Supplementary Material - Journal of the American College of
advertisement

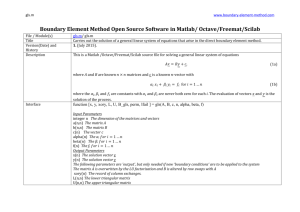
Supplementary Material Table A. Summary of studies that have used advanced myocardial mechanics to illustrate early myocardial injury during cancer chemotherapy (Studies in adult patients are presented first followed by studies in pediatric patients). Study (year) Echo Method Cancer Type N (age, years), % female 78 (52±10), 98.7% Treatment Echo Timing Key Findings Doxorubicin 81% mean (range) cumulative dose 238mg/m2 (140-340), epirubicin 19%, 392mg/m2 (255-572). 68% of HER(-) patients received radiotherapy. All HER2(+) received trastuzumab. Pre- and 1 week postanthracycline (12-18 weeks, preradiotherapy), then at 6 & 12 months (only in HER2-) GLS fell by 9% by end of anthracycline (-18.6±2.4% to 17.0±2.2%) in all 78 patients. Also a 2% relative drop in LVEF was seen. In the HER2(-) patients GLS fell by 7.9% post-anthracycline (-19.0±2.3% to -17.5±2.3%) but normalized in 84% by 12 months. Basal and mid LV segments had significant reduction in GLS but not apex. Early diastolic strain-rate fell by 10% (1.00±0.24% to 0.90±0.22%) postanthracycline. Pre-therapy GLS and LVEF correlated with post-therapy diastolic strain (r=-0.35 and -0.54). GLS data reported in previous study3. Stoodley et al 20131‡ STE GLS (2 and 4 chamber) Breast 28 HER2(+), 50 HER2(-) Stoodley et al 20132‡ STE GLS and diastolic strain rate (2 and 4 chamber) Breast, HER2(+) and (-) 52 (49 ± 9), 100% Doxorubicin in 77%, mean±SD cumulative dose 236±33 mg/m2, epirubicin in 23%, dose 408±110mg/m2, no radiotherapy Pre-and 1 week postanthracycline (12 -18 weeks, preradiotherapy or trastuzumab) Zhang et al 20124 TDI LSR from the basal IVS Breast (no HER2 data) 60 (54±12), 100% Epirubicin maximal cumulative dose 400±40mg/m2 (30 patients randomized to treatment with salidroside and 30 to placebo) Pre, and 7 days post-reaching epirubicin doses of 100,200,300, and 400mg/m2 Motoki et al 20125 STE LV twist and untwist parameters + GLS (3 apical views), NHL, AML, ALL 25 (58±11), 56% female Anthracyclines, equivalent cumulative dose 98±59mg/m2 at 1 month and 170±87mg/m2 Pre, 1 and 3 months after start of anthracycline Fall in LSR seen in both groups by 200mg/m2 - salidroside 15·5% (1.68±0.54 to 1.42±0.49/s) placebo 16.0%(1.69 ± 0.64 to 1.35±0.36/s), LSR returned to normal by 300mg/m2 in the salidroside but not placebo group. At end of therapy LSR in the placebo group was lower than salidroside group (1.40±0.23 vs 1.68±0.29/s). No change in mean LVEF. Reduced peak systolic torsion, twisting rate, untwisting rate by 1 month compared to baseline. GLS reduced by 1 month, no change in Vendor, Reproducibility GE, Inter GLS COV 9.0%, Intra 9.9% GE, inter and intra as mean difference (SD) for early 0.08 (0.12/s) & 0.01(0.05/s) and late diastolic SR 0.06(0.12/s) &0.01 (0.08/s), GLS -1.73 (1.0%) and 0.86(0.59%) Philips, Inter and intra of LSR as percentage of mean of two repeated measures 10 ± 4% and 11± 3%. GE, Inter and intraobserver variability as bias ±1.96SD for LV torsion were - GCS (mid SAX) at 3 months, no radiotherapy Stoodley et al 20113‡ STE GLS (4 chamber), GRS, GCS (mid SAX) and strain-rate Breast, HER2(+) and( -) 52(49±9), 100% Doxorubin and epirubicin (mean cumulative dose 236±33mg/m2 and 408 ±110mg/m2), radiotherapy 0% Pre- and 1 week postanthracycline (12 -18 weeks, preradiotherapy or trastuzumab) Cadeddu et al 20106 TDI LS and LSR (septum) Multiple 49 (56±13), 76% Epirubicin (maximal cumulative dose 400±20mg//m2) but 25 received telmisartan and 24 placebo, radiotherapy 0% Pre- and 7 days post-epirubicin dose of 100, 200, 300, and 400 mg/m2 Wildiers et al 20087† TDI RS and RSR (SAX mid inferior lateral wall) Breast, HER2(+) and (-) TDI LS and LSR (septum) Multiple Liposomal doxorubicin (cumulative dose 180mg/m2), radiotherapy 0% Epirubicin cumulative dose 400mg/m2 (58%) and 300mg/m2 (42%) Pre, before 4th cycle, after 6th cycle Mantovani et al 20088* 16 (median 69, range 65-74), 100% 31 (59±14), 74% Jurcut et al, 20089† TDI LS and LSR (3 apical views, 18 segments), RS and RSR ( SAX mid inferior lateral wall) Breast, HER2(+) and (-) 16 (69.8±3.1), 100% Liposomal doxorubicin (cumulative dose 180mg/m2), radiotherapy 0% Pre- and within 7-14 days after 3rd and 6th cycles Pre, 7 days post100, 200, 300, 