider plan within 30 days after that offering. After that time period, any health care provider may submit a proposal, and the insurer offering the preferred provider benefit plan shall consider all pending applications for participation and give reasons for any rejections or failure to act on an application on at least an annual basis. Any health care provider seeking to participate in the preferred provider benefit plan, whether upon the initial offering or subsequently, may be permitted to do so in the discretion of the insurer offering the preferred provider benefit plan. G.S. 58-50-30 applies to preferred provider benefit plans. (d) Any provision of a contract between an insurer offering a preferred provider benefit plan and a health care provider that restricts the provider's right to enter into preferred provider contracts with other persons is prohibited, is void ab initio, and is not enforceable. The existence of that restriction does not invalidate any other provision of the contract. (e) Except where specifically prohibited either by this section or by rules adopted by the Commissioner, the contractual terms and conditions for special reimbursements shall be those that the parties find mutually agreeable. (f) Every insurer offering a preferred provider benefit plan and contracting with a PPO shall require by contract that the PPO shall provide all of the preferred providers with whom it holds contracts information about the insurer and the insurer's preferred provider benefit plans. Managed Care Annual Filing Training Manual 3.2013 Page 4 This information shall include for each insurer and preferred provider benefit plan the benefit designs and incentives that are used to encourage insureds to use preferred providers. (g) The Commissioner may adopt rules applicable to insurers offering preferred provider benefit plans under this section. These rules shall provide for: (1) Accessibility of preferred provider services to individuals within the insured group. (2) The adequacy of the number and locations of health care providers. (3) The availability of services at reasonable times. (4) Financial solvency. (h) Each insurer offering a preferred provider benefit plan shall provide the Commissioner with summary data about the financial reimbursements offered to health care providers. All such insurers shall disclose annually the following information: (1) The name by which the preferred provider benefit plan is known and its business address. (2) The name, address, and nature of any PPO or other separate organization that administers the preferred provider benefit plan for the insurer. (3) The terms of the agreements entered into by the insurer with preferred providers. (4) Any other information necessary to determine compliance with this section, rules adopted under this section, or other requirements applicable to preferred provider benefit plans. (i) A person enrolled in a preferred provider benefit plan may obtain covered health care services from a provider who does not participate in the plan. In accordance with rules adopted by the Commissioner and subject to G.S. 58-3-200(d), the preferred provider benefit plan may limit coverage for health care services obtained from a nonparticipating provider. The Commissioner shall adopt rules on product limitations, including payment differentials for services rendered by nonparticipating providers. These rules shall be similar in substance to rules governing HMO point-of-service products. (j) A list of the current participating providers in the geographic area in which a substantial portion of health care services will be available shall be provided to insureds and contracting parties. The list shall include participating physician assistants and their supervising physician. (k) Publications or advertisements of preferred provider benefit plans or organizations shall not refer to the quality or efficiency of the services of nonparticipating providers. (1997-443, s. 11A.122; 1997-519, s. 3.1; 1998-211, s. 2; 1999-210, s. 3; 2001-297, s. 3; 2001-334, s. 2.1.) Link to NORTH CAROLINA GENERAL STATUTES Link to NORTH CAROLINA ADMINISTRATIVE RULES Managed Care Annual Filing Training Manual 3.2013 Page 5 One of the primary missions of the North Carolina Department of Insurance is to serve and protect the insurance consumer. The managed care annual filing process is one way the Department can evaluate and determine if the Insurer, and/or its Delegated Entity(s)/Intermediary(s) are fully complying with the applicable regulations referenced in the Certifications and Data Grids. This manual is not inclusive of all Statutes and Administrative Codes the Insurer and its Delegated Entity(s)/Intermediary(s) must comply with; therefore, it is not a Compliance manual. The NC Managed Care Annual Filing manual is a detailed step-bystep guide on how to complete the Certifications and Data Grids. Managed Care Annual Filing Training Manual 3.2013 Page 6 2. INTRODUCTION TO THE MANAGED CARE ANNUAL FILING PROCESS Throughout the manual, the terms “Plan”, “Company”, “Insurer” and “Carrier” refer to the licensed HMO or Insurer responsible for the filing. The filing must be submitted electronically to the Department’s mailbox at managed.care.annual.filing@ncdoi.gov on or before the deadline of May 1st of each year by 5:00 p.m. EDT, or the next business day if May 1st falls on a Saturday, Sunday or Holiday. The managed care annual filing forms can be downloaded from the Department’s website: http://www.ncdoi.com/MR/MR_MC_Annual_Requirements.aspx. Each year, the Department will send notification to the last company contact on record when the forms for the upcoming data year submission have been posted to the website and are ready for use. Data cannot be in zip files or encrypted when submitting to the Department. The Checklist, Overall Attestation and Certifications must be sent in MS Word or .pdf files. Data must be submitted in the required .xls format (or .xlsx Office 2007). If the Insurer submits the annual filing via secured email and the time available to open the email is limited, the Insurer must include the wording “TIME SENSITIVE” in the subject line. This will ensure the Insurer’s filing is properly downloaded. If the Department encounters problems with opening/saving the information submitted via secured email then resubmission of the information in another format may be required. When submitting data with “password protection”, the Insurer must include the password that will enable the Department access. The Insurer is reminded that certain data is publicized on the Department’s website for NC consumers to review and compare Insurers. A complete filing must contain the applicable Certifications, Plan Data Grids and Delegated Entity Data Grids for each Delegated Entity and/or Intermediary. An outline of the actual files required for submission can be found on page 2, FILES NEEDED, of the Domestic/Foreign Instructions for the specified data year. It is important to note that late, incomplete and/or non-compliant filings may be subject to a monetary penalty or further regulatory action as outlined in NCGS 58-2-70. Late filings will require a written explanation on the Insurer’s letterhead signed/dated by the company’s President at the time of submission. To minimize the number of issues identified during the Department’s initial review requiring additional action, the Insurer must read the instructions carefully and thoroughly review the filing (including Delegated Data Grids received from a Delegated Entity and/or Intermediary) for completeness and accuracy, prior to submitting it to the Department. As the Department compares the current filing with the previous filing(s), the Insurer must also perform such a review and address any conflicting information, significant changes, etc. Managed Care Annual Filing Training Manual 3.2013 Page 7 If the previous data year’s filing was closed as “Accepted with Issues” or “Noncompliant”, the Insurer must address the ongoing, outstanding issue(s) outlined in the Department’s closure letter including the submission of any requested information. Unresolved/unanswered issues, failing to implement corrective action, or compliance issues impacting North Carolina insureds, may result in a market inquiry, market conduct examination and/or administrative penalty. Do not attach copies of Policies & Procedures (P&Ps) unless requested by the Department. For Foreign Insurers copies of P&Ps, when applicable, must be submitted as evidence of corrective action planned/taken when an area of non-compliance was identified. If the Department’s Market Regulation Division (MRD) has performed a market conduct examination within the past year, the Insurer must discuss and review the filing with the Insurer’s exam coordinator, to ensure that information submitted in the annual filing is consistent with information furnished during the examination. 2.1. EXEMPTIONS: If an Insurer believes its company should be exempt from submitting an annual filing, a request for exemption must be received by the Department on or before March 15th of each year by 5:00 p.m. EDT. A request must be submitted on the Insurer’s letterhead outlining the reason(s) for the exemption. The exemption request must be dated and signed by an officer of the company. Exemption requests are reviewed by the Department and are not automatically granted. The Insurer must provide sufficient detail to support the exemption. The request must be sent to the attention of the company’s assigned Market Analyst either Cheryl Allen-Bivens via email cheryl.allen-bivens@ncdoi.gov or Donna Tucker via email donna.tucker@ncdoi.gov. An exemption request is only valid for the specified data year. An exemption request must be submitted for each applicable data year. An exemption request is necessary when the Insurer is not actively marketing in North Carolina and has no NC managed care membership. However, if the Insurer has submitted an official market exit notification to the Life & Health Division and it has been acknowledged, an exemption request is not required, as long as, the withdrawal did not take place during the specified data year. If the market withdrawal took place during the specified data year contact the company’s assigned Market Analyst for instructions on completing the annual filing. 2.2. ABBREVIATED FILINGS: HMO/PPO Insurers new to the NC managed care market and submitting the initial managed care annual filing, Insurers withdrawing or officially exiting from the NC managed care market with less than 3 months of data should contact the company’s assigned Market Analyst for instructions on completing an abbreviated filing. Managed Care Annual Filing Training Manual 3.2013 Page 8 2.3. FORMS: Be sure to download and complete the correct forms (Domestic, Foreign → Full Service, Single Service) and data grids (Plan, Delegated Entity → Full Service, Single Service) for the specified data year. If the incorrect forms are used, the Department will be unable to begin the review process until the completed, corrected forms are received. The “receipt date” of the Insurer’s filing will be the date when the Department receives the completed, corrected forms. Remember, the Insurer may be subject to further regulatory action for late, incomplete and noncompliant filings. Separate submissions/filings are required for HMO and PPOs, and by product (medical, dental, vision). The Insurer must file information/data on any Delegated Entity/Intermediary even if the executed contract has not been filed and/or approved by the Life & Health Division. North Carolina Domestic Insurers, and Foreign Insurers that are utilizing their North Carolina domestic HMO or PPO affiliate for the provider network must use the Domestic Instructions. Foreign Insurers that do not have and/or do not utilize their North Carolina Domestic HMO or PPO affiliate for the provider network must use the Foreign Instructions. An affiliate, is defined as a related company through common ownership, also referred to as a "sister company". Affiliate, in this situation, does not refer to a delegated entity or network intermediary where the relationship is merely contractual. When using an attachment, the Insurer must properly label the document in the email submission and add a reference in the applicable Certification and/or Data Grid. 2.4. RIDERS: Benefits offered under a rider to all NC insureds must complete/submit all related Certifications and Data Grids. Riders not offered to all NC insureds under the Benefit Plan will not require the completion of Certifications and Data Grids. A statement certifying how the rider is marketed (all NC insureds or limited offering) will be required for the Department’s records upon the Life & Health Division’s approval of the Initial Operations and/or Intermediary Network Addition filing. If at any time the Insurer changes the marketing strategy of a restricted rider (limited offering), prompt notification must be sent to the company’s assigned Market Analyst. The Insurer will be required to complete/submit all related Certifications and Data Grids in the upcoming or subsequent annual filing depending on the effective date the (revised) rider was offered to all NC members. Managed Care Annual Filing Training Manual 3.2013 Page 9 2.5. ADDITION OR REPLACEMENT OF AN INTERMEDIARY/NEW PRODUCT LINE: Insurers that have never filed or an existing Insurer that added/replaced an Intermediary or added an additional network from a previously approved Intermediary (Intermediary offers more than one network) must complete the, “InitialFilers&NewIntermediaryForm”, Supplemental Checklist for the specified data year. This document must also be completed by Insurers that have had a Full Service or Single Service PPO product approved prior to the specified data year and had a new/or additional product line/rider (i.e. Dental or Vision) approved during the specified data year. When there has been a change in functions delegated from the previous data year, the Insurer must provide the following to the Department at the time of the annual filing submission for the current data year: 1) a letter explaining the change, and the reason for change and 2) if applicable, a copy of the SERFF filing approval from Life & Health Division. 2.6. REVIEW PROCESS: If no deficiencies and/or areas of concerns are identified during the Market Regulation Division’s (MRD) initial review of the Insurer’s annual filing, the Insurer will receive an “Accepted” closure letter. If deficiencies are identified (i.e. failure to meet all provider availability/accessibility standards or filing late) after the Market Regulation Division’s (MRD) initial review of the Insurer’s filing requiring no further action, the Insurer will receive an “Accepted with Issues” closure letter along with the Attachment outlining deficiencies found. If deficiencies and/or areas of concerns are identified during the Market Regulation Division’s (MRD) initial review of the Insurer’s annual filing requiring further action, the Insurer will receive an unacceptable letter along with an attachment outlining the initial findings. Within 30 days of receiving this letter, the Insurer is required to provide a response to MRD, including the completion of the “Company’s Response” column in the Attachment and submit any revised Certification/Data Grid to replace those initially submitted. The Attachment must be submitted in Word format (not .pdf). The Insurer must address all issues in the “Department’s Initial Findings” column. The filing will automatically close as “Non-compliant” if no response is received within the required 30 days, and the Insurer will be cited 11 NCAC 1.0602 for failure to respond to the Department’s request, along with any other violations found during the initial review. For timely responses, MRD will review the Insurer’s response and (if applicable) revised Certification(s)/Data Grid(s), then send final notification of its final action of each issue along with the “Accepted with Issues” or “Noncompliant” closure letter. “Accepted with Issues” and “Non-Compliant” closure letters will require signed acknowledgement from the company’s President attesting to knowledge of the deficiencies identified in the specified data year annual filing. Managed Care Annual Filing Training Manual 3.2013 Page 10 Due to the importance of timely communication during the annual filing process, all correspondence are sent via email with the tracking option of “Request a read receipt for this message”. The Insurer must send a “Read Receipt” or send a response acknowledging the receipt of the email. This ensures to the Department that the Insurer has received the correspondence. Managed Care Annual Filing Training Manual 3.2013 Page 11 3. INTRODUCTION TO THE CERTIFICATIONS NOTE: The Checklist, Overall Attestation and Certifications must be completed and submitted by the Insurer. There are two types of Certifications: Non-Delegated Certifications are used when the Plan itself performs the activity, and Delegated Certifications are used when a Delegated Entity or Intermediary performs the activity. A Delegated Entity includes a parent company, affiliated (sister) companies, etc. where the activity has been designated through a Management Service Agreement. If the Annual Filing Checklist indicates a Certification is “N/A”, skip the Certification or do not include the Certification in the submission. Separate Certifications must be completed for each Delegated Entity and Intermediary. Insurers cannot submit combined Certifications for HMO and PPO products. HMOs with a POS product must submit a combined Certification. Note that, if there are separate Policies & Procedures (P&Ps) for the HMO and POS benefit plans, the Insurer must provide information on both. The Department understands that there may be corporate Policies and Procedures (P&Ps) applicable across affiliated companies and related products; however, the Insurer must track and report separate audit (review activity) findings by entity/product (HMO/PPO) for its NC insureds. Remember, while the Insurer may have “internal” targets (less than 100%) for measurements related to Grievance and Utilization Review activity, for annual filing purposes the Insurer must report any area falling below 100% as an area of non-compliance. Managed Care Annual Filing Training Manual 3.2013 Page 12 4. C1. COMPLIANCE CERTIFICATION: ANNUAL FILING CHECKLIST Only one Checklist needs to be completed. Do not complete a Checklist for each Delegated Entity/Intermediary. The Checklist must be completed by the Insurer, identifying the functions and forms applicable to the Insurer’s benefit plan: Each Item must be checked “Included” or “N/A”. Skip over or do not submit any Certifications indicated as “N/A”. Do not complete any data grids indicated as “N/A”. If Items C4a/C4b, C6a/C6b and C9 are applicable, the Delegated Entity(s) must be listed. For Items C3 through C9: If checked “N/A”, an explanation must be provided in the far-right column entitled “Plan Comments”. For Items D1 through D18, any explanation(s) must be provided in the Comment Boxes located below each data grid. Delegated Entity(s)/Intermediary(s) listed on the Checklist must be consistent with the Certifications, submitted Delegated Entity Data Grids, and Plan data grid D18. 4.1. INITIAL FILERS & NEW INTERMEDIARY FORM (SUPPLEMENTAL CHECKLIST) This form must be completed when 1) the Insurer is a new filer, 2) the Insurer is replacing or adding an Intermediary, 3) the Insurer added a new product/rider or 4) the Insurer is adding a network option with a previously approved Intermediary (Intermediary offers more than one network). The Checklist must be completed by the Insurer. Each Item must be checked “No Changes” or “Revised Policy”. If the “No Change” box is checked, the Insurer must submit a Certification stating no changes have been made since approval of the Initial Operations or Intermediary Network Addition Filing, and also include a copy of the SERFF approval from our Life & Health Division. The Certification must be signed/dated by a Company officer and must address all the applicable Item numbers. The “No Change” check box is NOT a substitution for the Certification. If the “Revised Policy” box is checked, the Insurer must submit both a clean copy and a red-lined copy of the policy showing the changes made (additions/deletions). Managed Care Annual Filing Training Manual 3.2013 Page 13 5. C2. COMPLIANCE CERTIFICATION: OVERALL ATTESTATION With this form the Insurer attests that it reviewed the entire annual filing including information applicable to any Delegated Entity and/or Intermediary, and ALL the information is true and accurate. The officers are also certifying that ALL outstanding issues from the previous data year’s filing have been appropriately addressed. Lastly, the officers are acknowledging that late, incomplete and/or non-compliant filings may be subject to a monetary penalty and/or further regulatory action as outlined in NCGS 58-2-70. An Overall Attestation is required at the time of initial submission of the annual filing, as well as, resubmission of any revised Certification and/or Data Grid. If the same officers are not used to attest to the revised information/data, an explanation must be provided. The overall attestation must be signed/dated by two officers of the company. Managers and Supervisors may complete the attestation if their positions/titles are considered officers in accordance with the Insurer’s bylaws. If an Insurer has officers in different locations, separate executed attestations from each officer are acceptable. Attestations with electronic signatures are accepted, or the company may obtain original signatures and scan the document. The signatures and dates must be legible. The Insurer must provide the primary contact and backup contact information for the persons submitting the filing on behalf on the Insurer. If the person submitting the filing is a consultant (not an employee of the Insurer) then information on a company contact must be provided as the backup contact. Valid email addresses, and working direct and toll-free telephone numbers including extensions must be provided. Prompt notification of changes in company contacts and/or contact information must be sent to the company’s assigned Market Analyst either Cheryl Allen-Bivens cheryl.allenbivens@ncdoi.gov or Donna Tucker donna.tucker@ncdoi.gov. Failure to do so may significantly delay the Insurer receiving timely communications from the Department. NOTE: Filing false information to the Department may subject the Insurer to be cited for noncompliance with 11 NCAC 1.1602 and NCGS 58-2-180. Managed Care Annual Filing Training Manual 3.2013 Page 14 6. C3A. COMPLIANCE CERTIFICATION: GRIEVANCE PROCEDURES / C3B. COMPLIANCE CERTIFICATION: EXTERNAL REVIEW RELATED TO GRIEVANCES (Not applicable to single service plans) NCGS 58-50-61. Utilization review. (a) Definitions. – As used in this section, in G.S. 58-50-62, and in Part 4 of this Article, the term: (6) "Grievance" means a written complaint submitted by a covered person about any of the following: a. An insurer's decisions, policies, or actions related to availability, delivery, or quality of health care services. A written complaint submitted by a covered person about a decision rendered solely on the basis that the health benefit plan contains a benefits exclusion for the health care service in question is not a grievance if the exclusion of the specific service requested is clearly stated in the certificate of coverage. b. Claims payment or handling; or reimbursement for services. c. The contractual relationship between a covered person and an insurer. d. The outcome of an appeal of a noncertification under this section. This Certification must be completed by the Insurer when Grievance and/or External Review related to Grievance are performed internally by the Insurer during any part of the specified data year. IMPORTANT NOTE: THE INSURER MUST ANSWER EACH QUESTION APPLICABLE TO THE SPECIFED DATA YEAR. A response to all questions must be provided. If the response is “N/A” an explanation must also be provided. Enter the name of the Insurer on the first page of the C3a and, if applicable, C3b, Certification. Check all type(s) of Grievances offered for services provided to North Carolina insureds, regardless of whether that type of review was conducted during the specified data year. The type(s) of grievances checked in the Certification must match those checked in the Plan’s data grid D3. Check all type(s) of Grievance notifications developed and sent by the Plan to North Carolina insureds. Managed Care Annual Filing Training Manual 3.2013 Page 15 In regards to External Review related to Grievances, the Insurer is ensuring covered persons were provided with notice of their rights as required by Statute. Question 1: The Insurer must identify its own Grievance P&Ps, including related form/template letters, effective during the specified data year. The Insurer must provide the following: Name of Insurer’s Grievance P&Ps, including any identification number/revision date* Specify Board of Directors, Committee or Name/Title of the Company Officer(s) that approved the Insurer’s Grievance P&Ps Date Insurer’s Grievance P&Ps approved by Board of Directors, Committee or Company Officer(s) Effective Date of Insurer’s Grievance P&Ps The Insurer must have in place formalized written Grievance P&Ps for receiving and resolving grievances from covered persons in accordance with State law for each version**. The actual P&Ps must contain either an approval signature/date or the Insurer must be able to provide evidence of the P&Ps’ approval via (committee) meeting minutes. These P&Ps are not those found in the Insurer’s approved policies/certificates but the internal P&Ps provided to the Insurer’s Grievance Department. All P&Ps must include an effective date to demonstrate when the process or revised process was initiated or implemented. The P&Ps must include a description of the internal audit mechanism and the frequency of the Insurer’s review of the Grievance P&Ps, Grievance form/template letters and actual Grievance case letters. *If any revisions were made to the P&Ps from the previous data year, the Insurer must briefly describe the changes. Do not attach copies of the actual revised P&Ps unless requested by the Department. **The Insurer must maintain all P&Ps and all other required information as stated above for each version in accordance with NC State law for record retention; 11 NCAC 19.0102. Question 2: The Insurer must state whether each of the following programs is included in the Grievance P&Ps identified in Question/Answer #1: Mental Health/Chemical Dependency, Pharmacy Benefit. If not, the Insurer must provide the same information identified in Question/Answer #1 for each of the programs. Managed Care Annual Filing Training Manual 3.2013 Page 16 IMPORTANT NOTES PERTAINING TO QUESTIONS #3, #4, #5 AND #6, CONCERNING REVIEW ACTIVITIES: If the review date specified is outside of the specified data year, an explanation MUST be provided (i.e. review was retroactive). For example, if the review date was April 2013, the Insurer must explain whether this review was applicable for data year 2012 or 2013. It is the Department’s position that the Insurer must be conducting annual reviews. The most recent review date will be compared to last year’s most recent review date to confirm that an annual review was conducted (within the rolling 12 months from the last review). If not, the Insurer MUST provide an explanation. The Insurer must provide an explanation for any change in dates or gaps from the date listed in last year’s filing for “next anticipated review”, or if the review is overdue (more than 12 months from the last review). Reviews and Accreditations done by agencies such as NCQA, URAC, etc. do not replace the Insurer’s statutory requirements to monitor performance. The review activities can be performed by external sources; however, it must meet all NC statutory and regulatory requirements. The Insurer must disclose the identity of the external source. Question 3: The Insurer must specify the date (month/year) of the most recent review during the specified data year of its Grievance P&Ps. Question 4: The Insurer must specify the date (month/year) of the next anticipated review of its Grievance P&Ps. Question 5: The Insurer must specify the date (month/year) of the most recent review during the specified data year of its Grievance related form/template letters as required by Statutes. Question 6: The Insurer must specify the date (month/year) of the most recent audit sampling of its Grievance actual case correspondence (notification letters required by Statutes). Managed Care Annual Filing Training Manual 3.2013 Page 17 Question 7: The Insurer must specify the number of Grievance cases reviewed. A case involves all notifications required by Statute for each level of review (see Certifications for statutory references). Question 8: The Insurer must provide its rationale for determining the number of Grievance cases reviewed as indicated in Question/Answer #7. The Insurer must be able to justify the number of cases reviewed. The sampling must be a fair representation of all grievances reported in the Plan’s data grid D3 for the specified data year. IMPORTANT NOTES PERTAINING TO QUESTIONS #9 AND #10 CONCERNING CORRECTIVE ACTION PLAN REQUIREMENTS: Domestic Insurers are required to document in the Certification the corrective action taken and/or planned including the implementation date(s). Foreign Insurers, if deficiencies were found in either the prior or current year’s filing, the Insurer is required to provide evidence demonstrating actual implementation of the corrective action plan. Evidence can be in the form of Committee Meeting Minutes, revised P&Ps, etc. The evidence must contain a (revision) date, as well as, the entity/committee/officer approving the revision. Simply indicating that internal procedures have been revised is inadequate. Due to constraints with the 30 days response time, if a deficiency is found in the current year’s filing and the Insurer is unable to actually implement corrective action, the Insurer must submit a Corrective Action Plan, including a schedule of implementation to resolve the deficiencies. The Insurer must ensure it or its Delegated Entity/Intermediary is taking timely action to correct deficiencies, and taking the appropriate action when either party has not. Question 9: The Insurer must state whether all the Grievance case correspondence reviewed were compliant (language and time requirements) with State law and did they include External Review Rights when required. The Insurer MUST explain any deficiencies found, along with corrective actions taken and/or planned. If an entity (i.e. Insurer or Intermediary) which does not perform the Grievance activity receives a written grievance from a member, then forwards it on to the proper entity performing Grievance activity the statutory time requirements begin when the first entity received the Grievance from the member (not the date when the entity which performs Grievance activity received it from the non-Grievance activity entity). Managed Care Annual Filing Training Manual 3.2013 Page 18 Question 10: The Insurer must detail any areas of non-compliance identified during the reviews of the Grievance P&Ps and form/template letters. The Insurer MUST explain any deficiencies found, along with corrective actions taken and/or planned. Managed Care Annual Filing Training Manual 3.2013 Page 19 7. C4A. COMPLIANCE CERTIFICATION: DELEGATED GRIEVANCE PROCEDURES / C4B. COMPLIANCE CERTIFICATION: DELEGATED EXTERNAL REVIEW RELATED TO GRIEVANCES (Not applicable to single service plans) NCGS 58-50-61. Utilization review. (a) Definitions. – As used in this section, in G.S. 58-50-62, and in Part 4 of this Article, the term: (6) "Grievance" means a written complaint submitted by a covered person about any of the following: a. An insurer's decisions, policies, or actions related to availability, delivery, or quality of health care services. A written complaint submitted by a covered person about a decision rendered solely on the basis that the health benefit plan contains a benefits exclusion for the health care service in question is not a grievance if the exclusion of the specific service requested is clearly stated in the certificate of coverage. b. Claims payment or handling; or reimbursement for services. c. The contractual relationship between a covered person and an insurer. d. The outcome of an appeal of a noncertification under this section. This certification must be completed by the Insurer when it delegated Grievances and/or External Review related to Grievances during any part of the specified data year. A certification is needed for each entity to which Grievance and/or External Review related to Grievances was delegated (“Delegated Entity”). Each Delegated Entity must be listed under Item #C4a/C4b on the C1. Annual Filing Checklist and listed on the Plan’s data grid D18 with “Grievance” activity checked. Each Delegated Grievance Entity must complete the delegated data grid D3. Grievances and/or External Review related to Grievances activity can be delegated to an intermediary organization, Utilization Review Organization and/or other subcontracted companies with which the Insurer has entered into a Management/Service Agreement. IMPORTANT NOTE: THE INSURER MUST ANSWER EACH QUESTION APPLICABLE TO THE SPECIFED DATA YEAR. A response to all questions must be provided. If the response is “N/A” an explanation must also be provided. Enter the name of the Insurer and Delegated Entity on the first page of the C4a and, if applicable, C4b Certification. Managed Care Annual Filing Training Manual 3.2013 Page 20 Enter the name of the Delegated Entity on Part ll. Monitoring Activities of the Certification. Check all type(s) of Grievances contracted by the Delegated Entity for services provided to North Carolina insureds, regardless of whether that type of review was conducted during the specified data year. The type(s) of Grievances checked in the Certification must match those checked in the Delegated Entity’s data grid D3. Check all type(s) of Grievance notifications developed and sent by the Delegated Entity to North Carolina insureds. In reporting External Review related to Grievances, the Insurer is ensuring covered persons were provided with notice of their rights as required by Statute. Question 1: The Insurer must identify the Delegated Entity’s Grievance P&Ps, including related form/template letters, effective during the specified data year. The Insurer must provide the following: Name of Delegated Entity’s Grievance P&Ps including any identification number/revision date* Date Delegated Entity’s Grievance P&Ps approved internally by the Delegated Entity Specify Board of Directors, Committee or Name/Title of the Company Officer from the Delegated Entity that approved the Grievance P&Ps Effective Date of Delegated Entity’s Grievance P&Ps Specify Board of Directors, Committee or Name/Title of the Company Officer from the Insurer that approved the Delegated Entity’s Grievance P&Ps Date Insurer’s Board of Directors, Committee or Company Officer(s) approved Delegated Entity’s Grievance P&Ps The Delegated Entity must have in place formalized written Grievance P&Ps for receiving and resolving grievances from covered persons in accordance with State law for each version**. The actual P&Ps must contain either an approval signature/date or the Insurer must be able to provide evidence of the Delegated Entity’s approval of its Grievance P&Ps via (committee) meeting minutes. These P&Ps are not those found in the Insurer’s approved policies/certificates but the internal P&Ps provided to the Delegated Entity’s Grievance Department. All P&Ps must include an effective date to demonstrate when the process or revised process was initiated or implemented. *If any revisions were made to the P&Ps from the previous data year, the Insurer must briefly describe the changes. Do not attach copies of the actual revised P&Ps unless requested by the Department. Managed Care Annual Filing Training Manual 3.2013 Page 21 **The Insurer must maintain and must ensure the delegated entity maintains, all P&Ps and all other required information for each version (as stated above) in accordance with NC State law for record retention; 11 NCAC 19.0102. **The Insurer must maintain evidence of review and approval for each version of the Delegated Entity’s P&Ps and all other required information, in accordance with NC State law for record retention; 11 NCAC 19.0102. Question 2: The Insurer must state whether each of the following programs is included in the Delegated Entity’s Grievance P&Ps identified in Question/Answer #1: Mental Health/Chemical Dependency, Pharmacy Benefit. If not, the Insurer must provide the same information identified in Question/Answer #1 for each of the programs. Question 3: The Insurer must identify its internal P&Ps for oversight of the Delegated Entity’s Grievance program effective during the specified data year by providing the following: Name of Insurer’s Grievance Oversight P&Ps, including identification number/revision date* Specify Board of Directors, Committee or Name/Title of the Company Officer(s) that approved the Grievance Oversight P&Ps. Date Insurer’s Grievance Oversight P&Ps approved by Board of Directors, Committee or Company Officer(s) Effective Date of the Insurer’s Grievance Oversight P&Ps The Insurer must have in place formalized written P&Ps for oversight of the Delegated Entity’s Grievance program for each version**. The actual P&Ps must contain either an approval signature/date or the Insurer must able to provide evidence of the Grievance Oversight P&Ps approval via (committee) meeting minutes. All P&Ps must include an effective date to demonstrate when the process or revised process was initiated or implemented. The P&Ps must include a description of the internal audit mechanism and the frequency of the Insurer’s review of the Delegated Entity’s Grievance P&Ps, Grievance form/template letters and actual Grievance case letters. *If any revisions were made to the P&Ps from the previous data year, the Insurer must briefly describe the changes. Do not attach copies of the actual revised P&Ps unless requested by the Department. **The Insurer must maintain all P&Ps and all other required information as stated above for each version in accordance with NC State law for record retention; 11 NCAC 19.0102. Managed Care Annual Filing Training Manual 3.2013 Page 22 Question 4: The Insurer must state whether each of the following programs is included in their oversight P&Ps for the Delegated Entity’s Grievance P&Ps identified in Question/Answer #3: Mental Health/Chemical Dependency, Pharmacy Benefit. If not, the Insurer must provide the same information identified in Question/Answer #3 for each of the programs. IMPORTANT NOTES PERTAINING TO QUESTIONS #5, #6, #7 AND #8, CONCERNING REVIEW ACTIVITIES: If the review date specified is outside of the specified data year, an explanation MUST be provided (i.e. review was retroactive). For example, if the review date was April 2013, the Insurer must explain whether this review was applicable for data year 2012 or 2013. It is the Department’s position that the Insurer must be conducting annual reviews. The most recent review date will be compared to last year’s most recent review date to confirm that an annual review was conducted (within the rolling 12 months from the last review). If not, the Insurer MUST provide an explanation. The Insurer must provide an explanation for any change in dates or gaps from the date listed in last year’s filing for “next anticipated review”, or if the review is overdue (more than 12 months after the last review). Reviews and Accreditations done by agencies such as NCQA, URAC, etc. do not replace the Insurer’s statutory requirements to monitor performance. The review activities can be performed by external sources; however, it must meet all NC statutory and regulatory requirements. The Insurer must disclose the identity of the external source. Question 5: The Insurer must specify the date (month/year) of its most recent review during the specified data year of the Delegated Entity’s Grievance P&Ps. Question 6: The Insurer must specify the date (month/year) of its next anticipated review of the Delegated Entity’s Grievance P&Ps. Question 7: The Insurer must specify the date (month/year) of its most recent review during the specified data year of the Delegated Entity’s Grievance related form/template letters as required by Statutes. Managed Care Annual Filing Training Manual 3.2013 Page 23 Question 8: The Insurer must specify the date (month/year) of its most recent audit sampling of the Delegated Entity’s Grievance actual case correspondence (notification letters required by Statutes). Question 9: The Insurer must specify the number of the Delegated Entity’s Grievance cases reviewed. A case involves all notifications required by Statute for each level of review (see Certifications for statutory requirements). Question 10: The Insurer must provide its rationale for determining the number of Grievance cases of the Delegated Entity reviewed as indicated in Question/Answer #9. The Insurer must be able to justify the number of cases reviewed. The sampling must be a fair representation of all grievance reported in the Delegated Entity’s data grid D3 for the specified data year. IMPORTANT NOTES PERTAINING TO QUESTIONS #11 AND #12 CONCERNING CORRECTIVE ACTION PLAN REQUIREMENTS: Domestic Insurers are required to document in the Certification the corrective action taken including the implementation date(s). Foreign Insurers, if deficiencies were found in either the prior or current year’s filing, the Insurer is required to provide evidence demonstrating actual implementation of the corrective action plan. Evidence can be in the form of Committee Meeting Minutes, revised P&Ps, etc. The evidence must contain a (revision) date, as well as, the entity/committee/officer approving the revision. Simply indicating that internal procedures have been revised is inadequate. Due to constraints with the 30 days response time, if a deficiency is found in the current year’s filing and the Insurer is unable to actually implement corrective action, the Insurer must submit a Corrective Action Plan, including a schedule of implementation to resolve the deficiencies. The Insurer must ensure it or its Delegated Entity/Intermediary is taking timely action to correct deficiencies, and taking the appropriate action when either party has not. Question 11: The Insurer must state whether all the Delegated Entity’s Grievance case correspondence reviewed were compliant (language and time requirements) with State law and included External Review Rights when required. The Insurer MUST explain any deficiencies found, along with corrective actions taken and/or planned. Managed Care Annual Filing Training Manual 3.2013 Page 24 If an entity (i.e. Insurer or Intermediary) which does not perform the Grievance activity receives a written grievance from a member, then forwards it on to the proper entity performing Grievance activity the statutory time requirements begin when the first entity received the Grievance from the member (not the date when the entity which performs Grievance activity received it from the non-Grievance activity entity). Question 12: The Insurer must detail any areas of non-compliance identified during its reviews of the Delegated Entity’s Grievance P&Ps and form/template letters. The Insurer MUST explain any deficiencies found, along with corrective actions taken and/or planned. Managed Care Annual Filing Training Manual 3.2013 Page 25 8. C5A. COMPLIANCE CERTIFICATION: UTILIZATION REVIEW / C5B. COMPLIANCE CERTIFICATION: EXTERNAL REVIEW RELATED TO UTILIZATION REVIEW (Not applicable to single service plans) NCGS 58-50-61. Utilization review. (a) Definitions. – As used in this section, in G.S. 58-50-62, and in Part 4 of this Article, the term: (13) "Noncertification" means a determination by an insurer or its designated utilization review organization that an admission, availability of care, continued stay, or other health care service has been reviewed and, based upon the information provided, does not meet the insurer's requirements for medical necessity, appropriateness, health care setting, level of care or effectiveness, or does not meet the prudent layperson standard for coverage of emergency services in G.S. 58-3-190, and the requested service is therefore denied, reduced, or terminated. A "noncertification" is not a decision rendered solely on the basis that the health benefit plan does not provide benefits for the health care service in question, if the exclusion of the specific service requested is clearly stated in the certificate of coverage. A "noncertification" includes any situation in which an insurer or its designated agent makes a decision about a covered person's condition to determine whether a requested treatment is experimental, investigational, or cosmetic, and the extent of coverage under the health benefit plan is affected by that decision. (17) "Utilization review" means a set of formal techniques designed to monitor the use of or evaluate the clinical necessity, appropriateness, efficacy or efficiency of health care services, procedures, providers, or facilities. These techniques may include: a. Ambulatory review. – Utilization review of services performed or provided in an outpatient setting. b. Case management. – A coordinated set of activities conducted for individual patient management of serious, complicated, protracted, or other health conditions. c. Certification. – A determination by an insurer or its designated URO that an admission, availability of care, continued stay, or other service has been reviewed and, based on the information provided, satisfies the insurer's requirements for medically necessary services and supplies, appropriateness, health care setting, level of care, and effectiveness. d. Concurrent review. – Utilization review conducted during a patient's hospital stay or course of treatment. Managed Care Annual Filing Training Manual 3.2013 Page 26 Discharge planning. – The formal process for determining, before discharge from a provider facility, the coordination and management of the care that a patient receives after discharge from a provider facility. f. Prospective review. – Utilization review conducted before an admission or a course of treatment including any required preauthorization or precertification. g. Retrospective review. – Utilization review of medically necessary services and supplies that is conducted after services have been provided to a patient, but not the review of a claim that is limited to an evaluation of reimbursement levels, veracity of documentation, accuracy of coding, or adjudication for payment. Retrospective review includes the review of claims for emergency services to determine whether the prudent layperson standard in G.S. 58-3-190 has been met. h. Second opinion. – An opportunity or requirement to obtain a clinical evaluation by a provider other than the provider originally making a recommendation for a proposed service to assess the clinical necessity and appropriateness of the proposed service. "Utilization review organization" or "URO" means an entity that conducts utilization review under a managed care plan, but does not mean an insurer performing utilization review for its own health benefit plan. e. (18) NCGS 58-3-200. Miscellaneous insurance and managed care coverage and network provisions. (b) Medical Necessity. – An insurer that limits its health benefit plan coverage to medically necessary services and supplies shall define "medically necessary services or supplies" in its health benefit plan as those covered services or supplies that are: (1) Provided for the diagnosis, treatment, cure, or relief of a health condition, illness, injury, or disease; and, except as allowed under G.S. 58-3-255, not for experimental, investigational, or cosmetic purposes. (2) Necessary for and appropriate to the diagnosis, treatment, cure, or relief of a health condition, illness, injury, disease, or its symptoms. (3) Within generally accepted standards of medical care in the community. (4) Not solely for the convenience of the insured, the insured's family, or the provider. For medically necessary services, nothing in this subsection precludes an insurer from comparing the cost-effectiveness of alternative services or supplies when determining which of the services or supplies will be covered. By definition, Utilization Review (UR) and Noncertification involve “medical necessity” determinations. Therefore, if the Insurer performs medical necessity determinations it must complete a C5a/(C5b if applicable) Certification and report the medical necessity determinations in the Plan’s Utilization Reviews data grids D4 and D5. This Certification must be completed by the Insurer when UR and/or External Review related to UR are performed internally by the Insurer during any part of the specified data year. Managed Care Annual Filing Training Manual 3.2013 Page 27 IMPORTANT NOTE: THE INSURER MUST ANSWER EACH QUESTION APPLICABLE TO THE SPECIFED DATA YEAR. A response to all questions must be provided. If the response is “N/A” an explanation must also be provided. Enter the name of the Insurer on the first page of the C5a and, if applicable, C5b Certification. Check all type(s) of Reviews offered for services provided to North Carolina insureds, regardless of whether that type of review was conducted during the specified data year. The type(s) of reviews checked in the Certification must match those checked in the Plan’s data grids D4 andD5. Check all type(s) of UR notifications developed and sent by the Plan to North Carolina insureds. Question 1: The Insurer must identify its own UR P&Ps, including related form/template letters, effective during the specified data year. The insurer must provide the following: Name of Insurer’s UR P&Ps including any identification number/revision date* Specify Board of Directors, Committee or Name/Title of the Company Officer(s) that approved the Insurer’s UR P&Ps Date Insurer’s UR P&Ps approved by Board of Directors, Committee or Company Officer(s) Effective Date of Insurer’s UR P&Ps The Insurer must have in place formalized written UR P&Ps for receiving and processing utilization reviews for covered persons in accordance with State law for each version**. The actual P&Ps must contain either an approval signature/date or the Insurer must be able to provide evidence of the P&Ps’ approval via (committee) meeting minutes. These P&Ps are not those found in the Insurer’s approved policies/certificates but the internal P&Ps provided to the Insurer’s UR Department. All P&Ps must include an effective date to demonstrate when the process or revised process was initiated or implemented. The P&Ps must include a description of the internal audit mechanism and the frequency of the Insurer’s review of the UR P&Ps, UR form/template letters and actual UR case letters. *If any revisions were made to the P&Ps from the previous data year, the Insurer must briefly describe the changes. Do not attach copies of the actual revised P&Ps unless requested by the Department. Managed Care Annual Filing Training Manual 3.2013 Page 28 **The Insurer must maintain all P&Ps and all other required information as stated above for each version in accordance with NC State law for record retention; 11 NCAC 19.0102. Question 2: The Insurer must state whether each of the following programs is included in the UR P&Ps identified in Question/Answer #1: Mental Health/Chemical Dependency, Pharmacy Benefit. If not, the Insurer must provide the same information identified in Question/Answer #1 for each of the programs. IMPORTANT NOTES PERTAINING TO QUESTIONS #3, #4, #5 AND #6, CONCERNING REVIEW ACTIVITIES: If the review date specified is outside of the specified