400mg/m2, and 3, 6, 12 &18 months post-last dose GCS. All parameters correlated with anthracycline dose. (No absolute values). Patients with lower torsion at baseline had more significant drop in torsion at 3 months. Reduced GLS by 8% (-17.8±2.1%to 16.3±2.0%) and GRS by 15% (40.5±11.4% to 34.3±11.4%), no change in GCS. LVEF from 58·6 ±2.6% to 56.0 ± 2.8%. None had LVEF drop ≥10%, however those with an LVEF ≤55% post-therapy had lower GLS than those with LVEF >55%. No change in any of the strainrate parameters. Significant reduction in septal LSR by 200 mg/m2 vs baseline by 20% (1.78±0.24 to 1.41±0.31/s) in placebo and 13% in telmisartan (1.83±0.24 to 1.59±0.36/s). LSR recovered in telmisartan group but not placebo. No change in strain or LVEF in either group. RS and RSR reduced by 34% (50±12% to 33±8%) and 28% (4.6±1.2 to 3.3±1.0/s) after 6th cycle. No significant change in LVEF Reduced septal LSR after 200 mg/m2 of epirubicin by 19% compared to baseline (1.79±0·06 to 1.45±0·15/s) and remained reduced for 18 mos. No change in LS or drop in LVEF. No data on LS or LSR predicting changes in LVEF. Compared to baseline, RS fell 25% (50.1±11.6 to 37.7±10.2%) and RSR 20% (4.57±1.18 to 3.64 ±1.52/s) after 3 cycles and GLS 17% (-22.7±2.8 to 18.8±2.8%) and LSR 12% (-1.54±0.19 to -1.36±0.23/s ) after 6 cycles. No 0.26º (1.59) and 0.21º (1.39). GE, mean (SD) inter and intra for GLS 1.73(1.0%) & 0.86(0.59%). GRS 5.0 (7.8%) & 3.4 (12.4%). GCS 1.48 (1.24%) & 1.62 (1.10%) Toshiba, no data GE, no data Toshiba, No data. GE, mean relative intraobserver variability was 8.3% of strain and 9.1% for strain rate change in LVEF. Mercuro et al 2007 10* TDI – LS and LSR (septum) Multiple 16 (56±3), 81% Epirubicin cumulative dose of upto 400mg/m2 Pre-therapy and after 200, 300, and 400 mg/m2 Poterucha et al 201211 STE GLS (3 apical views) Various pediatric 19 (15·3±3), 37%. 19 controls Mean cumulative anthracycline dose 296 ±103mg/m2, doxorubicin (89%), idarubicin (32%), danorubicin (5%), radiotherapy 0% Before, 4, and 8 months after starting anthracycline Al-Biltagi et al 201212 STE GLS (3 apical views) ALL 25 (9±2.6), 48%, 30 controls Doxorubicin 30mg/m2 (as part of induction therapy). No radiotherapy. Pre- and within 1 week of starting doxorubicin Ganame et al 200713 TDI – LS and LSR (entire septum) and RS and RSR (SAX mid inferior lateral wall) Multiple 13 (10.7±3.8), 23% Danorubicin (30 or 40mg/m2), doxorubicin (60-75mg/m2), or Idarubicin 10mg/m2 Before first dose, then post-1, 2, and 3rd doses Reduced septal LSR after 200 mg/m2 of epirubicin by 20% versus baseline (1.82±0.57 to 1.45±0.44/s). No change in LS, LVEF. GLS fell by 9% by 4 months vs pretherapy (-19.9 ±2.1% to -18.1±2.5 %), remained reduced at 8 months (18.1±2.8%). Also GLS fell compared with controls (-20.5±1.5%) at both time points. LVEF did not change until 8 months (62±3% to 59±3%). Correlation between fall in LVEF between pre-therapy and 8 months and the fall in average mid (r=-0.49) and apical (r=-0.48) segmental LS was reported but no data on early change in strain predicting LVEF drop. Pre-therapy, patients had lower GLS (18.7±4.5% vs -21.5± 2.2%) than controls. Post-treatment the GLS fell further by 19% to -15.1 ± 2.5%. Fractional shortening also fell (40±4.9% to 33.5± 6.6%). RS and RSR fell by 24% (74±14% to 56±11%) and 15% (5.4±0.9 to 4.6±0.8/s) and LS and LSR fell by 15% (-27±5% to -23±7%) and 9% (2.2±0.4% to -2.0±0.4%) after first dose and remained reduced. LVEF change significant by second dose (71±4% to 66±4%) Toshiba, no data GE, GLS COV Inter 7.2%, Intra 10%. GE, no data GE, mean difference (95% CI): intra / inter LS 2.67(3.69%) / 5.14 (3.73%), LSR 0.13(0.13/s) / 0.44 (0.41/s), RS 2.03(2.81%) /6.44(8.98)%, RSR 0.44 (0.36/s) / 0.50 (0.33/s) STE, speckle-tracking echocardiography; TDI, tissue-doppler imaging, GCS, global circumferential strain; GCSR, global circumferential strain-rate; GLS, global longitudinal strain; GLSR, global longitudinal strain-rate; GRS, global radial strain; GRSR, global radial strain-rate – the word global was used for all STE-based strain as multiple segments were used; for TDI strain, unless multiple segments were used, the character G is removed to illustrate that this is not “global” strain; GE, General electric; IVS, interventricular septum; SAX, short axis; NHL, Non-Hodgkin’s