data year, an explanation MUST be provided (i.e. review was retroactive). For example, if the review date was April 2013, the Insurer must explain whether this review was applicable for data year 2012 or 2013. It is the Department’s position that the Insurer must be conducting annual reviews. The most recent review date will be compared to last year’s most recent review date to confirm that an annual review was conducted (within the rolling 12 months from the last review). If not, the Insurer MUST provide an explanation. The Insurer must provide an explanation for any change in dates or gaps from the date listed in last year’s filing for “next anticipated review”, or if the review is overdue (more than 12 months after the last review). Reviews and Accreditations done by agencies such as NCQA, URAC, etc. do not replace the Insurer’s statutory requirements to monitor performance. The review activities can be performed by external sources; however, it must meet all NC statutory and regulatory requirements. The Insurer must disclose the identity of the external source. Question 3: The Insurer must specify the date (month/year) of the most recent review during the specified data year of its UR P&Ps. Question 4: The Insurer must specify the date (month/year) of the next anticipated review of its UR P&Ps. Question 5: The Insurer must specify the date (month/year) of the most recent review during the specified data year of its UR related form/template letters as required by Statutes. Managed Care Annual Filing Training Manual 3.2013 Page 29 Question 6: The Insurer must specify the date (month/year) of the most recent audit sampling of its UR actual case correspondence (notification letters required by Statutes). Question 7: The Insurer must specify the number of UR cases reviewed. A case involves all notifications required by Statute of each level of review (see Certification for statutory references). Question 8: The Insurer must provide its rationale for determining the number of UR cases reviewed as indicated in Question/Answer #7. The Insurer must be able to justify the number of cases reviewed. The sampling must be a fair representation of all Utilization Reviews reported in the Plan’s data grids D4 and D5 for the specified data year. IMPORTANT NOTES PERTAINING TO QUESTIONS #9 AND #10 CONCERNING CORRECTIVE ACTION PLAN REQUIREMENTS: Domestic Insurers are required to document in the Certification the corrective action taken including the implementation date. Foreign Insurers, if deficiencies were found in either the prior or current year’s filing, the Insurer is required to provide evidence demonstrating actual implementation of the corrective action plan. Evidence can be in the form of Committee Meeting Minutes, revised P&Ps, etc. The evidence must contain a (revision) date, as well as, the entity/committee/officer approving the revision. Simply indicating that internal procedures have been revised is inadequate. Due to constraints with the 30 days response time, if a deficiency is found in the current year’s filing and the Insurer is unable to actually implement corrective action, the Insurer must submit a Corrective Action Plan, including a schedule of implementation to resolve the deficiencies. The Insurer must ensure it or its Delegated Entity/Intermediary is taking timely action to correct deficiencies, and taking the appropriate action when either party has not. Question 9: The Insurer must state whether all the UR case correspondence reviewed were compliant (language and time requirements) with State law and included External Review Rights when required. The Insurer MUST explain any deficiencies found, along with corrective actions taken and/or planned. Managed Care Annual Filing Training Manual 3.2013 Page 30 Question 10: The Insurer must detail any areas of non-compliance identified during the reviews of the UR P&Ps and form/template letters. The Insurer MUST explain any deficiencies found, along with corrective actions taken and/or planned. Question 11: The Insurer must specify those staff member(s) who have ultimate oversight responsibilities for the UR Program, including their position titles and clinical degree(s). If more than one person is identified, the Insurer must clarify the duties for each. The Insurer must be able to demonstrate compliance with State law which requires that qualified health care professionals administer the Utilization Review Program and oversee review decisions under the direction of a medical doctor; NCGS 58-50-61(d). Question 12: The Insurer must specify those staff members who have ultimate operational (day-to-day management) responsibilities for the UR Program, including their position titles and clinical degree(s). If more than one person is identified, the Insurer must clarify the duties for each. The Insurer must be able to demonstrate compliance with State law which requires that qualified health care professionals administer the Utilization Review Program and oversee review decisions under the direction of a medical doctor; NCGS 58-50-61 (c)(8) and (d). Question 13: The Insurer must provide the name, clinical degree(s) and State(s) where the clinical degree(s)/license(s) are active and in good standing for those individuals making noncertification decisions. If the Insurer contracts with an Utilization Review Organization (URO) to perform this function, the name of URO must be identified, and a list of those individual(s) within the URO making noncertification decisions, along with their clinical degree(s) and State(s) where the clinical degree(s)/license(s) are active and in good standing must be provided. Important Note: If the URO reviews the case and directly sends notifications of its decisions to insureds, the URO is considered a Delegated Entity; therefore, a C6a Delegated Utilization Review and, if applicable, a C6b Delegated External Review Certification must be completed. State law requires a medical doctor licensed to practice medicine in North Carolina to evaluate the clinical appropriateness of noncertifications: NCGS 58-50-61(d). Managed Care Annual Filing Training Manual 3.2013 Page 31 9. C6A. COMPLIANCE CERTIFICATION: DELEGATED UTILIZATION REVIEW / C6B. COMPLIANCE CERTIFICATION: EXTERNAL REVIEW RELATED TO UTILIZATION REVIEW (Not applicable to single service plans) 58-50-61. Utilization review. (a) Definitions. – As used in this section, in G.S. 58-50-62, and in Part 4 of this Article, the term: (13) "Noncertification" means a determination by an insurer or its designated utilization review organization that an admission, availability of care, continued stay, or other health care service has been reviewed and, based upon the information provided, does not meet the insurer's requirements for medical necessity, appropriateness, health care setting, level of care or effectiveness, or does not meet the prudent layperson standard for coverage of emergency services in G.S. 58-3-190, and the requested service is therefore denied, reduced, or terminated. A "noncertification" is not a decision rendered solely on the basis that the health benefit plan does not provide benefits for the health care service in question, if the exclusion of the specific service requested is clearly stated in the certificate of coverage. A "noncertification" includes any situation in which an insurer or its designated agent makes a decision about a covered person's condition to determine whether a requested treatment is experimental, investigational, or cosmetic, and the extent of coverage under the health benefit plan is affected by that decision. (17) "Utilization review" means a set of formal techniques designed to monitor the use of or evaluate the clinical necessity, appropriateness, efficacy or efficiency of health care services, procedures, providers, or facilities. These techniques may include: a. Ambulatory review. – Utilization review of services performed or provided in an outpatient setting. b. Case management. – A coordinated set of activities conducted for individual patient management of serious, complicated, protracted, or other health conditions. c. Certification. – A determination by an insurer or its designated URO that an admission, availability of care, continued stay, or other service has been reviewed and, based on the information provided, satisfies the insurer's requirements for medically necessary services and supplies, appropriateness, health care setting, level of care, and effectiveness. d. Concurrent review. – Utilization review conducted during a patient's hospital stay or course of treatment. Managed Care Annual Filing Training Manual 3.2013 Page 32 Discharge planning. – The formal process for determining, before discharge from a provider facility, the coordination and management of the care that a patient receives after discharge from a provider facility. f. Prospective review. – Utilization review conducted before an admission or a course of treatment including any required preauthorization or precertification. g. Retrospective review. – Utilization review of medically necessary services and supplies that is conducted after services have been provided to a patient, but not the review of a claim that is limited to an evaluation of reimbursement levels, veracity of documentation, accuracy of coding, or adjudication for payment. Retrospective review includes the review of claims for emergency services to determine whether the prudent layperson standard in G.S. 58-3-190 has been met. h. Second opinion. – An opportunity or requirement to obtain a clinical evaluation by a provider other than the provider originally making a recommendation for a proposed service to assess the clinical necessity and appropriateness of the proposed service. "Utilization review organization" or "URO" means an entity that conducts utilization review under a managed care plan, but does not mean an insurer performing utilization review for its own health benefit plan. e. (18) NCGS 58-3-200. Miscellaneous insurance and managed care coverage and network provisions. (b) Medical Necessity. – An insurer that limits its health benefit plan coverage to medically necessary services and supplies shall define "medically necessary services or supplies" in its health benefit plan as those covered services or supplies that are: (1) Provided for the diagnosis, treatment, cure, or relief of a health condition, illness, injury, or disease; and, except as allowed under G.S. 58-3-255, not for experimental, investigational, or cosmetic purposes. (2) Necessary for and appropriate to the diagnosis, treatment, cure, or relief of a health condition, illness, injury, disease, or its symptoms. (3) Within generally accepted standards of medical care in the community. (4) Not solely for the convenience of the insured, the insured's family, or the provider. For medically necessary services, nothing in this subsection precludes an insurer from comparing the cost-effectiveness of alternative services or supplies when determining which of the services or supplies will be covered. By definition, Utilization Review (UR) and Noncertification involve “medical necessity” determinations. Therefore, if the Delegate Entity performs medical necessity determinations it must complete a C6a/(C6b if applicable) Certification and report the medical necessity determinations in the Delegated Entity’s Utilization Reviews data grids D4 and D5. Managed Care Annual Filing Training Manual 3.2013 Page 33 This certification must be completed by the Insurer when it delegated UR and/or External Review related to UR to a Delegated Entity during any part of the specified data year. A certification is needed for each entity to which UR and/or External Review was delegated (“Delegated Entity”). Each Delegated Entity must be listed under Item #C6a/C6b on the C1. Annual Filing Checklist, and listed on the Plan’s data grid D18 with the “Utilization Review” activity checked. Each Delegated Utilization Review and/or External Review Entity must complete the delegated data grids D4 and D5. Utilization Review and/or External Review related to UR can be delegated to an intermediary organization, Utilization Review Organization and/or other subcontracted companies with which the Insurer has entered into a Management/Service Agreement. IMPORTANT NOTE: THE INSURER MUST ANSWER EACH QUESTION APPLICABLE TO THE SPECIFED DATA YEAR. A response to all questions must be provided. If the response is “N/A” an explanation must also be provided. Enter the name of the Insurer and Delegated Entity on the first page of the C6a and, if applicable, C6b Certification. Enter the name of the Delegated Entity on Part ll. Monitoring Activities of the Certification. Check all type(s) of UR contracted by the Delegated Entity for services provided to North Carolina insureds regardless of whether that type of review was conducted during the specified data year. The type(s) of UR checked in the Certification must match those checked in the Delegated Entity’s data grids D4 and D5. Check all type(s) of UR notification(s) developed and sent by the Delegated Entity to North Carolina insureds. Question 1: The Insurer must identify the Delegated Entity’s UR P&Ps, including related form/template letters, effective during the specified data year. The Insurer must provide the following: Name of Delegated Entity’s UR P&Ps including any identification number/revision date* Date Delegated Entity’s UR P&Ps approved internally by the Delegated Entity Specify Board of Directors, Committee or Name/Title of the Company Officer from the Delegated Entity that approved the UR P&Ps Effective Date of Delegated Entity’s UR P&Ps Managed Care Annual Filing Training Manual 3.2013 Page 34 Specify Board of Directors, Committee or Name/Title of the Company Officer from the Insurer that approved the Delegated Entity’s UR P&Ps Date Insurer’s Board of Directors, Committee or Company Officer(s) approved Delegated Entity’s UR P&Ps The Delegated Entity must have in place formalized written UR P&Ps for receiving and processing utilization reviews for covered persons in accordance with State law for each version**. The actual P&Ps must contain either an approval signature/date or the Insurer must be able to provide evidence of the Delegated Entity’s approval of its UR P&Ps via (committee) meeting minutes. These P&Ps are not those found in the Insurer’s approved policies/certificates but the internal P&Ps provided to the Delegated Entity’s UR Department. All P&Ps must include an effective date to demonstrate when the process or revised process was initiated or implemented. *If any revisions were made to the P&Ps from the previous data year, the Insurer must briefly describe the changes. Do not attach copies of the actual revised P&Ps unless requested by the Department. **The Insurer must maintain and must ensure the delegated entity maintains, all P&Ps and all other required information for each version (as stated above) in accordance with NC State law for record retention; 11 NCAC 19.0102. **The Insurer must maintain evidence of review and approval for each version of the Delegated Entity’s P&Ps and all other required information, in accordance with NC State law for record retention; 11 NCAC 19.0102. Question 2: The Insurer must state whether each of the following programs is included in the Delegated Entity’s UR P&Ps identified in Question/Answer #1: Mental Health/Chemical Dependency, Pharmacy Benefit. If not, the Insurer must provide the same information identified in Question/Answer #1 for each of the programs. Questions 3: The Insurer must identify its internal P&Ps for oversight of the Delegated Entity’s UR program effective during the specified data year by providing the following: Name of Insurer’s UR Oversight P&Ps, including identification number/revision date* Specify Board of Directors, Committee or Name/Title of the Company Officer(s) that approved the UR Oversight P&Ps. Date Insurer’s UR Oversight P&Ps approved by Board of Directors, Committee or Company Officer(s) Effective Date of the Insurer’s UR Oversight P&Ps Managed Care Annual Filing Training Manual 3.2013 Page 35 The Insurer must have in place formalized written P&Ps for oversight of the Delegated Entity’s UR program for each version**. The actual policy must contain either an approval signature/date or the Insurer must be able to provide evidence of the P&Ps’ approval via (committee) meeting minutes. All P&Ps must include an effective date to demonstrate when the process or revised process was initiated or implemented. The policy must include a description of the internal audit mechanism and the frequency of the Insurer’s review of the Delegated Entity’s UR P&Ps, UR form/template letters and actual UR case letters. *The Insurer must maintain all P&Ps and all other required information as stated above for each version in accordance with NC State law for record retention; 11 NCAC 19.0102. Question 4: The Insurer must state whether each of the following programs is included in their oversight P&Ps for the Delegated Entity’s UR P&Ps identified in Question/Answer #3: Mental Health/Chemical Dependency, Pharmacy Benefit. If not, the Insurer must provide the same information identified in Question/Answer #3 for each of the programs. IMPORTANT NOTES PERTAINING TO QUESTIONS #5, #6, #7 AND #8, CONCERNING REVIEW ACTIVITIES: If the review date specified is outside of the specified data year, an explanation MUST be provided (i.e. review was retroactive). For example, if the review date was April 2013, the Insurer must explain whether this review was applicable for data year 2012 or 2013. It is the Department’s position that the Insurer must be conducting annual reviews. The most recent review date will be compared to last year’s most recent review date to confirm that an annual review was conducted (within the rolling 12 months from the last review). If not, the Insurer MUST provide an explanation. The Insurer must provide an explanation for any change in dates or gaps from the date listed in last year’s filing for “next anticipated review”, or if the review is overdue (more than 12 months after the last review). Reviews and Accreditations done by agencies such as NCQA, URAC, etc. do not replace the Insurer’s statutory requirements to monitor performance. The review activities can be performed by external sources; however, it must meet all NC statutory and regulatory requirements. The Insurer must disclose the identity of the external source. Question 5: The Insurer must specify the date (month/year) of its most recent review during the specified data year of the Delegated Entity’s UR P&Ps. Managed Care Annual Filing Training Manual 3.2013 Page 36 Question 6: The Insurer must specify the date (month/year) of its next anticipated review of the Delegated Entity’s UR P&Ps. Question 7: The Insurer must specify the date (month/year) of its most recent review during the specified data year of the Delegated Entity’s UR related form/template letters as required by Statutes. Question 8: The Insurer must specify the date (month/year) of its most recent audit sampling of the Delegated Entity’s UR actual case correspondence (notification letters required by Statutes). Question 9: The Insurer must specify the number of the Delegated Entity’s UR cases reviewed. A case involves all notifications required by Statute for each level of review (see Certification for statutory requirements). Question 10: The Insurer must provide its rationale for determining the number of UR cases of the Delegated Entity reviewed as indicated in Question/Answer #9. The Insurer must be able to justify the number of cases reviewed. The sampling must be a fair representation of all Utilization Reviews reported in the Delegated Entity’s data grids D4 and D5for the specified data year. IMPORTANT NOTES PERTAINING TO QUESTIONS #11 AND #12 CONCERNING CORRECTIVE ACTION PLAN REQUIREMENTS: Domestic Insurers are required to document in the Certification the corrective action taken including the implementation date(s). Foreign Insurers, if deficiencies were found in either the prior or current year’s filing, the Insurer is required to provide evidence demonstrating actual implementation of the corrective action plan. Evidence can be in the form of Committee Meeting Minutes, revised P&Ps, etc. The evidence must contain a (revision) date, as well as, the entity/committee/officer approving the revision. Simply indicating that internal procedures have been revised is inadequate. Due to constraints with the 30 days response time, if a deficiency is found in the current year’s filing and the Insurer is unable to actually implement corrective action, the Insurer must submit a Corrective Action Plan, including a schedule of implementation to resolve the deficiencies. The Insurer must ensure it or its Delegated Entity/Intermediary is taking timely action to correct deficiencies, and taking the appropriate action when either party has not. Managed Care Annual Filing Training Manual 3.2013 Page 37 Question 11: The Insurer must state whether all the Delegated Entity’s UR case correspondence reviewed were compliant (language and time requirements) with State law and included External Review Rights when required. The Insurer MUST explain any deficiencies found, along with corrective actions taken and/or planned. Question 12: The Insurer must detail any areas of non-compliance identified during its reviews of the Delegated Entity’s UR P&Ps and form/template letters. The Insurer MUST explain any deficiencies found, along with corrective actions taken and/or planned. Question 13: The Insurer must specify its staff member(s) who have ultimate oversight responsibilities for the Delegated Entity’s UR Program, including their position titles and clinical degree(s). If more than one person is identified, the Insurer must clarify the duties for each. The Insurer must be able to demonstrate compliance with State law which requires that qualified health care professionals administer the Utilization Review Program and oversee review decisions under the direction of a medical doctor; NCGS 58-50-61(d). Question 14: The Insurer must specify those staff member(s) from the Delegated Entity who have ultimate operational (day-to-day management) responsibilities for its UR Program, including their position titles and clinical degree(s). If more than one person is identified, the Insurer must clarify the duties for each. The Insurer must be able to demonstrate compliance with State law which requires that qualified health care professionals shall administer the Utilization Review Program and oversee review decisions under the direction of a medical doctor; NCGS 58-50-61 (c)(8) and (d). Question 15: The Insurer must specify those staff members from the Delegated Entity who have ultimate oversight responsibilities for its UR Program, including their position titles and clinical degree(s). If more than one person is identified, the Insurer must clarify the duties for each. The Insurer must be able to demonstrate compliance with State law which requires that qualified health care professionals administer the Utilization Review Program and oversee review decisions under the direction of a medical doctor; NCGS 58-50-61(d). Managed Care Annual Filing Training Manual 3.2013 Page 38 Question 16: The Insurer must provide the name, clinical degree(s) and State(s) where the clinical degree(s)/license(s) are active and in good standing for those individuals making noncertification decisions. If the Insurer contracts with an Utilization Review Organization (URO) to perform this function, the name of URO must be identified, and a list of those individual(s) within the URO making noncertification decisions, along with their clinical degree(s) and State(s) where the clinical degree(s)/license(s) are active and in good standing must be provided. Important Note: If the URO reviews the case and communicates their decision back to the Insurer, then the Insurer sends notifications of the decisions to insureds, the URO is not considered a Delegated Entity; therefore, a C5a Utilization Review and, if applicable, a C5b External Review Certification must be completed. State law requires a medical doctor licensed to practice medicine in North Carolina to evaluate the clinical appropriateness of noncertifications: NCGS 58-50-61(d). Managed Care Annual Filing Training Manual 3.2013 Page 39 10. C7 COMPLIANCE CERTIFICATION: INTERMEDIARY ARRANGEMENTS DEFINITION OF INTERMEDIARY: The information presented below is intended to clarify the Department’s interpretation of the “Intermediary” definition found in 11 NCAC 20.0101(b)(4): " 'Intermediary' or 'intermediary organization' means any entity that employs or contracts with health care providers for the provision of health care services, and that also contracts with a network plan carrier or its intermediary." This definition of “intermediary” was intended to include those entities that supply the “network plan carrier” (insurer, HMO, or other entity acting as an insurer as defined in NCGS 58-1-5(3)) with a provider network comprised of otherwise non-related independent providers and group practices. It was not intended to include group practices. Some important distinctions between a group practice and an intermediary are as follows: • Group practices are business entities that are composed of health care providers. A group practice’s providers are often employed by the group practice, typically practicing exclusively under the group’s auspices. Group practices can be single-site or multi-site. For the sake of this discussion, incorporated groups and professional associations (P.A.s) would both be considered group practices, when they participate in provider networks via a single provider agreement (vs. having each individual provider sign his/her own separate participating provider agreement). • In contrast, as the Department’s Bulletin 97-B-3 points out, an intermediary exists separate and apart from the provider and group practices that comprise the intermediary’s network. These practices exist independent of the intermediary, and may contract with multiple carriers and/or intermediaries simultaneously. Various entities would qualify as intermediaries. Some common examples would include preferred provider organizations (PPOs) that contract with unaffiliated providers and then “lease” this network to an insurance company; a single-service managed care organization that, in addition to other services, provides a carrier access to its specialized provider network (e.g., mental health or chiropractic); an independent practice association (IPA) which employs or contracts with a carrier to allow the carrier’s members to receive services from the IPA’s provider network; and a physician-hospital organization (PHO) that contracts with carriers on behalf of its physician and/or hospital members. NOTE: Applying the above definition, the Department views large academic health systems such as Duke, UNC and Wake Forest to be provider groups, not intermediaries. NOTE: An intermediary can also be delegated for additional functions such as credentialing, utilization review, etc. Carriers with questions about how to classify specific entities can be referred to Ted Hamby at (919) 733-5060 ext. 349 or ted.hamby@ncdoi.gov. IMPORTANT NOTE: Pharmacy Benefit Managers are considered Network Intermediaries; therefore, all required information relating to an Intermediary must be provided. A Pharmacy that ONLY fills prescriptions is not a Pharmacy Benefit Manager. A Pharmacy Benefit Manager determines pharmacy benefit levels i.e. medical necessity, appropriateness of prescriptions. Managed Care Annual Filing Training Manual 3.2013 Page 40 Intermediaries are not directly regulated by the Department; however, the Insurer is held responsible for the activities of its Intermediary(s). This Certification must be completed when the Insurer contracts with an Intermediary for a network of contracted providers (Intermediary Arrangements). C7 Certification ensures compliance with State law regarding Intermediary Arrangements and provider contracts. IMPORTANT NOTE: THE INSURER MUST ANSWER EACH QUESTION APPLICABLE TO THE SPECIFED DATA YEAR. A separate certification must be submitted for each Intermediary, and each Intermediary must be listed on the Plan’s data grid D18 with the “Intermediary” activity checked. Enter the name of the Carrier and Intermediary on the first page of the C7 Certification. In Part II, Monitoring Activities, enter the name of the Intermediary and identify all entities subcontracted by the named Intermediary (i.e. leased networks, intermediaries). Question 1: The Carrier must identify its internal P&Ps for oversight of the Intermediary’s provider contracting effective during the specified data year by providing the following: Name of Carrier’s P&Ps for oversight of the Intermediary’s provider contracting, including identification number/revision date* Specify Board of Directors, Committee or Name/Title of the Company Officer(s) that approved the Carrier’s P&Ps for oversight of the Intermediary’s provider contracting Date Carrier’s P&Ps for oversight of the Intermediary’s provider contracting was approved by Board of Directors, Committee or Company Officer(s) Effective Date of the Carrier’s P&Ps for oversight of the Intermediary’s provider contracting The Carrier must have in place formalized written P&Ps for oversight of the functions delegated to the Intermediary for each version**. The actual P&Ps must contain either an approval signature/date or the Carrier must be able to provide evidence of the P&Ps’ approval via (committee) meeting minutes. All P&Ps must include an effective date to demonstrate when the process or revised process was initiated or implemented. The P&PSs must include a description of the internal audit mechanism (review of the Intermediary agreement, review of the Intermediary’s P&Ps, review of the Intermediary’s form/template provider agreement(s), and an audit sampling of the Intermediary’s executed provider contracts), and the frequency of the Insurer’s reviews. *If any revisions were made to the P&Ps from the previous data year, the Insurer must briefly describe the changes. Do not attach copies of the actual revised P&Ps unless requested by the Department. Managed Care Annual Filing Training Manual 3.2013 Page 41 **The Carrier must maintain all P&Ps and all other required information (as stated above) for each version in accordance with NC State law for record retention; 11 NCAC 19.0102. It is the Department’s position that the Carrier MUST be conducting reviews at least annually in order to certify compliance with 11 NCAC 20.0202 and 20.0204 in the C7 Certification. In reviewing the Intermediary contract, the review must determine if the contract specifically addresses the activities which have been delegated to the intermediary, the intermediary’s responsibilities with respect to those delegated activities and the oversight activities to be performed by the Insurer. IMPORTANT NOTES PERTAINING TO QUESTIONS #2, #3 and #4, CONCERNING REVIEW ACTIVITIES: If the review date specified is outside of the specified data year, an explanation MUST be provided (i.e. review was retroactive). For example, if the review date was April 2013, the Insurer must explain whether this review was applicable for data year 2012 or 2013. It is the Department’s position that the Insurer must be conducting annual reviews. The most recent review date will be compared to last year’s most recent review date to confirm that an annual review was conducted (within the rolling 12 months from the last review). If not, the Insurer MUST provide an explanation. The Insurer must provide an explanation for any change in dates or gaps from the date listed in last year’s filing for “next anticipated review”, or if the review is overdue (more than 12 months after the last review). Reviews and Accreditations done by agencies such as NCQA, URAC, etc. do not replace the Insurer’s statutory requirements to monitor performance. The review activities can be performed by external sources; however, it must meet all NC statutory and regulatory requirements. The Insurer must disclose the identity of the external source. Providing a copy of the Life & Health Division’s approval letter for the provider contract form/template or Intermediary contract does not replace the Carrier’s responsibility for ongoing monitoring. Question 2: The Carrier must specify the date (month/year) of its most recent review during the specified data year of the Intermediary’s provider contract form/template. Managed Care Annual Filing Training Manual 3.2013 Page 42 IMPORTANT NOTES PERTAINING TO AUDIT SAMPLING QUESTION #3: Having a contract management system where contracts are handled electronically (on-line) with safeguards for edits, does not exempt the Carrier from performing the required oversight to ensure the contracts are compliant by pulling an actual sampling of executed provider contracts to audit. The printed provider contract could be modified or struck through then initialed/executed manually; thereby, changing the contract from the “authorized” form stored electronically. The audit sampling MUST be selected by the entity performing the audit. If the Carrier audits the Intermediary, then the Carrier must pull the audit sampling. If the Intermediary audits the subcontracted Intermediary, then the Intermediary must pull the audit sampling. The sampling must be refreshed each year (not allowing for the same providers to be selected year-to-year). The sampling must be random and duplicate data removed. The Carrier must not limit its sampling to only newly executed provider contracts. The audit sampling must include a fair representation of ALL executed provider contracts, including both newly contracted and renewed providers, during the specified data year (unique providers reported in D7). Question 3: The Carrier must specify the date (month/year) of its most recent audit sampling of the Intermediary’s executed provider contracts during the specified data year. Question 4: The Carrier must specify the date(s) (month/year) of its next anticipated review of the Intermediary’s provider form/template and audit sampling of the Intermediary’s executed provider contracts. Question 5: The Carrier must specify the number of the Intermediary’s executed provider contracts reviewed by the Carrier. Question 6: The Carrier must specify whether a subcontracted Intermediary was utilized. If “yes”, specify which organization (i.e. Carrier/Intermediary and Name/Title) conducted the oversight of the subcontracted Intermediary’s P&Ps, provider contract form/template and audit sampling of the subcontracted Intermediary’s executed provider contracts. The Carrier must specify the number of the subcontracted Intermediary’s executed provider contracts reviewed and specify the date (month/year) of the review. Managed Care Annual Filing Training Manual 3.2013 Page 43 Question 7: If the review of the subcontracted Intermediary was conducted by the Intermediary, state how and when the oversight results were communicated to the Carrier. If the review was conducted by the Carrier, this question is not applicable, as the Carrier would report the results of their review in Question/Answer #6. Question 8: The Carrier must explain its rationale in determining the number of the Intermediary’s, and if applicable, subcontracted Intermediary’s executed provider contracts audited. The Carrier must be able to justify the number of executed provider contracts reviewed. While the Department does not determine the number of executed provider contracts that must be audited, the number reviewed must be a fair representation of the number of unique providers participating in the network (data grid D7). IMPORTANT NOTES PERTAINING TO QUESTIONS #9 AND #10 CONCERNING CORRECTIVE ACTION PLAN REQUIREMENTS: Domestic Insurers are required to document in the Certification the corrective action taken including the implementation date(s). Foreign Insurers, if deficiencies were found in either the prior or current year’s filing, the Insurer is required to provide evidence demonstrating actual implementation of the corrective action plan. Evidence can be in the form of Committee Meeting Minutes, revised P&Ps, etc. The evidence must contain a (revision) date, as well as, the entity/committee/officer approving the revision. Simply indicating that internal procedures have been revised is inadequate. Due to constraints with the 30 days response time, if a deficiency is found in the current year’s filing and the Insurer is unable to actually implement corrective action, the Insurer must submit a Corrective Action Plan, including a schedule of implementation to resolve the deficiencies. The Insurer must ensure it or its Delegated Entity/Intermediary is taking timely action to correct deficiencies, and taking the appropriate action when either party has not. Question 9: The Carrier must identify any areas of non-compliance found during its review of the Intermediary’s and, if applicable, subcontracted Intermediary’s provider contract form/template. If applicable, the Carrier must include in the Corrective Action Plan whether the area of noncompliance was determined to be a systemic error/problem or an isolated issue. The Carrier will also need to describe the effects on previous years’ executed provider contracts, and how the issue is/was corrected going forward. Managed Care Annual Filing Training Manual 3.2013 Page 44 Question 10: The Carrier must identify all deficiencies found during its audit sampling of the Intermediary’s and, if applicable, subcontracted Intermediary’s (or the Intermediary’s audit sampling of the subcontracted Intermediary’s) executed provider contracts. If applicable, the Carrier must include in the Corrective Action whether the area of noncompliance was determined to be systematic error/problem or an isolated issue. The Carrier will also need to describe the effects on previous years’ executed provider contracts, and how the issue is/was corrected going forward. Question 11: The Carrier must provide the form number of the Intermediary’s and, if applicable, subcontracted Intermediary’s provider contract form/template reviewed for compliance. The form number is located in the lower left corner of the contract; 11 NCAC 20.0205(3). 11 NCAC 20.0201(b) requires Carriers to file provider contracts with the Life & Health Division for approval before it is used. Question 12: The Carrier must specify whether any material changes*, as defined in 11 NCAC 20.0203, were made to any of the executed provider contracts reviewed in the Insurer’s and/or Intermediary’s audit samplings. If “yes”, the SERFF Tracking Number for the filing of the revised provider contract must be provided. The Insurer must provide an explanation if no SERFF Tracking Number is available. For HMOs 11 NCAC 20.0601(e) requires all changes to provider and intermediary contract forms be submitted to the Life & Health Division for review and approval in accordance with 11 NCAC 20.0203 prior to the use of the amended form. *An approved form number cannot be changed without prior approval from the Life & Division. Question 13: The Carrier must specify whether any material changes*, as defined in 11 NCAC 20.0203, were made to the contract between the Carrier and Intermediary. If “yes”, the SERFF Tracking Number for the filing of the revised Intermediary contract must be provided. The Insurer must provide an explanation if no SERFF Tracking Number is available. For HMOs 11 NCAC 20.0601(e) requires that all changes to provider and intermediary contract forms be submitted to the Life & Health Division for review and approval in accordance with 11 NCAC 20.0203 prior to the use of the amended form. Managed Care Annual Filing Training Manual 3.2013 Page 45 11 NCAC 20.0201(b) and 11 NCAC 20.0204(a) requires carriers to file intermediary contracts with the Life & Health Division for approval before use. *An approved form number cannot be changed without prior approval from the Life & Division. Question 14: If the Intermediary paid claims, the Carrier must state if the Intermediary holds an active and valid TPA license for the specified data year. For any questions or concerns regarding this subject, please contact our Life & Health Division for guidance. Question 15: If the Carrier pays the Intermediary directly for the services provided, the Carrier must state whether it has in place financial protection for itself and its members through member hold harmless language. If “no”, the Carrier must provide an explanation. Managed Care Annual Filing Training Manual 3.2013 Page 46 11. C8. COMPLIANCE CERTIFICATION: PROVIDER AVAILABILITY AND ACCESSIBILITY The provider availability and accessibility (network adequacy) portion of the annual filing is designed to ensure that Carriers offering managed care plans maintain service networks that are sufficient to ensure that all services offered are accessible to members without unreasonable delay. The standards require Carriers to ensure the adequacy, accessibility and quality of health care services offered through its own and/or its Intermediary’s service networks. Grievances related to provider access issues reported in D3 Data Grid (Plan’s or Intermediary’s), must be further explained in the applicable question/answer. Submission of either the C8 or C9 is determined by whether the Plan or Intermediary sets the standards. Use C8 when the Carrier sets the standards for its network and/or when the Intermediary adopts the Carrier’s standards. Use C9 when the Intermediary sets the standards for its network and/or when the Plan adopts the Intermediary’s standards. Separate C8 Certifications are needed for each Intermediary that adopted the Plan’s standards. Each Intermediary must be listed on the Plan’s data grid D18 with the “Intermediary” activity checked. When the Plan sets the standards; the Plan monitors the network and runs/furnishes reports: Complete a C8 Certification. Identify which standard(s) (network density, driving distance, appointment wait times) is established by Plan. Identify the reports supplied to support the results for the standards established by the Plan and reported in the applicable provider availability/accessibility data grids. Record the standards in the applicable Plan data grids (D10, D12, and D14). Record the results in the applicable Plan data grids (D11, D13, and D15). When the Plan sets the standards; the Intermediary monitors the network and runs/furnishes the Plan with reports: Complete a C8 Certification for each Intermediary for which Plan sets the standards. Identify which standard(s) (network density, driving distance, appointment wait times) is established by Plan. Identify the reports supplied by the Intermediary to support the results for the standards established by the Plan and reported in the applicable provider availability/accessibility data grids. Managed Care Annual Filing Training Manual 3.2013 Page 47 Record the standards in the applicable Plan data grids (D10, D12, and D14). Record the results in the applicable Intermediary’s delegated data grids (D11, D13, and D15). When the Plan sets one or more of the provider availability/accessibility standards and the Intermediary sets one or more of the provider availability/accessibility standards, both a C8 and C9 Certification must be completed. For example, when the Plan sets network density and driving distance standards and the Intermediary sets appointment wait times, complete a C8 Certification for network density and driving distance and complete a C9 for appointment wait times. In each Certification only answer those questions applicable to the standards set by the applicable entity. For this example, the questions pertaining to network density and driving distance must be answered in C8. Questions pertaining to appointment wait times must be answered in the C9 Certification. If the Plan uses “benchmarks” (minimum requirements) for the intermediary to meet and the intermediary meets or exceeds the benchmarks and the Plan adopts the Intermediary’s standards, a C9 Certification will apply. If the Plan does not adopt the Intermediary’s standards, a C8 Certification will apply. IMPORTANT NOTE: THE CARRIER MUST ANSWER EACH QUESTION APPLICABLE TO THE SPECIFED DATA YEAR. A response to all questions must be provided. If the is response is “N/A” an explanation must be provided. Enter the name of the Carrier and Intermediary, if applicable, on the first page of the C8 Certification. Enter the name of the Intermediary on Part ll. Monitoring Activities of the Certification, if applicable. Question 1: The Carrier must check which standard(s) [network density, driving distance, appointment wait times] is established by the Plan. DO NOT DISCLOSE THE ACTUAL STANDARDS. The actual standards must be reported in the applicable data grids. Question 2: The Carrier must identify its P&Ps for Provider Availability & Accessibility effective during the specified data year by providing the following: Name of Carrier’s Provider Availability & Accessibility P&Ps, including identification number/revision date* Specify Board of Directors, Committee or Name/Title of the Company Officer(s) that approved the Provider Availability & Accessibility P&Ps Managed Care Annual Filing Training Manual 3.2013 Page 48 Date Carrier’s Provider Availability & Accessibility P&Ps approved by Board of Directors, Committee or Company Officer(s) Effective Date of the Carrier’s Provider Availability & Accessibility P&Ps The Carrier must have in place formalized written P&Ps for Provider Availability & Accessibility for each version**. The actual P&Ps must contain either an approval signature/date or the Carrier must be able to provide evidence of the P&Ps’ approval via (committee) meeting minutes. All P&Ps must include an effective date to demonstrate when the process or revised process was initiated or implemented. The P&Ps must include a description of the internal audit mechanism and the frequency of the Carrier’s review of its Provider Availability & Accessibility P&Ps, and network performance. *If any revisions were made to the P&Ps from the previous data year, the Insurer must briefly describe the changes. Do not attach copies of the actual revised P&Ps unless requested by the Department. **The Carrier must maintain all P&Ps and all other required information (as stated above) for each version in accordance with NC State law for record retention; 11 NCAC 19.0102. For any change in a standard from previous data year identified in Question/Answer #18, a corresponding revision date to the Provider Availability & Accessibility P&Ps for the specified change must be indicated in Question/Answer #2 . IMPORTANT NOTES PERTAINING TO QUESTIONS #3 AND #4, CONCERNING REVIEW ACTIVITIES: If the review date specified is outside of the specified data year, an explanation MUST be provided (i.e. review was retroactive). For example, if the review date was April 2013, the Insurer must explain whether this review was applicable for data year 2012 or 2013. It is the Department’s position that the Insurer must be conducting annual reviews. The most recent review date will be compared to last year’s most recent review date to confirm that an annual review was conducted (within the rolling 12 months from the last review). If not, the Insurer MUST provide an explanation. The Insurer must provide an explanation for any change in dates or gaps from the date listed in last year’s filing for “next anticipated review”, or if the review is overdue (more than 12 months after the last review). Reviews and Accreditations done by agencies such as NCQA, URAC, etc. do not replace the Insurer’s statutory requirements to monitor performance. The review activities can be performed by external sources; however, it must meet all NC statutory and regulatory requirements. The Insurer must disclose the identity of the external source. Managed Care Annual Filing Training Manual 3.2013 Page 49 Providing a copy of the Life & Health Division’s approval letter for provider availability and accessibility does not replace the Carrier’s responsibility for ongoing monitoring. Question 3: The Carrier must specify the date (month/year) of its most recent review during the specified data year of its Provider Availability & Accessibility P&Ps. Question 4: The Carrier must specify the date (month/year) of its next anticipated review of its P&Ps regarding Provider Availability & Accessibility. Question 5: If the Carrier is monitoring availability/accessibility according to the terms and frequency of its established P&Ps, the Carrier must state “Yes” or “No”. If “No”, an explanation must be provided. IMPORTANT NOTES PERTAINING TO QUESTION #6 CONCERNING CORRECTIVE ACTION PLAN REQUIREMENTS: Domestic Insurers are required to document in the Certification the corrective action taken including the implementation date(s). Foreign Insurers, if deficiencies were found in either the prior or current year’s filing, the Insurer is required to provide evidence demonstrating actual implementation of the corrective action plan. Evidence can be in the form of Committee Meeting Minutes, revised P&Ps, etc. The evidence must contain a (revision) date, as well as, the entity/committee/officer approving the revision. Simply indicating that internal procedures have been revised is inadequate. Due to constraints with the 30 days response time, if a deficiency is found in the current year’s filing and the Insurer is unable to actually implement corrective action, the Insurer must submit a Corrective Action Plan, including a schedule of implementation to resolve the deficiencies. The Insurer must ensure it or its Delegated Entity/Intermediary is taking timely action to correct deficiencies, and taking the appropriate action when either party has not. Question 6: The Carrier must detail any areas of non-compliance identified during the review of its Provider Availability & Accessibility P&Ps. For any area of non-compliance identified, the Carrier must state the corrective action taken and/or planned, including implementation dates. Managed Care Annual Filing Training Manual 3.2013 Page 50 Question 7: The Carrier must name the report reviewed by the Carrier to determine if the network density standards for the specified data year were met (i.e. GeoAcess). If the Carrier/Intermediary calculates network density results using membership data grid D2 and provider counts from either D6 or D7, the Carrier must identify the reports supporting the membership/provider counts reported in these data grids. Merely referencing these data grids is insufficient. Question 8: The Carrier must specify the date of the report identified in Question/Answer #7, the time period covered by the report, and the date the Carrier reviewed the report. Each of these components must be answered. Remember network density results must be as of December 31st of the specified data year and based on the Carrier’s commercial insured managed care membership in NC (including border counties), and NC contracted providers (including border counties). This does not mean the Plan/Intermediary needs to run the report exactly on December 31st but when running the report the period ending date must be December 31st of the specified data year. Question 9: The Carrier must identify any network density standard which was not met, along with corrective action planned/taken. If the target was narrowly missed (within 5% of target) the Insurer must acknowledge the missed target and indicate that no corrective action plan was necessary. The Insurer will need to continue closely monitoring the network. If the target was missed by more than 5%, the Insurer must describe the corrective action taken/planned by it and/or the Intermediary. If no corrective action was taken/planned, an explanation must be provided in the applicable Certification. Question 10: The Carrier must name the report reviewed by the Carrier to determine if the driving distance standards for the specified data year were met (i.e. GeoAcess). Question 11: The Carrier must specify the date of the