Lymphoma; ALL, Acute Lymphoblastic Leukemia, AML; Acute Myelogenous Leukemia; COV, coefficient of variance. *‡study from same group with likely overlap in the patients; †study of the same patients. Table B. Summary of studies that have used early changes in advanced myocardial mechanics to predict subsequent cardiotoxicity (Studies in adult patients are presented first followed by studies in pediatric patients). Study (year) Echo Method Cancer Type N (age, years), % female 74 (51±11), 58%, 37 controls Treatment Echo Timing Key Findings Prognosis Anthracycline equivalent cumulative dose 118±43mg/m2 at 6 weeks and 178±58mg/m2 at 12 weeks. Total cumulative dose 259±52mg/m2, no data on radiotherapy Preanthracycline, immediately post, 6, 12, 24, and 52 weeks later By 6 weeks GLS fell 10.4% (-21.2±2·5 to 19.0±2·4), GRS 14.0% (47.8±5.3% to 41.1±5.4%), apical rotation 16% (8.1±1.4% to 6.8±1.3%), twist 10.8% (13.8±1.7% to 12.3±1.7%), and GLS x twist by 19.9% (-297±68 to -238±57). No separate data for cardiotoxicity group. Significant GLS fall of 11.4% (-20.7±2.6% to 18.3±2.1%), GLSR 12.8% (-1.17±0.24 to 1.00±0.15/s) and GLSRE-E 11.9% (1.36±0.28 to 1.20±0.28/s) at 6 months in patients with cardiotoxicity at 12 months. GCS and GRS changes not significant. No data for whole group For the whole group GLS fell 6.9% (-20.3±2.7% to 18.9±2.5%) at 3 months, and GRS 5.6% (53.1±4% to 50±3.9) at 4 months . In patients with cardiotoxicity fall in GLS and GRS at 3 months by 20.1% (20.4±3·0% to 16.3±2·4%) and 5.5% (54±2% to 51±4%) and at 4 months by 22.0%(to -15.9±1·7%) 13% cardiotoxicity (CREC criteria). Best predictors of cardiotoxicity between 24 and 52 weeks were change between pre-therapy and 6 weeks in GLS x twist – cut-off of 71% x o had sensitivity 90%, specificity 82% and GLS – cut-off of 2.77% (13·1% relative) had sensitivity 79% and specificity 73%. 30% cardiotoxicity (EF fall ≥ 10%). Relative GLS change ≥11% between preand 6 months had sensitivity 65% and specificity 95% to predict cardiotoxicity at 12 months. Absolute GLS >20·5 at 6 months also predictive (sensitivity 96%, specificity 66%) 19.4% cardiotoxicity (CREC criteria) by 6 months. Relative GLS fall ≥15% at 3 months had sensitivity 86% and specificity 86% and GRS ≥10% at 4 months had sensitivity 86% and specificity 69% for cardiotoxicity. Combination of both sensitivity 71%, specificity Mornos et al, 201314 STE GLS (3 apical views), twist (basal and apical slices), and GRS (mid SAX) Breast (HER2-), lymphoma, ALL, AML, osteosarcoma Negishi et al 201315 STE GLS, GLSR, early diastolic GLSR (GLSR-E) - 3 apical views, GCS, GRS (mid SAX) Breast HER2(+) 81 (50 ± 11), 100% 100% trastuzumab, 46% doxorubicin <240mg/m2 or epirubicin <600mg/m2, radiotherapy 62%. Pretrastuzumab, 6, and 12 months later Baratta et al 201316 STE – GLS (2 and 4 chamber basal and mid segments), GRS (mid SAX) Breast (HER2+ and -) (n=16), lymphoma/ leukemia (n=11), other (n=9), 36 (47 ± 16), 58% Doxorubicin in 58% (mean 294±122mg/m2 in those with cardiotoxicity and 102±124mg/m2 in those without), trastuzumab in 22%. No data on radiotherapy Pre, 2,3,4, and 6 months after start of therapy Vendor, Reproducibility GE, Intra ICC (COV) for GLS x twist 0.94(2.9%), GLS 0.95 (2.6%), LV twist 0.93 (3.1%), GRS 0.91 (2.9%). Inter 0.90 (4.3%), 0.91 (3.9%), 0.89 (4.8%), 0.84 (5.1%) GE, Intra ICC (95% CI) for GLS 0.85 (0.54-0.96%), GLSR 0.91 (0.700.98/s), GLSR-E 0.90 (0.66-0.97/s). Inter 0.71 (0.230.92%), 0.85 (0.280.97/s), 0.87 (0.560.97/s). GE, mean (SD) absolute difference inter / intra GLS 0.6 (1.4%) / 0.2 (1.1%), GRS 3.4 (7.1%) / 3.2 (6.6%) Sawaya et al, 201217 STE GLS (basal and mid segments of 4CH and 2CH views), GCS, GRS (mid SAX) Breast HER2(+) 81 (50±10), 100% Cumulative doxorubicin 240mg/m2 or epirubin 300mg/m2, then paclitaxel and trastuzumab, radiotherapy 60%. Preanthracycline, 3 months (pretrastuzumab), then at, 6, 9, 12, 15 months Sawaya et a,.201118 STE GLS (basal and mid segments of 4CH and 2CH views), GCS, and GRS (mid SAX) Breast HER2(+) 43 (49 ± 10), 100% Doxorubicin 240mg/m2 or epirubicin 300mg/m2, taxanes and trastuzumab, radiotherapy 11.6% Preanthracycline, 3, 6 months Fallah-Rad et al 201119 STE GLS (3 apical views), GRS (mid SAX) Breast, HER2(+) 42 (47 ± 9), 100% FEC 6 cycles in 88% (max epirubicin 600mg/m2), AC 4 cycles in 12% (max doxorubicin 240mg/m2) then