report identified in Question/Answer #10, the time period covered by the report, and the date the Carrier reviewed the report. Each of these components must be answered. Managed Care Annual Filing Training Manual 3.2013 Page 51 Remember driving distance results must be as of December 31st of the specified data year and based on the Carrier’s commercial insured managed care membership in NC (including border counties), and NC contracted providers (including border counties). This does not mean the Plan/Intermediary needs to run the report exactly on December 31st but when running the report the period ending date must be December 31st of the specified data year. Question 12: The Carrier must identify any driving distance standard which was not met, along with corrective action planned/taken. If the target was narrowly missed (within 5% of target) the Insurer must acknowledge the missed target and indicate that no corrective action plan was necessary. The Insurer will need to continue closely monitoring the network. If the target was missed by more than 5%, the Insurer must describe the corrective action taken/planned by it and/or the Intermediary. If no corrective action was taken/planned, an explanation must be provided in the applicable Certification. Question 13: The Carrier must specify if a NC Member Satisfaction Survey or NC Provider Survey was used in determining the appointment wait times results. Remember appointment wait times results must be based on the Carrier’s commercial insured managed care membership in NC including border counties. Surveys conducted on another basis i.e. national or regional basis are unacceptable. If both the Carrier and the Intermediary perform surveys to measure the standards for appointment wait times, the Carrier must disclose which survey is considered primary and record the results accordingly. For example, if the Carrier’s survey is primary, the results must be recorded in the Plan’s data grid D15. However, if the Intermediary’s survey is primary, the results must be recorded in the Intermediary’s data grid D15. The Carrier is responsible for reviewing the survey to determine if the questions are appropriate to measure its appointment wait times standards. The questions MUST tie back to the actual standards. For example, if the target was 10 business days for PCP routine care the appropriate question to ask would be “Were you able to obtain a routine care appointment with your PCP within 10 business days?” General and vague questions like, “Were you able to obtain an appointment within a reasonable time?” do not accurately measure the target; therefore, they are unacceptable. For Quality Management purposes, the Department recommends including questions in the provider and member surveys to measure the following: 1) how long a member sits in the waiting room before being called back to an examination room, and 2) how long a member waits in the examination room before the actual service is rendered by the provider. Managed Care Annual Filing Training Manual 3.2013 Page 52 Question 14: The Carrier must specify the date of the survey identified in Question/Answer #13, the time period the survey covered, and the date the Carrier reviewed the survey results. Each of these components must be addressed. The Carrier must ensure that survey results were based on services rendered during the specified data year. Question 15: The Carrier must disclose the participation rate (# of members/providers surveyed vs. # of respondents). The Department does not determine the required (valid) participation rate. The number of respondents must be a fair representation of the number of members/providers surveyed. If the number of responses was not enough to adequately analyze the performance, a supplemental method (i.e. reviewing complaints/grievances) must be used in conjunction with the surveys. Remember, only reviewing grievance/complaint data is not a sufficient method. Question 16: If applicable, the Carrier must describe any supplemental method used to measure any appointment wait times type (i.e. Routine, Urgent, Emergent/Emergency) including the date of the report, the time period covered by the report, and the date the Carrier reviewed the report. Each of these components must be answered. A supplemental method must be used if the member/provider survey was invalid due to the lack of respondents. The Insurer must also describe if a different method was used to measure an appointment wait times type (i.e. cold calls to providers’ offices after hours to measure emergency appointment wait times). Question 17: The Carrier must identify any appointment wait time standard which was not met, along with corrective action planned/taken. If the target was narrowly missed (within 5% of target) the Insurer must acknowledge the missed target and indicate that no corrective action plan was necessary. The Insurer will need to continue closely monitoring the network. If the target was missed by more than 5%, the Insurer must describe the corrective action taken/planned by it and/or the Intermediary. If no corrective action was taken/planned, an explanation must be provided in the applicable Certification. Managed Care Annual Filing Training Manual 3.2013 Page 53 Question 18: The Carrier must state (“yes” or “no”) if any standard (network density, driving distance, appointment wait times) was revised from the previous data year. If “yes”, the Carrier must disclose the change, the reason for the change and the date the change was approved/adopted by the Carrier. Each of these components must be answered. Before approving/adopting a change for any standard the Carrier must evaluate how the change will affect its members. Lowering a standard for the sole purpose of meeting/exceeding the established goal is unacceptable. Question 19: Full Service Plans: The Carrier must state it or its Intermediary’s (as applicable) policy for paying claims for in-network emergency care, and state if pre-authorization is required; refer to NCGS 58-3-190 for statutory requirements. Single Service Vision Plans: If the benefit is a wellness plan and therefore does not cover emergency care (i.e. vision - exams and hardware only) a statement of such must be provided. Single Service Dental Plans: If the benefit covers emergency services, the Carrier must state it or its Intermediary’s (as applicable) policy for paying claims for in-network emergency care, and state if pre-authorization is required. If pre-authorization is required the Carrier or Intermediary must describe how it is documented in the claim system for proper processing/payment. Question 20: Full Service Plans: The Carrier must state it or its Intermediary’s (as applicable) policy for paying claims for out-of-network emergency care, and state if pre-authorization is required. It must be clear to the Department that claims are being paid at the in-network benefit without penalty to the member; NCGS 58-3-190 and NCGS 58-3-200(d). Single Service Vision Plans: If the benefit is a wellness plan and therefore does not cover emergency care (i.e. vision - exams and hardware only) a statement of such must be provided. Single Service Dental Plans: If the benefit covers emergency services, the Carrier must state it or its Intermediary’s (as applicable) policy for paying claims for out-of-network emergency care, and state if pre-authorization is required. It is the Department’s position, in accordance with 11 NCAC 20.0301 and 20.0302, that the Carrier must maintain an adequate network to provide covered services to its members at the in-network benefit level. Therefore, when in-network providers are not available within the established standards, a Carrier must allow the member to seek services from out-of-network providers at the in-network benefit level. Managed Care Annual Filing Training Manual 3.2013 Page 54 If pre-authorization is required the Carrier or Intermediary must describe how it is documented in the claim system for proper processing/payment. Question 21: The Carrier must state the provisions (addressing authorization and claim payment) made for members when care by a participating provider cannot be received within the availability and accessibility standards, and a member seeks care from a non-participating provider. This includes those counties with membership but no or limited providers. In the description the Carrier must state if pre-authorization/notification is required, how the claim is paid (in-network or out-of-network), whether the member is balance billed, and whether a member has to file a grievance/appeal for reimbursement at the in-network level. Each component must be answered. The Department must ensure that the covered person obtains the covered benefit at no greater cost to the covered person than if the benefit were obtained from participating providers. Question 22: The Carrier must state the actual disclosure provisions communicated to members about receiving care from a non-participating provider when an in-network provider is not reasonably available (within the standards for driving distance and/or appointment wait times). The Carrier must identify the document used during the reporting period which disclosures these provisions (i.e. member handbook, enrollment material, Certificate, etc.) in accordance with the provisions of 11 NCAC 12.1804. Question 23: If the named Intermediary used a subcontracted entity (as identified in the C7 Certification) and its provider network(s) was used to supplement the Plan’s or Intermediary’s network (not a standalone network option) the Carrier must state whether (“Yes” or “No”) the answers and provider availability/accessibility results were inclusive for ALL participating providers. If “No”, an explanation must be provided. Managed Care Annual Filing Training Manual 3.2013 Page 55 12. C9. COMPLIANCE CERTIFICATION: DELEGATED PROVIDER AVAILABILITY AND ACCESSIBILITY The provider availability and accessibility (network adequacy) portion of the annual filing is designed to ensure that Carriers offering managed care plans maintain service networks that are sufficient to ensure that all services offered are accessible to members without unreasonable delay. The standards require Carriers to ensure the adequacy, accessibility and quality of health care services offered through its own and/or its Intermediary’s service networks. Grievances related to provider access issues reported in D3 Data Grid (Plan’s or Intermediary’s), must be further explained in the applicable question/answer. Submission of either the C8 or C9 is determined by whether the Plan or Intermediary sets the standards. Use C8 when the Carrier sets the standards for its network and/or when the intermediary adopts the Carrier’s standards. Use C9 when the Intermediary sets the standards for its network and/or when the Plan adopts the Intermediary’s standards. Separate C9 Certifications are needed for each Intermediary. Each Intermediary must be listed under Item #C9 on the C1. Annual Filing Checklist, and listed on the Plan’s data grid D18 with the “Intermediary” and “Provider Availability & Accessibility” activities checked. When the Intermediary sets the standards; Intermediary monitors the network and runs/furnishes the Plan with reports: Complete a C9 Certification. Identify which standard(s) (network density, driving distance, appointment wait times) is established by Intermediary. Identify the reports supplied by the Intermediary to support the results for the standards established by the Intermediary and reported in the applicable provider availability and accessibility data grids. Record the standards in the applicable Intermediary’s delegated data grids (D10, D12, and D14). Record the results in the applicable Intermediary’s delegated data grids (D11, D13, and D15). When the Intermediary sets the standards; Plan monitors the network and runs/furnishes the reports: Complete a C9 Certification for each applicable Intermediary. Identify which standard(s) (network density, driving distance, appointment wait times) is established by Intermediary. Managed Care Annual Filing Training Manual 3.2013 Page 56 Identify the reports supplied by the Plan to support the results for the standards established by the Intermediary and reported in the applicable provider availability and accessibility data grids. Record the standards in the applicable Intermediary’s delegated data grids (D10, D12, and D14). Record the results in the applicable Plan data grids (D11, D13, and D15). When the Plan sets one or more of the provider availability/accessibility standards and the Intermediary sets one or more of the provider availability/accessibility standards, both a C8 and C9 Certification must be completed. For example, when the Plan sets network density and driving distance standards and the Intermediary sets appointment wait times, complete a C8 Certification for network density and driving distance and complete a C9 for appointment wait times. In each Certification only answer those questions applicable to the standards set by the applicable entity. For this example, the questions pertaining to network density and driving distance must be answered in C8. Questions pertaining to appointment wait times must be answered in the C9 Certification. If the Plan uses “benchmarks” (minimum requirements) for the intermediary to meet and the intermediary meets or exceeds the benchmarks and the Plan adopts the Intermediary’s standards, a C9 Certification will apply. If the Plan does not adopt the Intermediary’s standards, a C8 Certification will apply. IMPORTANT NOTE: THE CARRIER MUST ANSWER EACH QUESTION APPLICABLE TO THE SPECIFED DATA YEAR. A response to all questions must be provided. If the response is “N/A” an explanation must also be provided. Enter the name of the Carrier and Intermediary on the first page of the C9 Certification Enter the name of the Intermediary on Part ll. Monitoring Activities of the Certification Question 1: The Carrier must check which standard(s) [network density, driving distance, appointment wait times] is established by the Intermediary. DO NOT DISCLOSE THE ACTUAL STANDARDS. The actual standards must be reported in the applicable data grids. Question 2: The Carrier must identify its internal P&Ps for oversight of the Intermediary’s Provider Availability & Accessibility effective during the specified data year by providing the following: Name of Carrier’s Delegated Provider Availability/Accessibility Oversight P&Ps, including identification number/revision date* Managed Care Annual Filing Training Manual 3.2013 Page 57 Specify Board of Directors, Committee or Name/Title of the Company Officer(s) that approved the Carrier’s Delegated Provider Availability/Accessibility Oversight P&Ps Date Carrier’s Delegated Provider Availability/Accessibility Oversight P&Ps approved by Board of Directors, Committee or Company Officer(s) Effective Date of the Carrier’s Delegated Provider Availability/Accessibility Oversight P&Ps The Carrier must have in place formalized written P&Ps for Oversight of the Delegated Provider Availability & Accessibility for each version**. The actual policy must contain either an approval signature/date or the Carrier must be able to provide evidence of the P&Ps’ approval via (committee) meeting minutes. All P&Ps must include an effective date to demonstrate when the process or revised process was initiated or implemented. The P&Ps must include a description of the internal audit mechanism and the frequency of the Carrier’s review of the Intermediary’s Provider Availability & Accessibility P&Ps, and network performance. *If any revisions were made to the P&Ps from the previous data year, the Insurer must briefly describe the changes. Do not attach copies of the actual revised P&Ps unless requested by the Department. **The Carrier must maintain all P&Ps and all other required information (as stated above) for each version in accordance with NC State law for record retention; 11 NCAC 19.0102. For any change in a standard from previous data year identified in Question/Answer #19, a corresponding revision date to the Intermediary’s Provider Availability & Accessibility P&Ps for the specified change must be indicated in Question/Answer #3 . Question 3: The Carrier must identify the Intermediary’s P&Ps for Provider Availability & Accessibility effective during the specified data year by providing the following: Name of Intermediary’s P&Ps, including identification number/revision date* Date Intermediary’s P&Ps approved internally by Intermediary Specify Board of Directors, Committee or Name/Title of the Company Officer(s) from the Intermediary that approved the Intermediary’s Provider Availability & Accessibility P&Ps Date Intermediary’s Provider Availability & Accessibility P&Ps approved by Board of Directors, Committee or Company Officer(s) Effective Date of the Intermediary’s Provider Availability & Accessibility P&Ps Specify Board of Directors, Committee or Name/Title of the Company Officer(s) from the Carrier that approved the Intermediary’s Provider Availability & Accessibility P&Ps Date Carrier approved the Intermediary’s Provider Availability & Accessibility P&Ps Managed Care Annual Filing Training Manual 3.2013 Page 58 The Intermediary must have in place formalized written Provider Availability & Accessibility P&Ps for each version**. The actual P&Ps must contain either an approval signature/date or the Carrier must be able to provide evidence of the Delegated Entity’s approval of the P&Ps via (committee) meeting minutes. All P&Ps must include an effective date to demonstrate when the process or revised process was initiated or implemented. *If any revisions were made to the P&Ps from the previous data year, the Insurer must briefly describe the changes. Do not attach copies of the actual revised P&Ps unless requested by the Department. **The Insurer must maintain and must ensure the delegated entity maintains, all P&Ps and all other required information for each version (as stated above) in accordance with NC State law for record retention; 11 NCAC 19.0102. **The Insurer must maintain evidence of review and approval for each version of the Delegated Entity’s P&Ps and all other required information, in accordance with NC State law for record retention; 11 NCAC 19.0102. IMPORTANT NOTES PERTAINING TO QUESTIONS #4 AND #5, CONCERNING REVIEW ACTIVITIES: If the review date specified is outside of the specified data year, an explanation MUST be provided (i.e. review was retroactive). For example, if the review date was April 2013, the Insurer must explain whether this review was applicable for data year 2012 or 2013. It is the Department’s position that the Insurer must be conducting annual reviews. The most recent review date will be compared to last year’s most recent review date to confirm that an annual review was conducted (within the rolling 12 months from the last review). If not, the Insurer MUST provide an explanation. The Insurer must provide an explanation for any change in dates or gaps from the date listed in last year’s filing for “next anticipated review”, or if the review is overdue (more than 12 months after the last review). Reviews and Accreditations done by agencies such as NCQA, URAC, etc. do not replace the Insurer’s statutory requirements to monitor performance. The review activities can be performed by external sources; however, it must meet all NC statutory and regulatory requirements. The Insurer must disclose the identity of the external source. Providing a copy of the Life & Health Division’s approval letter for provider availability and accessibility does not replace the Carrier’s responsibility for ongoing monitoring. Managed Care Annual Filing Training Manual 3.2013 Page 59 Question 4: The Carrier must specify the date (month/year) of its most recent review during the specified data year of the Intermediary’s Provider Availability & Accessibility P&Ps. Question 5: The Carrier must specify the date (month/year) of its next anticipated review of the Intermediary’s Provider Availability & Accessibility P&Ps. Question 6: If the Intermediary is monitoring availability/accessibility according to the terms and frequency of its established P&Ps, the Carrier must state “Yes” or “No”. If “No”, an explanation must be provided. IMPORTANT NOTES PERTAINING TO QUESTION #7 CONCERNING CORRECTIVE ACTION PLAN REQUIREMENTS: Domestic Insurers are required to document in the Certification the corrective action taken including the implementation date(s). Foreign Insurers, if deficiencies were found in either the prior or current year’s filing, the Insurer is required to provide evidence demonstrating actual implementation of the corrective action plan. Evidence can be in the form of Committee Meeting Minutes, revised P&Ps, etc. The evidence must contain a (revision) date, as well as, the entity/committee/officer approving the revision. Simply indicating that internal procedures have been revised is inadequate. Due to constraints with the 30 days response time, if a deficiency is found in the current year’s filing and the Insurer is unable to actually implement corrective action, the Insurer must submit a Corrective Action Plan, including a schedule of implementation to resolve the deficiencies. The Insurer must ensure it or its Delegated Entity/Intermediary is taking timely action to correct deficiencies, and taking the appropriate action when either party has not. Question 7: The Carrier must detail any areas of non-compliance identified during the review of the Intermediary’s Provider Availability & Accessibility P&Ps. For any area of non-compliance identified, the Carrier must state the corrective action taken and/or planned, including implementation dates. Question 8: The Carrier must name the report reviewed by the Carrier to determine if the network density standards for the specified data were met (i.e. GeoAcess). Managed Care Annual Filing Training Manual 3.2013 Page 60 If the Carrier/Intermediary calculates network density results using membership data grid D2 and provider counts from either D6 or D7, the Carrier must identify the reports supporting the membership/provider counts reported in these data grids. Merely referencing these data grids is insufficient. Question 9: The Carrier must specify the date of the report identified in Question/Answer #8, the time period covered by the report, and the date the Carrier reviewed the report. Each of these components must be answered. Remember network density results must be as of December 31st of the specified data year and based on the Carrier’s commercial insured managed care membership in NC (including border counties), and NC contracted providers (including border counties). This does not mean the Plan/Intermediary needs to run the report exactly on December 31st but when running the report the period ending date must be December 31st of the specified data year. Question 10: The Carrier must identify any network density standard which was not met, along with corrective action planned/taken. If the target was narrowly missed (within 5% of target) the Insurer must acknowledge the missed target and indicate that no corrective action plan was necessary. The Insurer will need to continue closely monitoring the network. If the target was missed by more than 5%, the Insurer must describe the corrective action taken/planned by it and/or the Intermediary. If no corrective action was taken/planned, an explanation must be provided in the applicable Certification. Question 11: The Carrier must name the report reviewed by the Carrier to determine if the driving distance standards for the specified data were met (i.e. GeoAcess). Question 12: The Carrier must specify the date of the report identified in Question/Answer #11, the time period covered by the report, and the date the Carrier reviewed the report. Each of these components must be answered. Remember driving distance results must be as of December 31st of the specified data year and based on the Carrier’s commercial insured managed care membership in NC (including border counties), and NC contracted providers (including border counties). This does not mean the Plan/Intermediary needs to run the report exactly on December 31st but when running the report the period ending date must be December 31st of the specified data year. Managed Care Annual Filing Training Manual 3.2013 Page 61 Question 13: The Carrier must identify any driving distance standard which was not met, along with corrective action planned/taken. If the target was narrowly missed (within 5% of target) the Insurer must acknowledge the missed target and indicate that no corrective action plan was necessary. The Insurer will need to continue closely monitoring the network. If the target was missed by more than 5%, the Insurer must describe the corrective action taken/planned by it and/or the Intermediary. If no corrective action was taken/planned, an explanation must be provided in the applicable Certification. Question 14: The Carrier must specify if a NC Member Satisfaction Survey or NC Provider Survey was used in determining the appointment wait times results. Remember appointment wait times results must be based on the Carrier’s commercial insured managed care membership in NC including border counties. Surveys conducted on another basis i.e. national or regional basis are unacceptable. If both the Carrier and the Intermediary perform surveys to measure the standards for appointment wait times, the Carrier must disclose which survey is considered primary and record the results accordingly. For example, if the Carrier’s survey is primary, the results must be recorded in the Plan’s data grid D15. However, if the Intermediary’s survey is primary, the results must be recorded in the Delegated Entity’s data grid D15. The Carrier is responsible for reviewing the survey to determine if the questions are appropriate to measure its appointment wait times standards. The questions MUST tie back to the actual target. For example, if the target was 10 business days for PCP routine care the appropriate question to ask would be “Were you able to obtain a routine care appointment with your PCP within 10 business days?” General, vague questions like “Were you able to obtain an appointment within a reasonable time?” do not accurately measure the targets; therefore, they are unacceptable. For Quality Management purposes, the Department recommends including questions in the provider and member surveys to measure the following: 1) how long a member sits in the waiting room before being called back to an examination room, and 2) how long a member waits in the examination room before the actual service is rendered by the provider. Question 15: The Carrier must specify the date of the survey identified in Question/Answer #14, the time period the survey covered and the date the Carrier reviewed the survey results. Each of these components must be answered. The Carrier must ensure that survey results were based on services rendered during the specified data year. Managed Care Annual Filing Training Manual 3.2013 Page 62 Question 16: The Carrier must disclose the participation rate (# of members/providers surveyed vs. # of respondents). The Department does not determine the required (valid) participation rate. The number of respondents must be a fair representation of the number of members/providers surveyed. If the number of responses was not enough to adequately analyze the performance, a supplemental method (i.e. reviewing complaints/grievances) must be used in conjunction with the surveys. Remember, only reviewing grievance/complaint data is not a sufficient method. Question 17: If applicable, the Carrier must describe any supplemental method used to measure any appointment wait times type (i.e. Routine, Urgent, Emergent/Emergency) including the date of the report, the time period covered by the report, and the date the Carrier reviewed the report. Each of these components must be answered. A supplemental method must be used if the member/provide survey was invalid due to the lack of respondents. The Insurer must also describe if a different method was used to measure an appointment wait times type (i.e. cold calls to providers’ offices after hours to measure emergency appointment wait times). Question 18: The Carrier must identify any appointment wait time standard which was not met, along with corrective action planned/taken. If the target was narrowly missed (within 5% of target) the Insurer must acknowledge the missed target and indicate that no corrective action plan was necessary. The Insurer will need to continue closely monitoring the network. If the target was missed by more than 5%, the Insurer must describe the corrective action taken/planned by it and/or the Intermediary. If no corrective action was taken/planned, an explanation must be provided in the applicable Certification. Question 19: The Carrier must state if any standard (network density, driving distance, appointment wait times) was revised from the previous data year. The Carrier must disclose the change, the reason for the change and the date the change was approved/adopted by the Carrier. Each of these components must be answered. Before approving/adopting a change for any standard the Carrier must evaluate how the change will affect its members. Lowering a standard for the sole purpose of meeting/exceeding the established goal is unacceptable. Managed Care Annual Filing Training Manual 3.2013 Page 63 Question 20: Full Service Plans: The Carrier must state it or its Intermediary’s (as applicable) policy for paying claims for in-network emergency care, and state if pre-authorization is required; refer to NCGS 58-3-190 for statutory requirements. Single Service Vision Plans: If the benefit is a wellness plan and therefore does not cover emergency care (i.e. vision - exams and hardware only) a statement of such must be provided. Single Service Dental Plans: If the benefit covers emergency services, the Carrier must state it or its Intermediary’s (as applicable) policy for paying claims for in-network emergency care, and state if pre-authorization is required. If pre-authorization is required the Carrier or Intermediary must describe how it is documented in the claim system for proper processing/payment. Question 21: Full Service Plans: The Carrier must state it or its Intermediary’s (as applicable) policy for paying claims for out-of-network emergency care, and state if pre-authorization is required. It must be clear to the Department that claims are being paid at the in-network benefit without penalty to the member; NCGS 58-3-190 and NCGS 58-3-200(d). Single Service Vision Plans: If the benefit is a wellness plan and therefore does not cover emergency care (i.e. vision - exams and hardware only) a statement of such must be provided. Single Service Dental Plans: If the benefit covers emergency services, the Carrier must state it or its Intermediary’s (as applicable) policy for paying claims for out-of-network emergency care, and state if pre-authorization is required. It is the Department’s position, in accordance with 11 NCAC 20.0301 and 20.0302, that the Carrier must maintain an adequate network to provide covered services to its members at the in-network benefit level. Therefore, when in-network providers are not available within the established standards, a Carrier must allow the member to seek services from out-of-network providers at the in-network benefit level. If pre-authorization is required the Carrier or Intermediary must describe how it is documented in the claim system for proper processing/payment. Question 22: The Carrier must state the provisions (addressing authorization and claim payment) made for members when care by a participating provider cannot be received within the availability and accessibility standards, and a member seeks care from a non-participating provider. This includes those counties with membership but no or limited providers. Managed Care Annual Filing Training Manual 3.2013 Page 64 In the description the Carrier must state if pre-authorization/notification is required, how the claim is paid (in-network or out-of-network), whether the member is balance billed, and whether a member has to file a grievance/appeal for reimbursement at the in-network level. Each component must be answered. The Department must ensure that the covered person obtains the covered benefit at no greater cost to the covered person than if the benefit were obtained from participating providers. Question 23: The Carrier must state the actual disclosure provisions communicated to members about receiving care from a non-participating provider when an in-network provider is not reasonably available (within the standards for driving distance and/or appointment wait times). The Carrier must identify the document used during the reporting period which disclosures these provisions (i.e. member handbook, enrollment material, Certificate, etc.) in accordance with the provisions of 11 NCAC 12.1804. Question 24: If the named Intermediary used a subcontracted entity (as identified in the C7 Certification) and its provider network(s) was used to supplement the Plan’s or Intermediary’s network (not a standalone network option) the Carrier must state whether (“Yes” or “No”) the answers and provider availability/accessibility results were inclusive for ALL participating providers. If “No”, an explanation must be provided. Managed Care Annual Filing Training Manual 3.2013 Page 65 13. INTRODUCTION TO THE DATA GRIDS Do not move or delete any rows, grids, text boxes, or other features. Provider Availability and Accessibility standards of, and actual performance against the standards by the Plan and/or Intermediary, as applicable, are reported in data grids D10 through D15. Do not include members living outside of NC and its border counties, and not using the NC network when reporting results in data grids D3, D4/D5, D11, D13 and D15. Data grids have been separated by service plan: Plan Full Service, Plan Single Service (Dental, Vision), Delegated Entity Full Service and Delegated Entity Single Service (Dental, Vision). Interactive functions have been added to facilitate the completion of the data grids. Questions with check boxes appear before most of the data grids. Depending on the answer(s) checked, certain areas or the entire data grid will be shaded, thus eliminating the need to enter “N/A” in all the cells of the data grids. Do not enter any data in a shaded cell. In addition, “ERROR” or “EXPLAIN” messages have been added to alert the Plan or Delegated Entity/Intermediary that a correction is needed and/or an explanation must be provided in the Comment Box. Separate data grids must be completed by each Delegated Entity/Intermediary. Delegated Entity(s)/Intermediary(s) must complete separate data grids for each Carrier (client health plan), and submit supporting data (i.e. GeoAccess Reports, Surveys) to the Carrier for review prior to submission to the Department. A Delegated Entity(s)/Intermediary(s) do not send data grids or other filing information directly to the Department. In addition, HMO and PPO data cannot be combined and submitted together; a separate filing is required for each product type. However, HMOs with a POS product must report combined data unless separate standards apply. Separate data grids must also be completed when the Plan and/or Intermediary offer more than one network option to members. Separate membership by county (data grid D2) and Provider Availability and Accessibility targets (if applicable) and results (data grids D10 through D15), based on the membership of each network, must be reported. For Full-Service filers with dental and/or vision riders available to all members, use the applicable (Plan and/or Delegated Entity) Single Service data grids when reporting data. As there is not a specific provider type column for Pharmacy Benefit Managers, PBMs may use either the column titled “Specialist Physicians (excl. OB/Gyn and MH/CD)” or “Non-MD Providers (excl. MH/CD)” when completing the Delegated Data Grids. Whichever column is selected, the Plan and/or Intermediary must use the same column throughout the filing when reporting data. Do not leave any cells blank; use zero (0) or “N/A” where applicable. Managed Care Annual Filing Training Manual 3.2013 Page 66 The space in the Comment Boxes below the data grids is limited. If more space is needed, use the General Comment Box found after Plan data grid D18 or Delegated Entity data grid D17 or use an attachment. When using an attachment, the Insurer must properly label the document in the email submission and add a reference in the applicable Certification and/or Data Grid. For Delegated Entities performing Grievance and/or Utilization Review only, it is not necessary to continue beyond data grids D4/D5. A message has been added to alert the Delegated Grievance and/or Utilization Review Entity after stoppage. Managed Care Annual Filing Training Manual 3.2013 Page 67 14. COVER PAGES Plan: Check HMO or PPO Single Service Only: Check Dental or Vision* Enter Plan Name and revision date, when applicable (The revision date will help the Department identify the chronological order of data grid submissions.) Full Service Only: Check the applicable plan type(s) as defined by the Affordable Care Act: Grandfathered Plan, Non-Grandfathered Plan or Both Delegated Entity: Enter Name of Delegated Entity/Intermediary and revision date, when applicable (If the Intermediary has more than one network then provide the name of the network after the name of the Intermediary). (The revision date will help the Department identify the chronological order of data grid submissions.) Enter Name of HMO or PPO Carrier Check HMO or PPO Single Service Only: Check Dental or Vision* Check whether the provider network is customized for the Carrier *Single service filers: When “Dental” is checked, all columns associated with Vision will be shaded, indicating those sections of the grid do not require input of data. When “Vision” is checked, all columns associated with Dental will be shaded, indicating those sections of the grid do not require input of data. Plan: “ERROR” messages will occur if the type of product or type of plan box is unchecked or if more than one type of product or type of plan box is checked. Explanations must be provided in the Comment Box for any “ERROR” message or if “N/A” is entered in a cell. Delegated Entity: “ERROR” messages will occur if the type of product or customized network box is unchecked or if more than one type of product or customized network box is checked. Explanations must be provided in the Comment Box for any “ERROR” message or if “N/A” is entered in a cell. Managed Care Annual Filing Training Manual 3.2013 Page 68 15. D1. ENROLLMENT/DISENROLLMENT SUMMARY Do not leave any cells blank; use “0” (zero) whenever applicable. Report commercial-insured membership, including membership covered under Individual and Group contracts sitused in North Carolina including those living out-of-state. Also include membership covered under Group Master Contracts and Group Trusts sitused out-of-state but marketed to North Carolina residents; refer to NCGS 58-3-1 and 58-3-150. Exclude membership covered under self-funded (non-risk), federally insured, Medicare or Medicaid Plans. Membership equals policyholders plus dependents. PPO Insurers that do not track dependents must estimate membership as “Members = (Policyholders) x (2.3). PPO Insurers must indicate in the Comment Box when dependent data is not tracked. For HMO Insurers, the year-end enrollment for the specified data year in data grids D1 and D2 must equal the total of columns 2 and 3 on the “Exhibit of Premiums, Enrollment, and Utilization” for Business in the State of North Carolina” in the Financial Annual Statement. If these counts do not match, then an explanation must be provided in the Comment Box. If the Insurer is an HMO (Health Maintenance Organization), DMO (Dental Maintenance Organization) or VMO (Vision Maintenance Organization), member months and members by HMO and POS product must be entered. An “ERROR” message will appear if the HMO/POS enrollment does not equal the total commercial insured members from the top grid. An “ERROR” message will also appear if the box for member months is left blank. If the Insurer is a PPO, then these fields will be shaded, indicating these sections do not require data input. The Department compares the “beginning” membership reported in the current filing with the “ending” member count from the previous data year’s annual filing. If these totals do not match, an explanation must be provided in the Comment Box. If there has been a “sizable” increase or decrease in membership since the previous data year, an explanation in the Comment Box must be provided. If there has been a sizeable decrease in membership explain if there has been a change in the marketing strategy for NC, and provide any other applicable explanation. If there has been a sizeable increase, explain if there has been a change in the marketing strategy for NC (i.e. introduced a new product/policy). The explanation must also state whether a correlating change in contracted providers occurred and/or revisions made to the Provider Availability & Accessibility standards/P&Ps. “Sizeable” changes will be reviewed on a case-by-case basis. If membership includes Association business, the Insurer must provide the name(s) of the Association(s) in the Comment Box. Managed Care Annual Filing Training Manual 3.2013 Page 69 16. D2. ENROLLMENT BY COUNTY The Plan and/or Intermediary must report the following as of December 31st of the specified data year: Number of NC members by county (A member can live or work in NC) Number of NC Members living in border counties using the NC network Number of NC Members living out-of-state NOT using the NC network Do not leave any cells blank; use “0” (zero) whenever applicable. When zero (0) is entered in data grids D2 (Members by County) and D6 (Providers by County), the font color will appear in red making it easier to compare the two data grids to see which counties have membership but no providers. The total NC membership by county, plus membership living (or working) in border counties and using the NC network, plus membership living outside of NC and not using the NC network, must equal the total membership reported in data grid D1. If not, an “ERROR” message will appear, and an explanation must be provided in the Comment Box. When the Plan and/or Intermediary offer more than one network to members a separate D2 data grid must be completed for each network option. The membership reported in the separate D2 data grids must equal the total membership reported in data grid D1 (as described above). Separate D2, Membership by County, data grids are not applicable to comprehensive plans which include pharmacy and MH/CD benefits (i.e. the network is seamless to the member). Managed Care Annual Filing Training Manual 3.2013 Page 70 17. D3. GRIEVANCES, BY REASON (Not applicable to single service plans) The Plan/Delegated Entity reports in D3 only those written grievances it received during the specified data year. The Grievance data must include “border county” members but not those members living outside of North Carolina covered by a group contract sitused in North Carolina and not utilizing the NC network. Typically if a person resides in North Carolina, he/she needs to be counted, because regardless of where the contract is sitused the member’s benefits are most likely administered based on North Carolina laws. HMOs with a POS product must report combined Grievance data. Do not include 2nd level grievances stemming from 1st level appeals as these must be reported in the Utilization Review data grids D4 and D5. Reviews for “medical necessity” are considered Utilization Review; therefore, must be reported in the Utilization Review data grids D4 and D5. Count 2nd level grievances separately from 1st level grievances. The Plan must indicate whether the Grievance function is performed by the Plan. If “NO” is checked, the entire data grid will be shaded and no input will be required. If “YES” is checked, indicate if “Informal Consideration”, “1st Level Grievances” and/or “2nd Level Grievances” are offered (not whether or not these types of reviews were actually performed during the specified data year). The Delegated Entity must indicate whether the Grievance function is performed by the Delegated Entity. If “NO” is checked, the entire data grid will be shaded and no input will be required. If “YES” is checked, indicate if Informal Consideration, 1st Level Grievances and 2nd Level Grievances are offered (not whether or not these types of reviews were actually performed during the specified data year). Input is required for all applicable non-shaded cells. Do not leave any cells blank use (0) zero wherever applicable. In the first column, enter the applicable entity’s grievance reasons/categories. The reason/category must be more specific than “Other”. Managed Care Annual Filing Training Manual 3.2013 Page 71 If a “Limitation & Exclusion” (or similar wording) category is used then verification must be made in the Comment Box if the decisions were rendered solely on the basis that the health benefit plan does not provide benefits for the health care service that was in question. If the exclusion of the specific service requested is clearly stated in the policy/certificate of coverage, the decision(s) must not be included in the grievance data. If a grievance reason/category was “annual or lifetime limits”, further explanation must be provided in the Comment Box regarding the plan type and circumstances of each case (reason for denial and outcome). The types of Grievance reviews checked must match those found in the C3a. Compliance Certification for Grievance Procedures/C3b. Compliance Certification for External Review related to Grievances and/or C4a. Compliance Certification for Delegated Grievance Procedures/C4b. Compliance Certification for Delegated External Review related to Grievances. “ERROR” messages will appear if a review type box is unchecked or if both “Yes” and “No” boxes are checked for the same review type. Explanations for any “NO” answers must be provided in the Comment Box. An “EXPLAIN” message will appear if any of the column totals equal zero (0). An explanation (acknowledgement) for no activity must be provided in the Comment Box. If data appears to indicate disproportionately small/large number of grievances to membership or if there has been significant changes in the reported grievances, an explanation must be provided in the Comment Box. For example, may have a large number of reported 1st level grievances but have no 2nd level grievances (or overturned decisions in favor of member). In this situation, based on the “zero activity” explanation, the Department may request a copy of the Grievance P&Ps, and/or Grievance related form/template letters to review for compliance. Managed Care Annual Filing Training Manual 3.2013 Page 72 18. D4. UTILIZATION REVIEW DECISIONS, BY REVIEW TYPE / D5. UTILIZATION REVIEW DECISIONS, BY SERVICE TYPE (Not applicable to single service plans) The Plan/Delegated Entity reports in D4/D5 only those Utilization Reviews (UR) and/or External Reviews it conducted during the specified data year. Utilization Review/External Review data must include “border county” members but not those members living outside of North Carolina covered by a group contract sitused in North Carolina and not utilizing the NC network. Typically if a person resides in North Carolina he/she needs to be counted because regardless of where the contract is sitused the member’s benefits are most likely administered based on North Carolina laws. By definition, Utilization Reviews and Noncertifications involve “medical necessity” determinations. If the Plan and/or Delegated Entity do not perform precertification, the company may still review for “medical necessity” and this type of grievance is considered UR. Therefore, “medical necessity” reviews must be recorded in data grids D4 and D5 (not data grid D3), even if the claim is reviewed retrospectively. Do not include administrative denials (non-covered services, benefit limits reached, lack of preauthorization, etc.). The reported External Review data is specifically related to the statutorily mandated External Review Program not for any internal review process of the Plan or Delegated Entity (report the number of cases submitted to the Department’s External Review Program/Smart NC). Count 2nd level UR grievances separately from 1st level appeals. When reporting “Decisions in Favor of Member”, count only those for which the appeal was fully resolved in the member’s favor. Do not count those appeals which are partially overturned in the member’s favor. HMOs with a POS product must report combined UR data, including External Review. The Plan must indicate the UR functions performed by the Plan: “Utilization Reviews”, “Informal Reconsideration”, “Noncertification Appeals 1st Level”, “Noncertification Appeals 2nd Level” and “External Reviews”. For any “NO” answer, the corresponding column(s) in the data grids will be shaded, and no input will be required. If “YES” is checked for “UR”, the Plan must indicate the types of reviews available (not whether or not these types of reviews were actually performed during the specified data year): “Prospective”, “Concurrent” and “Retrospective”. For any “NO” answer, the corresponding row(s) will be shaded, and no input will be required. If “No” is checked for Noncert Appeals – 2nd Level, the Plan will be asked if this function was delegated/never offered or discontinued. If discontinued, the date of discontinuance must be entered otherwise an “ERROR” message will appear. Managed Care Annual Filing Training Manual 3.2013 Page 73 The Delegated Entity must indicate the UR functions performed by the Delegated Entity: “Utilizations Reviews”, “Informal Reconsideration”, “Noncertifications Appeals 1st Level”, “Noncertification Appeals 2nd Level” and “External Reviews”. For any “NO” answer, the corresponding column(s) will be shaded, and no input will be required. If “YES” is checked for “UR”, the Delegated Entity must indicate the types of reviews available (not whether or not these types of reviews were actually performed during the specified data year): “Prospective”, “Concurrent” and “Retrospective”. For any “NO” answer, the corresponding row(s) will be shaded, and no input will be required. If “No” is checked for Noncert Appeals – 2nd Level, the Delegated Entity will be asked if this function was not delegated/never offered or discontinued. If discontinued, the date of discontinuance must be entered otherwise an “ERROR” message will appear. Input is required for all applicable non-shaded cells. Do not leave any cells blank use (0) zero wherever applicable. The types of reviews checked must match those found in the C5a. Compliance Certification for Utilization Review/C5b. Compliance Certification for External Review and/or C6a. Compliance Certification for Delegated Utilization Review/C6b. Compliance Certification for Delegated External Review. “ERROR” messages will appear if a review type or type of UR box is unchecked or if both “Yes” and “No” boxes are checked for the same review type or type of UR. Explanations for any “NO” answers must be provided in the Comment Box. An “EXPLAIN” message will appear if any of the column totals equal zero (0). An explanation (acknowledgement) for no activity must be provided in the Comment Box. A “WARNING” message will appear if “No” is checked for “Noncert Appeals – 2nd Level” but the Plan or Delegated Entity did not check whether the function was (not) delegated/never offered or discontinued. An “ERROR” message will appear if “No” is check for “Noncert Appeals – 2nd Level” and the “Discontinued offering 2nd level grievance process for UR matters” box is checked but the date of discontinuance was not entered. “ERROR” message will appear if the column totals in data grid D4 do