trastuzumab (no taxanes), radiotherapy 98%. Preanthracycline, Pretrastuzumab, 3, 6, 9, 12 months thereafter Hare et al, 200920 TDI LS and LSR (6 basal segments) STE GLS, Breast HER 2(+) 35 (51±8), 100% Doxorubicin or epirubicin use in 91%, taxane 89%, and trastuzumab Baseline (preand/or postanthracycline ) and at 3 and 14.8% (to 46±2%). Significant fall in GLS of 10% (-21±2% to -19±2%), GRS 6% (53±15% to 50±17%), GCS 11% (18±4% to -16±4%) for the whole group by 3 months compared to baseline. GLS fell by a maximum of 15±3% for the group with cardiotoxicity Significant fall in GLS by 5·8% (-20.5±2.2% to 19.3±2.4%), GCS by 16.7% (18±4% to 15±4%) for whole group by 3 months compared to baseline. GRS fall not significant by 3 months. GLS fell by 15±8% and GRS 22±22% in group with cardiotoxicity. GLS fell by 18% (19.8±1.8% to -16.4±1.1%) and GRS by 19% (41.4±15.2% to 34.5±15.2%) at 3 months into trastuzumab (versus pre-trastuzumab) in patients with cardiotoxicity. No data for group as whole. TDI LS – no change, LSR 13% fall (-1.32±0.28 to 1.15±0.27/s) by 3-6 months. STE GLSR fell by 97%. 32% cardiotoxicity (CREC criteria). Fall in absolute GLS at 3 months to < -19% predicted subsequent cardiotoxicity sensitivity 74%, specificity 73%, PPV 53%, NPV 87%. Relative fall in GLS of 10% also predictive. GE, same variability as in previous study18. 21% cardiotoxicity (CREC criteria). A 10% relative fall of GLS by 3 months had sensitivity 78%, specificity 79%, PPV 50%, and NPV 93% to predict cardiotoxicity at 6 months. GE, intra as absolute mean error (SD) GLS 0.14(1.1%), inter 0.5 (1.5%). GRS 2 (5%), 2.2 (7.5%).GCS 0.53 (2.82%), 3.3 (3.5%). 24% cardiotoxicity (Fall in LVEF ≥10% to <55%, signs or symptoms of CHF, discontinuation of drug). Absolute GLS fall of 2·0% (~10.1% relative) had sensitivity 79%, specificity 82%, PPV 60%, and NPV 92% and absolute GRS fall of 0.8% (~1.9% relative) sensitivity 86%, specificity 81%, PPV 60%, and NPV 95% to predict cardiotoxicity. Amongst 14 patients who had a drop in 2D GLSR >1SD during therapy 2 (14%) and had follow-up, a GE, Intra as ICC (COV) GLS 0.94 (3.5%), GRS 0.91 (3.2%). Inter 0.90 (5.2%), 0.82(5.4%) GE, Intra / Inter as ICC for 2D GLS 0.94 / 0.91, GLSR 0.94 / 0.91, GRS GLSR (3 apical views) GRS and GRSR (mid SAX) Mavinkurve -Groothuis et al, 201321 STE, GLS (4CH), for GRS and GCS (mid SAX) and strain-rate for all ALL 60 (49 with complete f/u), age 6 (2.2-15.4), 38%. 60 controls. 100%, radiotherapy 77% month intervals after start of trastuzumab Anthracycline equivalent cumulative dose – 120mg/m2 to 300mg/m2, radiotherapy 100% Preanthracycline, 10 weeks and 12 months later 5% by 3 months (1.30±0.21 to -1.24±0.18/s) and RSR by 13% by 6-9 months (2.02±0.61 to 1.75±0.41/s). A fall ≥1SD in LSR and RSR seen in 51% and 37% of patients. No fall in GLS or GRS. No separate data on cardiotoxicity group By 12 months significant fall in GLS by 8·2% (18.2±3.1% to -16.7±5·2%), GLSR 16.7% (-1.44±0·3 to -1.20±0.4/s), GRS 17.3% (66.8±1% to 55.2±16%), GCS 12.9% (-19.4±4.3% to -16.9±3.1%). At 12 months compared to controls, all strain and strain-rate except GRS were lower by 7.7 to 32.4%. drop in LVEF >10% (cardiotoxicity) from baseline as seen at a mean follow-up of 22± 6 months. 0.86 / 0.50, GRSR 0.83/0.65. TDI LS 0.99/0.64, LSR 0.96/0.77 0% cardiotoxicity (Fall in FS > 10%). Early strain values were not predictive of decrease in LV fractional shortening by 12 months. But a decrease in FS >10% was seen in 23% although not into abnormal range. GE, no data. Please see abbreviations from Table A. FS, fractional shortening; FEC, 5-fluorouracil, epirubicin, cyclophosphamide; AC, Adriamycin, cyclophosphamide. 4CH, 4 chamber APPENDIX TABLE C: Guidelines and Position Statements on Monitoring of Chemotherapy-induced Cardiotoxicity ESC Heart Failure Guidelines (2012)22 Pre- and post-evaluation of EF in patients receiving cardiotoxic chemotherapy Heart Failure Association of the ESC (2011)23 Regular cardiovascular evaluation in patients receiving treatment known to be associated with cardiotoxicity Follow-up beyond the completion of chemotherapy should be considered in those receiving high doses of anthracyclines ESMO Clinical Practice Guidelines (2010)24 Baseline assessment with echocardiography in patients undergoing treatment with anthracyclines or monoclonal