not match the corresponding column totals in data grid D5. An explanation to address the discrepancy must be provided in the Comment Box. If data appears to indicate disproportionately small/large number of noncertifications/appeals to membership or if there has been significant changes in the reported UR, an explanation must be provided in the Comment Box. For example, no reported data but have external review activity, or may have a large number of reported appeals and 2nd level grievances but have no external review activity. In these situations, based on the “no activity” explanation provided, the Department may request a copy of the UR P&Ps, and/or UR related form/template letters to review for compliance. Managed Care Annual Filing Training Manual 3.2013 Page 74 19. D6. PROVIDERS BY COUNTY Provider, including border counties, data must be as of December 31st of the specified data year. Do not count the same provider more than once within the same county. Count only those providers for whom credentialing and contracting have been completed and are “in-network” for the members. Full Service Only: A listing of all contracted hospitals (i.e. inpatient facilities, Acute Care, Tertiary, Children’s Hospitals, etc.) by county (including border counties) must be provided in the Comment Box. If additional space is needed, an attachment may be used. How to Categorize Providers: “Service providers” such as DME, home health, home infusion, hospice, prosthetics/orthotics, laboratories must be counted as non-MD providers. Nurse practitioners, physician assistants and nurse midwives who do not practice independent of supervising physicians must be counted with “MDs” because they are supporting the MDs’ practice. It is appropriate to categorize them on the basis of the type of physician they support. A group of nurse practitioners who are in a standalone practice and not supporting an MD practice must be classified as non-MDs. Even though they are physician extenders, they would not be considered MDs for the basis of reporting since they technically do not hold a MD’s license. Hospital-based providers and other providers which participate under a facility contract (i.e. emergency room physicians, radiologists, anesthesiologists, etc.) and not separately listed in the provider directory must be excluded in the MD count. Providers who are strictly OB or strictly Gyn must be grouped in the OB/Gyn category. Hospitals that offer outpatient services must be included in the count for Outpatient Facilities (excl. MH/CD). Effective DY2012: The MH/CD columns from data grids D6 through D13, and D16/D17 have been renamed for clarification. The Insurer/Intermediary must report the number of “MH/CD Inpatient Facilities Pre-Stabilization” and the number of “MH/CD Inpatient Facilities PostStabilization”. Pre-Stabilization includes services rendered in a hospital setting including Emergency Room, Observation Stay and Temporary Inpatient Stay in a hospital. PostStabilization includes services rendered in a MH/CD facility. If a facility offers both prestabilization and post stabilization, the facility must be counted in both categories. Managed Care Annual Filing Training Manual 3.2013 Page 75 Full Service and Single Service: A listing of border counties must be provided in the Comment Box. “Border Counties” is for contracted/credentialed providers participating in the Plan/Intermediary’s network, but located across state lines in counties contiguous to the NC border (SC, VA, TN, and GA). Full Service: The Plan must check which network is used. If “Intermediary Network Providers” is checked, data grids D6 through D9 will be shaded, and no input will be required. If “Plan Directly Contracted Providers” is selected, then the Plan must check the provider type(s) included in the network: “All Provider Types”, “All Provider Types Exclude MH/CD”, or “MH/CD Only”. If “All Provider Types” is checked, enter the provider counts by county for all Provider Types. If “All Provider Types Exclude MH/CD” is checked, then the MH/CD columns in data grids D6 through D9 will be shaded, and no input will be required. Enter in the provider counts by county for all other provider types. If “MH/CD Only” is checked, then all other Provider Types columns in data grids D6 through D9 will be shaded, and no input will be required. Enter in the provider counts by county for MH/CD providers. The Intermediary must check which network is used. If “Plan Directly Contracted Providers” is checked, data grids D6 through D9 will be shaded, and no input will be required. If “Intermediary Network Providers” is selected, then the Intermediary must check the provider types included in the network: “All Provider Types”, “All Provider Types Exclude MH/CD”, or “MH/CD Only”. If “All Provider Types” is checked, enter in the provider counts by county for all Provider Types. If “All Provider Types Exclude MH/CD” is checked, then the MH/CD columns in data grids D6 through D9 will be shaded, and no input will be required. Enter in the provider counts by county for all other provider types. If “MH/CD Only” is checked, then all other Provider Types columns in data grids D6 through D9 will be shaded, and no input will be required. Enter in the provider counts by county for MH/CD providers. Single Service: The Plan must check which network is used. If “Intermediary Network Providers” is checked, data grids D6 through D9 will be shaded, and no input will be required. If “Plan Directly Contracted Providers” is checked, enter in the provider counts by county for all Provider Types. Managed Care Annual Filing Training Manual 3.2013 Page 76 The Intermediary must check which network is used. If “Plan Directly Contracted Providers” is checked, data grids D6 through D9 will be shaded, and no input will be required. If “Intermediary Network Providers” is checked, enter in the provider counts by county for all Provider Types. Full Service and Single Service: Do not leave any cells blank; use “0” (zero) whenever applicable. Vision: Do not count retail store employees. Rider(s): Do not include separate carve-out networks of specialty providers for riders if all members do not have access to those providers. HMOs with a POS product must report combined network data (counting each provider only once). When zero (0) is entered in data grids D2 (Membership by County) and D6 (Providers by County) the font color will appear in red making it easier to compare the two data grids to see which counties have membership but no providers. “ERROR” messages will occur if the type of network or type of network providers box is unchecked or if more than one type of network or type of network providers box is checked. Explanations must be provided in the Comment Box for any “ERROR” message or if “N/A” is entered in a cell. Managed Care Annual Filing Training Manual 3.2013 Page 77 20. D7: UNIQUE PROVIDERS ON NETWORK As of December 31st of the current specified data year and December 31st of the previous specified data year, report the number of “unique” providers (including border county providers), counting each provider only once even if the provider has office locations in multiple counties, or multiple locations in the same county. Count only those providers for whom credentialing and contracting have been completed and are “in-network” for the members. This data grid may be completely shaded depending on which network (Plan or Intermediary) is checked in data grid D6. In addition for Full Service, depending on which provider types are included in the network, the columns for MH/CD or the columns for all other Provider Types will be shaded, and no input will be required. Do not leave any cells blank; use “0” (zero) whenever applicable. Vision: Do not count retail store employees. Rider(s): Do not include separate carve-out networks of specialty providers for riders if all members do not have access to those providers. HMOs with a POS product must report combined network data counting each “unique” provider only once. The current filing’s year-end total must equal last year’s year-end total plus the providers joining the network (data grid D9), minus the providers leaving the network (data grid D8). If these calculations do not reconcile, an “ERROR” message beneath the applicable column(s) will appear, and an explanation must be provided in the Comment Box. If there has been a significant increase or decrease in the number of unique providers since the previous data year, an explanation must be provided in the Comment Box, including whether any adjustments were made to the provider availability and accessibility standards/policy. If “YES”, submit a copy(s) of the revised standard(s)/policy(s) for the Department’s records. The revised P&Ps reflecting the adjusted standard and the policy revision must be addressed in the applicable questions in Certification(s) C8 and/or C9. The Department compares the previous data year December 31st totals for each provider type reported in the current filing with totals in the prior filing for the same period. If the totals are not the same, an explanation must be provided in the Comment Box. For example, current filing for 2013 (data year 2012) the number of unique PCPs reported as of December 31, 2012 was 800 but in last year’s filing for 2012 (data year 2011) the number of unique PCPs reported for December 31, 2012 was 680, an explanation must be provided in the Comment Box. Managed Care Annual Filing Training Manual 3.2013 Page 78 21. D8: UNIQUE PROVIDERS LEAVING NETWORK Report the number of “unique” providers (including border county providers) that left the network (not a location) during the specified data year, counting each provider only once even if the provider has sites in multiple counties, or multiple locations in the same county. This data grid may be completely shaded depending on which network (Plan or Intermediary) is checked in data grid D6. In addition for Full Service, depending on which provider types are included in the network, the columns for MH/CD or the columns for all other Provider Types will be shaded, and no input will be required. Do not leave any cells blank; use “0” (zero) whenever applicable. Vision: Do not count retail store employees. Rider(s): Do not include separate carve-out networks of specialty providers for riders if all members do not have access to those providers. HMOs with a POS product must report combined network data (counting each provider terminating only once). Terminations: Involuntary means terminated with cause (poor performance, unethical conduct, etc.). Voluntary means terminated via resignation, retirement, relocation, etc. The Company may need to contact its Provider Contracting/Credentialing or Quality Management for this information. The Insurer must ensure its system is programmed to properly report the terminating providers as defined. An “ERROR” message will appear indicating that the Plan/Intermediary must provide an explanation in the Comment Box if the total providers in any column leaving the network represents 10% or more of the total unique providers in the corresponding column in data grid D7. The explanation must include clarification as to whether the reduction occurred at one time and describe any corrective action taken/planned. Refer to the Corrective Action Plan requirements outlined in the C8/C9 Certifications. It is the Insurer’s responsibility to track the growth and reduction of its and/or the Intermediary’s network. While there may be a net growth to the network at the end of year, it does not exempt the Insurer’s responsibility to make certain that its members have sufficient access to care throughout the year. Insurers must review the network(s) to determine if it and/or the Intermediary are maintaining sufficient coverage. Managed Care Annual Filing Training Manual 3.2013 Page 79 The review can include determining if a reduction has occurred in a particular service area which includes a geographic location, a particular provider type or the network as a whole. The Insurer must ensure that no harm (i.e. claims processing/payment) to members occurs when members seek care from non-participating providers because the in-network is insufficient and in-network providers are unable to render services within the provider availability and accessibility standards. 11 NCAC 20.0602(2) requires an HMO to submit written notification to the Department (Life & Health Division) within 15 days following reductions in the number of providers that exceed 10% of the total number of providers in a particular service area. When applicable, the HMO must provide in the Comment Box the NCDOI/SERFF tracking number for the filing. Managed Care Annual Filing Training Manual 3.2013 Page 80 22. D9: UNIQUE PROVIDERS JOINING NETWORK Report the number of “unique” providers (including border county providers) joining the network during the specified data year, counting each provider only once, even if the provider has office locations in multiple counties, or in multiple locations in the same county. Count only those providers for whom credentialing and contracting have been completed and are “innetwork” for the members. This data grid may be completely shaded depending on which network (Plan or Intermediary) is checked in data grid D6. In addition for Full Service, depending on which provider types are included in the network, the columns for MH/CD or the columns for all other Provider Types will be shaded, and no input will be required. Do not leave any cells blank; use “0” (zero) whenever applicable. Vision: Do not count retail store employees. Rider(s): Do not include separate carve-out networks of specialty providers for riders if all members do not have access to those providers. HMOs with a POS product must report combined network data (counting each provider joining the network only once). Managed Care Annual Filing Training Manual 3.2013 Page 81 23. D10. NETWORK DENSITY, TARGETS BY PROVIDER TYPE AND GEOGRAPHIC AREA Full Service: Plan Data Grid D10: The Plan must indicate if it sets the targets for: “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the targets for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the targets for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the targets for MH/CD providers. If “NO” is checked, the entire data grid will be shaded and no input will be required. Intermediary Data Grid D10: The Intermediary must indicate if it sets the targets for: “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the targets for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the targets for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the targets for MH/CD providers. If “NO” is checked, the entire data grid will be shaded, and no input will be required. Single Service: Plan Data Grid D10: The Plan must indicate if it sets the targets. If “YES” is checked, then enter the targets for all provider types specified in data grid D10. If “NO” is checked, the data grid will be shaded, and no input will be required. Intermediary Data Grid D10: The Intermediary must indicate if it sets the targets. If “YES” is checked, enter the targets for all provider types specified in data grid D10. If “NO” is checked, the data grid will be shaded, and no input will be required. Single service filers must specify in the Comment Box if targets are based on all “participating providers”. Managed Care Annual Filing Training Manual 3.2013 Page 82 Full Service and Single Service: The Department will NOT convert or interpret targets. The Department may refer to the Insurer/Intermediary’s standards on file with the Life & Health Division. The standards reported must match those in the formalized written Provider Availability & Accessibility P&Ps applicable for the specified data year. HMOs with a POS product must report combined network targets unless separate targets apply. Rider(s): Do not include separate carve-out networks of specialty providers for riders if all members do not have access to those providers. Enter the Geographic Area(s) in the far-left column of the grid. If the targets differ by geographic areas, make sure that the areas are appropriate i.e. Statewide, Urban/Suburban/Rural. Standards must be expressed as a ratio (2:100) or spelled out (2 providers for every 100 members). The same ratio format must be used for all geographic areas and provider types. If the standards and/or provider types are not reportable within the grid, use the Comment Box to report the data. While the Department does not set targets or determine industry norms, the Department will question targets outside of the industry norm or improperly set. Examples of improperly set targets are using driving distance rather than provider-to-member data or using NC census data and/or the total of all licensed providers in NC including by provider type; NCGS 58-3191(a)(4). When evaluating “industry norms” the Department reviews insurers with similar size membership. Standards can vary depending on the type of carrier and membership. Full-service carriers with large membership may have standards ranging from 1 PCP per 100 members to 1:1,000 members. Carriers with medium membership and small/medium networks may have standards ranging from 1:500 to 1:1,200. Standards for mental health/chemical dependency providers may range from 1:500 to 1:5,000. Specialist standards can range from 1:2,000 members to 1:10,000, and facilities, including mental health/chemical dependency, can range from 1:10,000 to 1:50,000. The premise is that Specialty (including MH/CD) providers are limited; therefore, the ratio can be higher than general type providers (i.e. PCPs, General Dentists, Optometrists). Full-Service carriers must specify in the Comment Box the type of providers included in the Specialist Physicians and Non-MD Providers columns. The Carrier MUST report at least the top 10 utilized provider types applicable to the Specialist Physicians and Non-MD Providers columns. When listing the provider types in the Comment Box it must be clear to the Department whether the same standard applies to all or if standards vary (each standard must be disclosed). Managed Care Annual Filing Training Manual 3.2013 Page 83 “ERROR” messages will occur if the network type is not checked, if more than one network type is checked and/or if a provider type cell within a geographic area is left blank. Explanations must be provided in the Comment Box for any “ERROR” message or if “N/A” is entered in a cell. Managed Care Annual Filing Training Manual 3.2013 Page 84 24. D11. NETWORK DENSITY, ACTUAL PERFORMANCE, BY PROVIDER TYPE AND GEOGRAPHIC AREA Full Service: Plan Data Grid D11: The Plan must indicate if it monitors the targets for: “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the results for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the results for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the results for MH/CD providers. If “NO” is checked, the entire data grid will be shaded, and no input will be required. Intermediary Data Grid D11: The Intermediary must indicate if it monitors the targets for “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the results for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the results for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the results for MH/CD providers. If “NO” is checked, the entire data grid will be shaded, and no input will be required. Single Service: Plan Data Grid D11: The Plan must indicate if it monitors the targets. If “YES” is checked, enter the results for all provider types specified in data grid D11. If “NO” is checked, the data grid will be shaded, and no input will be required. Intermediary Data Grid D11: The Intermediary must indicate if it monitors the targets. If “YES” is checked, enter the results for all provider types specified in data grid D11. If “NO” is checked, the data grid will be shaded, and no input will be required. Managed Care Annual Filing Training Manual 3.2013 Page 85 Full Service and Single Service: The Department will NOT convert or interpret results. HMOs with a POS product must report combined network results unless separate targets apply. Rider(s): Do not include separate carve-out networks of specialty providers for riders if all members do not have access to those providers Enter the specified Geographic Area(s) in the far-left column of the grid (must be the same area(s) as identified in data grid D10). Results must be recorded in the same manner as used in setting the target(s) in data grid D10 (i.e. results must be converted to the ratio [per 1,000 members] as specified in data grid D10). If the results and/or provider types are not reportable within the grid, use the Comment Box to report the data. Full-Service carriers using the data grid D11 Comment Box must report results for Specialist Physicians and Non-MD Providers as specified in the data grid D10 Comment Box. Results must be based on the Carrier’s NC membership (home or work address), including “border county members”, and NC contracted providers including border counties, as of December 31st of the specified data year. This does not mean the Plan/Intermediary needs to run the report exactly on December 31st, but when running the report, the period ending date must be December 31st of the specified data year. Members living outside of NC and NOT using the NC provider network must not be included when measuring network density results. The Plan and/or Intermediary must disclose in the Comment Box the actual calculations and properly identify each component to support the reported results or attach a copy of the actual report. When submitting a GeoAccess or similar zip code analysis report, it must be clear to the Department how the results were calculated. Remember, the Insurer must identify any standard which was not met in the applicable C8 or C9 Certification. If the target was narrowly missed (within 5% of target) the Insurer must acknowledge in the applicable Certification the missed target and indicate that no corrective action plan was necessary. The Insurer will need to continue closely monitoring the network. If the target was missed by more than 5%, the Insurer must describe in the applicable Certification the corrective action taken/planned by it and/or the Intermediary. If no corrective action was taken/planned, an explanation must be provided in the applicable Certification. “ERROR” messages will occur if the network type is not checked, if more than one network type is checked and/or if a provider type cell within a geographic area is left blank. Explanations must be provided in the Comment Box for any “ERROR” message or if “N/A” is entered in a cell. Managed Care Annual Filing Training Manual 3.2013 Page 86 25. D12. DRIVING DISTANCE, TARGETS BY PROVIDER TYPE AND GEOGRAPHIC AREA Full Service: Plan Data Grid D12: The Plan must indicate if it sets the targets for: “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the targets for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the targets for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the targets for MH/CD providers. If “NO” is checked, the entire data grid will be shaded and no input will be required. Intermediary Data Grid D12: The Intermediary must indicate if it sets the targets for: “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the targets for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the targets for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the targets for MH/CD providers. If “NO” is checked, the entire data grid will be shaded, and no input will be required. Single Service: Plan Data Grid D12: The Plan must indicate if it sets the targets. If “YES” is checked, then enter the targets for all provider types specified in data grid D12. If “NO” is checked, the data grid will be shaded, and no input will be required. Intermediary Data Grid D12: The Intermediary must indicate if it sets the targets. If “YES” is checked, enter the targets for all provider types specified in data grid D12. If “NO” is checked, the data grid will be shaded, and no input will be required. Single service filers must specify in the Comment Box if targets are based on all “participating providers”. Managed Care Annual Filing Training Manual 3.2013 Page 87 Full Service and Single Service: The Department will NOT convert or interpret targets. The Department may refer to the Insurer/Intermediary’s standards on file with the Life & Health Division. The standards reported, including overall target(s) (i.e. 90% of members with access to 1 PCP within 10 miles), must match the formalized written Provider Availability & Accessibility P&Ps applicable for the specified data year. HMOs with a POS product must report combined network targets unless separate targets apply. Rider(s): Do not include separate carve-out networks of specialty providers for riders if all members do not have access to those providers. Enter the Geographic Area(s) in the far-left column of the grid. If the targets differ by geographic areas, make sure that the areas are appropriate i.e. Statewide, Urban/Suburban/Rural. Standards must be expressed as a ratio (1:10) or spelled out (1 provider within 10 miles), and the percentage of the target, if less than 100%, must be stated in the Comment Box. If the standards and/or provider types are not reportable within the grid, use the Comment Box to report the data. While the Department does not set targets or determine industry norms, the Department will question targets outside the industry norm or improperly set. Examples of improperly set targets are using provider-to-member ratios rather than driving distance or using NC census data and/or the total of all licensed providers in NC including by provider type; NCGS 58-3-191(a)(4). When evaluating “industry norms” the Department reviews insurers with similar size membership. Standards may vary depending on the type of carrier and membership. Full-service carriers with large networks and large memberships or large network and medium membership may set more aggressive targets. Industry standards normally range from 1 PCPs, Pediatricians and OB/GYNs within 30 miles or less for urban and suburban areas while rural areas may range up to 45 miles. For carriers with small membership and networks, targets may use a statewide target where standards may range up to 45 miles. For Specialists, the standards may range up to 60 miles. Single-service carriers do not typically have very large networks, so the standards reflect the lack of providers. This is especially true for rural areas. Typical standards may be a general dentist or optometrist within 30 miles, a specialty dentist (orthodontists, periodontists, oral surgeons, ophthalmologists, etc.) within 60 to 75 miles. Full-Service carriers must specify in the Comment Box the type of providers included in the Specialist Physicians and Non-MD Providers columns. At a minimum the Carrier MUST report the top 10 utilized provider types applicable to the Specialist Physicians and Non-MD Providers columns. When listing the provider types in the Comment Box it must be clear to the Department whether the same standard applies to all or if standards vary (each standard must be disclosed). Managed Care Annual Filing Training Manual 3.2013 Page 88 “ERROR” messages will occur if the network type is not checked, if more than one network type is checked and/or if a provider type cell within a geographic area is left blank. Explanations must be provided in the Comment Box for any “ERROR” message or if “N/A” is entered in a cell. Managed Care Annual Filing Training Manual 3.2013 Page 89 26. D13. DRIVING DISTANCE, ACTUAL PERFORMANCE BY PROVIDER TYPE AND GEOGRAPHIC AREA Full Service: Plan Data Grid D13: The Plan must indicate if it monitors the targets for: “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the results for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the results for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the results for MH/CD providers. If “NO” is checked, the entire data grid will be shaded, and no input will be required. Intermediary Data Grid D13: The Intermediary must indicate if it monitors the targets for “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the results for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the results for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the results for MH/CD providers. If “NO” is checked, the entire data grid will be shaded, and no input will be required. Single Service: Plan Data Grid D13: The Plan must indicate if it monitors the targets. If “YES” is checked, enter the results for all provider types specified in data grid D11. If “NO” is checked, the data grid will be shaded, and no input will be required. Intermediary Data Grid D13: The Intermediary must indicate if it monitors the targets. If “YES” is checked, enter the results for all provider types specified in data grid D11. If “NO” is checked, the data grid will be shaded, and no input will be required. Managed Care Annual Filing Training Manual 3.2013 Page 90 Full Service and Single Service: The Department will NOT convert or interpret results. HMOs with a POS product must report combined network results unless separate targets apply. Rider(s): Do not include separate carve-out networks of specialty providers for riders if all members do not have access to those providers Enter the specified Geographic Area(s) in the far-left column of the grid (must be the same area(s) as identified in data grid D12). Results must be recorded as the percentage of members that fell within the targets identified in data grid D12. Remember, the assumed percentage of members falling within the specified targets is 100% unless otherwise stated in the data grid D12 Comment Box. If the results and/or provider types are not reportable within the grid, use the Comment Box to report the data. Full-Service carriers using the data grid D13 Comment Box must report results for Specialist Physicians and Non-MD Providers as specified in the data grid D12 Comment Box. Results must be based on the Carrier’s NC membership (home or work address), including “border county members”, and NC contracted providers including border counties, as of December 31st of the specified data year. . This does not mean the Plan/Intermediary needs to run the report exactly on December 31st, but when running the report, the period ending date must be December 31st of the specified data year. Members living outside of NC and NOT using the NC provider network must not be included when measuring driving distance results. In the Comment Box, the Insurer/Intermediary must specify the (report) components of how the results were developed: 1. Must disclose if the results were based on members, employees, etc. 2. Must disclose if the results were based on home address or work address. 3. Must disclose if the results were based on the number of unique providers (counting each provider once regardless of the number of locations i.e. data grid D7), the number of providers for each county (counting each county once regardless of the number of locations in the same county i.e. data grid D6), or the total number of locations (counting each provider’s location(s) in all counties). Remember, the Insurer must identify any standard which was not met in the applicable C8 or C9 Certification. If the target was narrowly missed (within 5% of target) the Insurer must acknowledge in the applicable Certification the missed target and indicate that no corrective action plan was necessary. The Insurer will need to continue closely monitoring the network. Managed Care Annual Filing Training Manual 3.2013 Page 91 If the target was missed by more than 5%, the Insurer must describe in the applicable Certification the corrective action taken/planned by it and/or the Intermediary. If no corrective action was taken/planned, an explanation must be provided in the applicable Certification. “ERROR” messages will occur if the network type is not checked, if more than one network type is checked and/or if a provider type cell within a geographic area is left blank. Explanations must be provided in the Comment Box for any “ERROR” message or if “N/A” is entered in a cell. Managed Care Annual Filing Training Manual 3.2013 Page 92 27. D14. APPOINTMENT WAIT TIMES, TARGETS BY PROVIDER TYPE AND APPOINTMENT TYPE Full Service: Plan Data Grid D14: The Plan must indicate if it sets the targets for: “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the targets for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the targets for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the targets for MH/CD providers. If “NO” is checked, the entire data grid will be shaded and no input will be required. Intermediary Data Grid D14: The Intermediary must indicate if it sets the targets for: “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the targets for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the targets for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the targets for MH/CD providers. If “NO” is checked, the entire data grid will be shaded, and no input will be required. Single Service: Plan Data Grid D14: The Plan must indicate if it sets the targets. If “YES” is checked, then enter the targets for all provider types specified in data grid D12. If “NO” is checked, the data grid will be shaded, and no input will be required. Intermediary Data Grid D14: The Intermediary must indicate if it sets the targets. If “YES” is checked, enter the targets for all provider types specified in data grid D12. If “NO” is checked, the data grid will be shaded, and no input will be required. Single service filers must specify in the Comment Box if targets are based on all “participating providers”. Managed Care Annual Filing Training Manual 3.2013 Page 93 Full Service and Single Service: The Department will NOT convert or interpret targets. The Department may refer to the Insurer/Intermediary’s standards on file with the Life & Health Division. The standards reported, including overall target(s) (i.e. 90% of members able to obtain a routine appointment within 10 business days), must match the formalized written Provider Availability & Accessibility P&Ps applicable for the specified data year. HMOs with a POS product must report combined network targets unless separate targets apply. Rider(s): Do not include separate carve-out networks of specialty providers for riders if all members do not have access to those providers. The Plan/Intermediary must specify the measurement of the targets: business days, calendar days, weeks, hours. For purposes of the managed care annual filing, the appointment wait time is not the time a member spends in a provider’s waiting room but the elapsed time it takes between scheduling an appointment and the actual appointment date. The Department will question if the targets appear to be outside the industry norm or improperly set. While the Department does not set targets or determine industry norms, the Department will question targets outside the industry norm or improperly set. Examples of improperly set targets are using time sitting in the waiting room or using NC census data and/or the total of all licensed providers in NC including by provider type; NCGS 58-3-191(a)(4). When evaluating “industry norms” the Department reviews insurers with similar size membership. Full-service Emergent (Emergency) standards are based on 24 hours per day, 7 days a week, and the target percentage of the standard must be 100%. Emergent (Emergency) standards for MH/CD can range from immediate up to 8 hours. The Department understands that it may be difficult to adequately measure “Emergency” appointment wait times through a survey methodology because members are instructed to call 9-1-1 or go to the nearest Emergency Room. Therefore, using a different method such as cold calls to the providers’ offices may be a better tool to measure performance. Cold calls should take place after hours to ensure providers have the “emergency” provisions as set forth in their provider agreement (i.e. instructions to call 9-1-1 or go to the nearest Emergency Room, answering service, voicemail, paging system, etc.). Urgent standards are normally within 24 to 48 hours with 72 hours being the outermost limit. Routine standards can vary depending on the type of carrier (full-service or single-service). For full-service carriers, routine appointment wait times will normally range from 10 to 30 calendar days for PCPs to 60 calendar days for Specialists although standards for Specialists can vary depending on whether the carrier makes a distinction between high-volume and low volume specialists. For services such as annual physicals and screenings, the standards can range up to 90 calendar days. Managed Care Annual Filing Training Manual 3.2013 Page 94 Full-Service carriers must specify in the Comment Box the type of providers included in the Specialist Physicians and Non-MD Providers columns. At a minimum the Carrier MUST report the top 10 utilized provider types applicable to the Specialist Physicians and Non-MD Providers columns. When listing the provider types in the Comment Box it must be clear to the Department whether the same standard applies to all or if standards vary (each standard must be disclosed). “ERROR” messages will occur if the network type is not checked, if more than one network type is checked and/or if a provider type cell within an appointment type is left blank. Explanations must be provided in the Comment Box for any “ERROR” message or if “N/A” is entered in a cell. Managed Care Annual Filing Training Manual 3.2013 Page 95 28. D15. APPOINTMENT WAIT TIMES, ACTUAL PERFORMANCE BY PROVIDER TYPE AND APPOINTMENT TYPE Full Service: Plan Data Grid D15: The Plan must indicate if it monitors the targets for: “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the results for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the results for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the results for MH/CD providers. If “NO” is checked, the entire data grid will be shaded, and no input will be required. Intermediary Data Grid D15: The Intermediary must indicate if it monitors the targets for “All Provider Types”, “All Provider Types Exclude MH/CD”, “MH/CD Only” or “No”. If “All Provider Types” is checked, enter the results for all provider types specified in the data grid. If “All Provider Types Exclude MH/CD” is checked, the MH/CD columns will be shaded, and no input will be required. Enter the results for all other provider types. If “MH/CD Only” is checked, all other provider type columns will be shaded, and no input will be required. Enter the results for MH/CD providers. If “NO” is checked, the entire data grid will be shaded, and no input will be required. Single Service: Plan Data Grid D15: The Plan must indicate if it monitors the targets. If “YES” is checked, enter the results for all provider types specified in data grid D11. If “NO” is checked, the data grid will be shaded, and no input will be required. Intermediary Data Grid D15: The Intermediary must indicate if it monitors the targets. If “YES” is checked, enter the results for all provider types specified in data grid D11. If “NO” is checked, the data grid will be shaded, and no input will be required. Managed Care Annual Filing Training Manual 3.2013 Page 96 Full Service and Single Service: The Department will NOT convert or interpret results. HMOs with a POS product must report combined network results unless separate targets apply. Rider(s): Do not include separate carve-out networks of specialty providers for riders if all members do not have access to those providers Results must be recorded as the percentage of members that fell within the targets identified in data grid D14. Remember, the assumed percentage of members falling within the specified targets is 100% unless otherwise stated in the data grid D14 Comment Box. If the results and/or provider types are not reportable within the grid, use the Comment Box to report the data. Full-Service carriers using the data grid D15 Comment Box must report results for Specialist Physicians and Non-MD Providers as specified in the data grid D14 Comment Box. When using a member survey to measure appointment wait times, results must be based on the Plan’s NC membership, including “border county” members, and services rendered during the specified data year. When using a provider survey to measure appointment wait times results must be based on “in-network” NC providers, including border county providers. The provider survey must be conducted during the specified data year. If surveys are performed on a more frequent basis than annual, the Insurer/Intermediary must report the overall results for the specified data year. The Insurer MUST ensure that the results are based on a valid, accurate survey. As previously mentioned in the C8/C9 Certifications, member/provider survey questions must be specific to the standards to adequately measure the actual performance. General or vague questions like “Were you able to obtain an appointment within a reasonable time?” are unacceptable. The survey questions must be specific to each appointment type and provider type (if targets are not based on all participating providers). For example, if the routine appointment wait time for PCPs was 10 business days, the appropriate survey question would be: “Were you able to obtain a routine appointment with your PCP within 10 business days?” If the Insurer or Intermediary does not receive enough responses for a valid survey, then this methodology must be supplemented with either cold calls and/or reviewing grievance/complaint data. It is the Department’s position that relying solely on reviews of members complaints/grievances does not constitute comprehensive monitoring of appointment wait times, although it can be a helpful component in tracking issues, and used as a supplemental method to surveys. Remember, the Insurer must identify any standard which was not met in the applicable C8 or C9 Certification. If the target was narrowly missed (within 5% of target) the Insurer must acknowledge in the applicable Certification the missed target and indicate that no corrective action plan was necessary. The Insurer will need to continue closely monitoring the network. Managed Care Annual Filing Training Manual 3.2013 Page 97 If the target was missed by more than 5%, the Insurer must describe in the applicable Certification the corrective action taken/planned by it and/or the Intermediary. If no corrective action was taken/planned, an explanation must be provided in the applicable Certification. “ERROR” messages will occur if the network type is not checked, if more than one network type is checked and/or if a provider type cell within an appointment type is left blank. Explanations must be provided in the Comment Box for any “ERROR” message or if “N/A” is entered in a cell. Managed Care Annual Filing Training Manual 3.2013 Page 98 29. D16. PERCENTAGE OF PROVIDERS UNDER EACH COMPENSATION MODEL / D17. RANGE OF WITHHOLDS AND BONUSES, BY COMPENSATION MODEL Plan Data Grid D16: Based on the unique provider totals reported in data grid D7, check the applicable Compensation Model(s) paid directly to providers by the Plan: o “Salary N/A”, “Salary W/O Withhold or Bonus”, “Salary W/Withhold or Bonus” or “Salary W/Both’ o “Fee-for-Service N/A”, “Fee-for-Service W/O Withhold or Bonus”, “Fee-forService W/Withhold or Bonus” or “Fee-for-Service W/Both’ o “Capitation N/A”, “Capitation W/O Withhold or Bonus”, W/Withhold or Bonus” or “Capitation W/Both” “Capitation Enter the percentage of providers paid under each compensation model. Enter the percentage range (i.e. 5% - 10%) of withhold or bonus, if applicable, in data grid D17. Intermediary Data Grid D16: Based on the unique provider totals reported in data grid D7, check the applicable Compensation Model(s) paid directly to providers by the Intermediary: o “Salary N/A”, “Salary W/O Withhold or Bonus”, “Salary W/Withhold or Bonus” or “Salary W/Both’ o “Fee-for-Service N/A”, “Fee-for-Service W/O Withhold or Bonus”, “Fee-forService W/Withhold or Bonus” or “Fee-for-Service W/Both’ o “Capitation N/A”, “Capitation W/O Withhold or Bonus”, “Capitation W/Withhold or Bonus” or “Capitation W/Both” Enter the percentage of providers paid under each compensation model. Enter the percentage range (i.e. 5% - 10%) of withhold or bonus, if applicable, in data grid D17. Managed Care Annual Filing Training Manual 3.2013 Page 99 The data grids will be shaded in certain areas depending on whether the Insurer is an HMO or PPO, and no input will be required. Only licensed HMOs/DMOs/VMOs are authorized to enter into risk-based compensation (capitation and percentage of premium) arrangements with provider networks. PPOs are restricted to fee-for-service arrangements only. “ERROR” messages will occur if the compensation models boxes are left unchecked, if more than one compensation type under one model is checked, and/or if a provider type cell is left blank. Explanations must be provided in the Comment Box for any “ERROR” message or if “N/A” is entered in a cell. Managed Care Annual Filing Training Manual 3.2013 Page 100 30. D18. LIST OF PLAN’S DELEGATED ENTITIES AND NETWORK INTERMEDIARIES List all contracted Delegated Entities and Intermediaries, including Pharmacy Benefit Managers: Enter the name of each Delegated Entity and/or Intermediary. Any affiliated/parent/sister entity that was contracted to perform a delegated activity through a Management/Service Agreement during the specified data year must also be listed. The distinction between a contracted organization (Delegated Entity) and an Intermediary organization lies in the provision of a provider network. Enter the form number of the contract between the Plan and the named Delegated Entity and/or Intermediary. Do NOT provide the approved policy/certificate form number(s) for the contract form number(s). Check the status of the contract: o Active = Contracts approved by the Life & Health Division o Inactive = Contracts that have been terminated with Life & Health Division’s acknowledgment o New = Contracts newly approved by the Life & Health Division, Contracts still under review by the Life & Health Division or Contracts yet to be filed with the Life & Health Division Enter the Delegated Entity and/or Intermediary’s mailing address. Check the applicable activities delegated to perform by each Delegated entity and/or Intermediary. Check to ensure that all fields (column details) are complete. In addition, for each entity make sure that the entity is listed on the C1. Annual Filing Checklist under the corresponding item number (Item numbers: C4, C6 and/or C9), and that the applicable Certification has been completed for the checked delegated activities (i.e. C4: Delegated Grievances, D6: Delegated Utilization Review and/or External Review, C7: Intermediary, and C8/C9 Provider Availability/Accessibility). The data grid D18 is also used to ensure that the Insurer has submitted the applicable Delegated Entity and/or Intermediary data grids. For any Intermediary listed, the contract form number, including any amendments, of the approved Intermediary Agreement must be provided. Every document that comprises the entire agreement must be specifically named. Pursuant to 11 NCAC 20.0205(3), each page of the contract form must show the unique form number in the bottom left corner. Managed Care Annual Filing Training Manual 3.2013 Page 101 For any delegated entity (including affiliated/sister/parent, companies) the Management Service Agreement form identification (i.e. name of document and/or form number) must be provided. Management Contracts are between two corporations (generally between parent corporations or holding corporations and their subsidiaries) for the purpose of providing for the administration of the business of one of the corporation. Pursuant to NCGS 58-67-30, no health maintenance organization shall enter into an exclusive agency, management, or custodial agreement unless the agreement is first filed with the Commissioner (Life & Health Division) and approved. 11 NCAC 20.0601(c) and (d) requires HMOs to file notice of addition or deletion of an intermediary. When applicable, the HMO must provide in the Comment Box the NCDOI/SERFF tracking number for the filing. In accordance with 11 NCAC 20.0201(b) and 11 NCAC 20.0204(a) contracts between the Carrier and Intermediary must be filed with the Life & Health Division prior to use. In accordance with 11 NCAC 20.0203 all material changes as defined in the Administrative Code (and including changing the previously approved form number) made to an approved contract form must be filed with the Life & Health Division for approval before use. (HMOs refer to 11 NCAC 20.0601(e)). The Company must be able to provide copies of approved Management /Service Agreements and/or Intermediary Agreements upon request by the Department or other regulatory action (i.e. market inquiry or market conduct examination). Contract Status: If the contract has been previously approved by the Life & Health Division prior to the specified data year and no material changes were been made to the contract during the specified data year, check the “Active” status. If the contract terminated during the specified data year, check the “Inactive” status and enter the termination date. If the contract was approved by the Life & Health Division during the specified data year, check the “New” status and enter the approval date along with the NCDOI/SERFF tracking number of the approved Life & Health filing. If the contract has been filed with our Life & Health Division but the filing is still pending approval, check the “New” status and enter the current NCDOI/SERFF tracking number. An explanation must be provided in the Comment Box. If the contract has yet to be filed with the Life & Health Division, check the “New” status and provide an explanation, including the projected filing date, in the Comment Box. Managed Care Annual Filing Training Manual 3.2013 Page 102 If the Plan/Intermediary is adding a “New” network option to a previously approved Intermediary Arrangement, the Plan must contact the Life & Health Division for determining if an “Intermediary Network Addition” filing will be required or any other filing instructions. For any “New” Intermediary filing which was approved by the Life & Health Division during the specified data year, the Insurer must be sure to complete the Supplemental Checklist as described in the Instructions. The current year data grid D18 will be compared to last year’s data grid D18, so it is imperative to report/explain any changes in the Comment Box. Failure to note any changes or explain discrepancies accordingly will be questioned by the Department. “ERROR” messages will occur if the contract form number and/or mailing address fields are left blank, if the “Delegated Activities” are unchecked, if the contract status is unchecked or if more than one contract status boxes are checked. Explanations must be provided in the Comment Box for any “ERROR” message or if “N/A” is entered in a cell. Managed Care Annual Filing Training Manual 3.2013 Page 103 31. SUMMARY OF “ERROR” AND “EXPLAIN” MESSAGES A listing of all “ERROR” and “EXPLAIN” messages received while completing the data grids will appear. The Plan must ensure that it and its Delegated Entity(s)/Intermediary(s) have resolved and/or addressed in the applicable Comment Box all of the issues prior to the Plan submitting the data to the Department. Managed Care Annual Filing Training Manual 3.2013 Page 104 32. PLAN/INTERMEDIARY COMMENTS If the Plan and/or Delegated Entity/Intermediary need more space than provided in the Comment Box below the data grid, this page can be used for additional space to continue providing the explanation to any “ERROR” and “EXPLAIN” messages, listing of contracted hospital by county, etc. The Plan and/or Delegated Entity/Intermediary must reference the applicable data grid. . Managed Care Annual Filing Training Manual 3.2013 Page 105