antibodies if: a) >60 years old b) Cardiovascular risk factors c) Documented cardiomyopathy or previous thoracic radiotherapy Further evaluations of LVEF are recommended according to the following schedule: a) After administration of half the planned dose of anthracycline b) After administration of a cumulative dose of doxorubicin 300 mg/m2, epirubicin 450 mg/m2 or mitoxantrone 60 mg/m2 c) After administration of a cumulative dose of doxorubicin of 240 mg/m 2 or epirubicin 360 mg/m2 in patients <15 years or >60 years d) Before every next administration of anthracycline e) After 3, 6, and 12 months from the end of therapy with anthracycline Assess LV diastolic function for early signs of LV dysfunction before the onset of reduction in LVEF Periodic monitoring every 12 weeks for those receiving monoclonal antibodies Assessment of cardiac function is recommended 4 and 10 years after anthracycline in patients who were treated at <15 years, or even at age >15 years but with cumulative dose of doxorubicin >240 mg/m 2 or epirubicin >360 mg/m2 LVEF reduction of ≥20% from baseline despite normal function or LVEF decline to <50% necessitate reassessment or discontinuation of therapy Children’s Oncology Group Long-Term Follow-up Guidelines from Children’s Oncology Group Late Effects Committee and Nursing Discipline (Version 3.0 – 10/08)25 Age at treatment < 1 year With chest radiation, any anthracycline dose, LVEF every year No chest radiation, total anthracycline dose <200mg/m2, LVEF every 2 years No chest radiation, total anthracycline dose≥200 mg/m2, LVEF every year Age at treatment 1-4 years Chest radiation, any anthracycline dose, LVEF every year No chest radiation, total anthracycline dose <100 mg/m2, LVEF every 5 years No chest radiation, total anthracycline dose ≥100 mg/m2 to <300mg/ m2 LVEF every 2 years No chest radiation, total anthracycline dose ≥300mg/ m2 LVEF every year Age at treatment ≥5 years Chest radiation, total anthracycline dose <300mg/ m2, LVEF every 2 years Chest radiation, total anthracycline dose ≥300 mg/m2, LVEF every year No chest radiation, total anthracycline dose <200 mg/m2, LVEF every 5 years No chest radiation, total anthracycline dose ≥200 mg/m2 to <300mg/ m2 LVEF every 2 years No chest radiation, total anthracycline dose ≥300mg/ m2 LVEF every year ASCO Clinical Evidence Review on the Ongoing Care of Adult Cancer Survivors (2007) 26 No approved surveillance recommendation for long-term cardiotoxicity in asymptomatic cancer survivors due to the lack of high quality evidence ACC/AHA Heart Failure Guidelines (2005)27 Monitor closely for the development of cardiac dysfunction ACC/AHA/ASE Clinical application of echocardiography guidelines (2003) 28 Class I indication to use echocardiography for baseline and re-evaluation examinations of patients receiving cardiotoxic chemotherapeutic agents. TABLE D: Summary of studies that have used advanced myocardial mechanics parameters to demonstrate subclinical myocardial injury in patients who previously received cancer chemotherapy (Studies in adult patients are presented first followed by studies in pediatric patients). Study (year) Echo Method Cancer Type N (age, years), % female 70 (54±8), 100%, 50 controls Echo Timing Key Findings Anthracycline (mean range 402[312-580mg/m2) with (n=19) and without (n=51) trastuzumab, radiotherapy (55±9 Gy) 80% Anthracyclines, mean cumulative dose of 229mg/m2 (range 40–644 mg/m2) Mean of 4.2±1.8 years postanthracycline or 3.1± 1.9 years posttrastuzumab for breast cancer Median of 7·2 years (2.4-16.4 years) after completion of anthracycline Reduced global LS compared to control by 7.7% (-18.1±2·2% versus 19·6±1·8%). 26% had GLS below lower limit of values for control group. No differences in radial strain or LVEF. Number of patients with LV dysfunction not provided. GE, Intra / Inter as ICC (COV) GLS 0.97(3.1%) / 0.95 (4.8%), GRS 0.97 (2.9%) / 0.97 (5.0%) Compared to control, LVEF reduced by 7·5%(60.1±4.2 vs 55.6±4.2), 3D global by 21% (44.7±7.8 vs 35.4±7.5), twist by 33% (9.9±3.2 vs 6.6±2.5), torsion 32%(1.9±0.7 vs 1.3±0.5), GPI by 67%(20.2±10·6 vs 6.7±3.9). Cumulative anthracycline dose correlated with 3D LV global strain (r=-0.32), GPI (r=-0.32) Compared with control: Reduced GRS of the mid-papillary level inner and outer layers, and the apical inner layers (11.6-20.6%). Lower transmural GCS gradients at all 3 LV levels (9.919.2%). Reduced rotation, PSTV and PDUV of both subendocardial and supepicardial layers of the base and subendocardial layer only of the apex (exact values not provided). Reduction in the apical transmural rotation gradient by 41.3% (2.7 ± 1.7 vs 4.6 ± 2.4º). No reduction in GLS. Number of patients with LV dysfunction not provided. LS and LSR were significantly lower in the basal RV, LV septal, lateral, and inferior walls. No values provided. Toshiba, Intra / Inter as COV 3D strain 7.3% / 8.2%, twist 7.5% / 10.3%, torsion 7.7% / 10.7% Ho et al 2010 29 STE – GLS (3 apical views) and GRS (mid SAX) Breast Yu et al 201330* 3D STE global systolic strain, LV twist, torsion, global performance index (GPI) = global 3D strain x torsion/systolic dyssynchrony index) STE - GLS (4 CH), GRS GCS and rotation parameters (basal, mid, and apical SAX). Layer specific strain analysis Multiple pediatric 53 (18.6±5.1), 30%, 38 controls Multiple pediatric 32 (19.3±5.4), 34%, 28 controls Anthracyclines, mean cumulative dose of 220mg/m2 (range 120–470 mg/m2) Median of 6.9 years (2.2-14.4 years) after completion of anthracycline TDI – LS and LSR from 4 basal LV segments (4 and 2 Multiple pediatric 19, (median age 14), 32%. 17 controls Doxorubicin, daunorubicin, or epirubicin dose ≥ Median of 67 months (range 8-142 Yu et al 201331* YagciKupeli et al 201232 Vendor, Reproducibility Treatment Toshiba, Inter and intra reported as COV for all parameters. Intra ranged from 2.49% to 6.29%, and inter from 2.86% to 13.35% GE, no data. Cheung et al 201133 chamber views) and one RV lateral wall segment STE - LV torsion parameters (basal and mid SAX) ALL (childhood survivors) 36 (15.6 ± 5.5), 47%, 20 controls 350mg/m2 (range 350-480 mg/m2), radiotherapy 10·5% Doxorubicin or daunorubicin, mean (range) cumulative dose 240mg/m2 (120-470 mg/m2) months)postanthracyclines Three patients had LV dysfunction Median of 7 years (3.1-24.3 years) after last anthracycline dose Reduced peak LV systolic torsion by 32% (8.0±4.1degrees vs 11.8 ± 4.5degrees), systolic twisting velocity by 25% (68.1 ± 20.3(degree/sec vs 91·0 ± 22·3 (degree/sec), and diastolic untwisting velocity by 18% (-90.1 ± 34.3(degree/sec vs -109.6 ± 33.4(degree/sec ) compared to control. This was a reflection of reduction in apical rotational parameters. Patients had lower LVEF than controls but 78% had LVEF ≥ 50%. Reduced global LS, CS, RS, and CSR compared to controls reductions of 7% (-17.6 ± 3.0% vs -19.0± 2.2%) , 17% (14.5 ±2.9% vs -17.4 ± 4.3%), 20% (40.1 ± 15.6% vs 50.0 ± 16.4%), and 15% (0.90 ± 0.21/s vs 1.06 ± 0.28/s) respectively. No reductions in GLSR. Cumulative anthracyline dose correlated with LSR (r=-0.33) and CSR (-0.32). None with LV dysfunction. Compared to controls all strain and strain-rate values were significantly reduced. GLS 6.6% (-19.8±2.6% vs 21.2±1.6%), GLSR 12.9% (-1.22 ±0.19/s vs -1.40 ± 0.08/s), GRS 14.0% (49±12% vs 57±5%), GRSR 48·9%(1.75±0.35/s vs 3.43±0.36/s), GCS 29.6% (-15.9±6.7% vs 22.6±2.1%), GCSR 19.1%(1.48±0.42/s vs -1.83±0.17/s). Number of patients with LV dysfunction not provided. Cheung et al 201034 STE - LV GLS, GLSR (4CH), GCS, GCSR, GRS (mid SAX) ALL 45 (15.3±5.8), 38%, 44 controls Doxorubicin or daunorubicin median (range) cumulative dose 240mg/m2 (120470mg/m2), radiotherapy 0% Median 6.3 years (2.7-19.8 years) postanthracycline Mavinkurve -Groothuis et al 201035 STE- GLS, GLSR (4CH), GCS, GCSR, GRS, GRSR (mid SAX) Multiple pediatric 111(20[5.637.4], 49%, 107 controls Doxorubicin or daunorubicin, cumulative dose median (range) 180mg/m2(50-600), radiotherapy 6.3% Median of 13.2 years (5.0-29.2 years posttherapy GE, intra / inter as mean (SD) difference for LV torsion 0.9º (5.0) / 4.0 º (7.1), peak systolic twisting velocity 0.0 º/sec (9.5) / -2.1 º/sec (10.8), peak diastolic untwisting velocity 1.7 º/sec (11.2) / -2.0 º/sec (14.4) GE, no data. GE, no data. Park et al 200936 STE – GLS and GLSR using VVI (4CH) Multiple pediatric 14 (age 6 to 17), 50%, 14 controls Anthracyclines cumulative dose between 90342mg/m2 > 3 years posttherapy Ganame et al 200737 TDI – LS and LSR (basal, mid, and apical septum, lateral wall, RV free wall) and RS and RSR (inferior lateral wall). Pediatric, ALL, lymphoma, solid tumour, or AML 56 (median 12.7 [4-28]), 61%, 32 controls Doxorubicin, daunorubicin, or idarubicin. Median cumulative dose 240mg/m2, range (90-300mg/m2) Median 5.2 years (2.0-15.2 years) after last dose of anthracycline. Although systolic strain, strain-rate, and diastolic strain-rate were lower in patients, it was not statistically significant. However compared to controls longitudinal peak systolic strain-rate fell by 12.2%(-1.89 ± 0.63/s vs -1.66 ± 0.27/s) and diastolic strain by 19.6% (2.38 ± 0.77% vs 2.96 ± 1.26%) in the septum. None had LV dysfunction. Reduced RS and RSR by 15-20%. Reduction in LS and LSR in each of the 6 LV segments (numbers not provided). Significant drop in LSR in the basal RV segment only by 17.5% (-33 ± 13% vs -40 ± 16%). Mean LVEF normal but 3 patients had abnormal fractional shortening. *study from same group with likely overlap in the patients, Please see Tables A and B for abbreviations. Siemens, intra as mean absolute difference (95% CI) GLS 0.99 (4.08%), GLSR 0.13 (0.53/s), diastolic strain rate 0.18 (0.72/s) GE, intra / inter as absolute mean difference (95% CI) LS 2.56 (3.72%) / 3.48%(3.89%), LSR 0.11(0.12/s) / 0.41(0.42/s), RS 2.79 (2.91%) / 6.03(8.57%), RSR 0.52 (0.47/s), 0.53 (0.59/s) TABLE E: Summary or studies used advanced myocardial mechanics to detect early myocardial injury from radiation therapy Study (year) Erven et al, 201338 Echo Method TDI – GLS ( 3 apical views) Cancer Type Breast HER2(+) and (-) N (age, years), % female 75 (no age), 100%. 51 left sided and 24 right sided caner. Total strain follow-up in 63 patients Treatment Echo Timing Key Findings Doxorubicin or epirubicin (in 100%), RT (50Gy) mean heart and LV doses were 9±4Gy for L sided breast cancer and 4±4 and 1±0.4Gy for R sided. 20% received trastuzumab Before RT, immediately after 50Gy, 8 months, 14 months Erven et al, 201139 TDI – GLS and GLSR (3 apical views) Breast HER2(+) and (-) 30 (no age), 100%. 20 left sided and 10 right sided cancer. Complete follow-up in 20 Epirubicin (100mg/m2, in 53%), RT (50Gy) mean LV dose was 6.7±6Gy for L sided RT and 0.6±0.1Gy for R sided RT. 16.7% received trastuzumab. Before RT, immediately after 50Gy, 2 months Tsai et al, 201140 STE – GLS (3 apical views) and GCS (mid SAX) Hodgkin’s Lymphom a 47 (51±9), 66% RT (mean 41Gy) with (n=27) and without doxorubicin (n=20)(309 ±92mg). Controls (N=20) 22±2 years after therapy Chang et TDI – Lung 40 (48·7 ± 3·2), RT only. Dose 1-2 days pre-RT, GLS fell immediately after RT by 9.8% (-19.4±2.4% to -17.5±1.9%), lowest strain at 8 months with 14.4% reduction (-16.6±1.4%). Strain-rate fell by 12.8% (-1.4±0.26/s to 1.22±0.15/s immediately postRT).Strain and strain-rate remained reduced to 14 months. Changes were only seen in women with L sided RT and involved the anterior wall and not the inferior wall. No change in LVEF. GLS fell in patients with left sided RT by 10.2% (from -19.5±2.1% to 17.6±1.5%) immediately post-RT, and remained reduced at 2 months. No change in overall GLSR. Strain drop was significant in the apical LV segments only, there was a reduction in GLSR in the apical segments only. The strain drop was limited to myocardial segments receiving >3Gy. No change in right sided radiation patients. LVEF reduction immediately post-rad in left sided breast cancer patients by 4·6% (absolute). GLS reduced by 8% in radiotherapy with anthracyclines versus no anthracyclines (-16.1±1.9% vs 17.5±1.7%). No difference in GCS or LVEF. In radiotherapy with and without anthracyclines reduced GLS (21% and 14% respectively) and GCS (19% and 21% respectively) compared to control (-20.4±1.7% and -22.5±2.2%). Patients had lower LVEF than controls. Compared to those imaged pre- Vendor, Reproducibility GE, no data. GE, no data. GE, Intra and inter Cronbach α were 0.98 and 0.97 Philips, no data al, 200941 systolic and early and late diastolic strain-rate (n=27), breast (n=13) 40% between 30-60Gy after week 3 (30Gy), 4 (40Gy), 5 (50Gy), or 6 (60Gy) Wang et al, 200642 TDI – systolic and early and late diastolic strain-rate Lung (19), esophagea l (12), thymic (5), lymphoma (4) 40 (48±3·2), 55% female RT only. Doses between 26-60Gy. 1-3 days before RT, after 2·5-3 weeks (26-30Gy), or 5-6 weeks (5060Gy) Please see Tables A and B for abbreviations. therapy the systolic and early diastolic strain-rate were lower in the anterior septum, and anterior and posterior wall in patients who received 50 and 60Gy of radiation but not with lower doses. Reduction was higher at 60Gy than 50Gy. At 60Gy reduction in systolic strain ranged from 27.4% to 39.5%, and diastolic strain from 31.8% to 37.9%. Compared to those pre-therapy systolic strain-rate and early diastolic strain-rate significantly reduced in the 5-6 weeks group in the basal and mid anterior wall, anterior septum, and posterior wall. Systolic strain-rate reduction ranged from 30·3% to 42·5% and diastolic strain-rate between 32·9%-44·0%. Philips, no data References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. Stoodley PW, Richards DA, Boyd A, et al. Left ventricular systolic function in HER2/neu negative breast cancer patients treated with anthracycline chemotherapy: A comparative analysis of left ventricular ejection fraction and myocardial strain imaging over 12 months. Eur J Cancer 2013; 49(16): 3396-403. Stoodley PW, Richards DA, Boyd A, et al. Altered left ventricular longitudinal diastolic function correlates with reduced systolic function immediately after anthracycline chemotherapy. European heart journal cardiovascular Imaging 2013; 14(3): 228-34. Stoodley PW, Richards DA, Hui R, et al. Two-dimensional myocardial strain imaging detects changes in left ventricular systolic function immediately after anthracycline chemotherapy. European Journal of Echocardiography 2011; 12(12): 945-52. Zhang H, Shen WS, Gao CH, Deng LC, Shen D. Protective effects of salidroside on epirubicin-induced early left ventricular regional systolic dysfunction in patients with breast cancer. Drugs in R&D 2012; 12(2): 101-6. Motoki H, Koyama J, Nakazawa H, et al. Torsion analysis in the early detection of anthracycline-mediated cardiomyopathy. European heart journal cardiovascular Imaging 2012; 13(1): 95-103. Cadeddu C, Piras A, Mantovani G, et al. Protective effects of the angiotensin II receptor blocker telmisartan on epirubicin-induced inflammation, oxidative stress, and early ventricular impairment. Am Heart J 2010; 160(3): 487 e1-7. Wildiers H, Jurcut R, Ganame J, et al. A pilot study to investigate the feasibility and cardiac effects of pegylated liposomal doxorubicin (PL-DOX) as adjuvant therapy in medically fit elderly breast cancer patients. Critical reviews in oncology/hematology 2008; 67(2): 133-8. Mantovani G, Madeddu C, Cadeddu C, et al. Persistence, up to 18 months of follow-up, of epirubicin-induced myocardial dysfunction detected early by serial tissue Doppler echocardiography: correlation with inflammatory and oxidative stress markers. Oncologist 2008; 13(12): 1296-305. Jurcut R, Wildiers H, Ganame J, et al. Strain Rate Imaging Detects Early Cardiac Effects of Pegylated Liposomal Doxorubicin as Adjuvant Therapy in Elderly Patients with Breast Cancer. Journal of the American Society of Echocardiography 2008; 21(12): 1283-9. Mercuro G, Cadeddu C, Piras A, et al. Early epirubicin-induced myocardial dysfunction revealed by serial tissue Doppler echocardiography: correlation with inflammatory and oxidative stress markers. Oncologist 2007; 12(9): 1124-33. Poterucha JT, Kutty S, Lindquist RK, Li L, Eidem BW. Changes in left ventricular longitudinal strain with anthracycline chemotherapy in adolescents precede subsequent decreased left ventricular ejection fraction. Journal of the American Society of Echocardiography 2012; 25(7): 733-40. Al-Biltagi M, Abd Rab Elrasoul Tolba O, El-Shanshory MR, Abd El-Aziz El-Shitany N, El-Sayed El-Hawary E. Strain echocardiography in early detection of Doxorubicininduced left ventricular dysfunction in children with acute lymphoblastic leukemia. ISRN pediatrics 2012; 2012: 870549. Ganame J, Claus P, Eyskens B, et al. Acute cardiac functional and morphological changes after Anthracycline infusions in children. Am J Cardiol 2007; 99(7): 974-7. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. Mornos C, Petrescu L. Early detection of anthracycline-mediated cardiotoxicity: The value of considering both global longitudinal left ventricular strain and twist. Can J Physiol Pharmacol 2013; 91(8): 601-7. Negishi K, Negishi T, Hare JL, Haluska BA, Plana JC, Marwick TH. Independent and incremental value of deformation indices for prediction of trastuzumab-induced cardiotoxicity. J Am Soc Echocardiogr 2013; 26(5): 493-8. Baratta S, Damiano M, Marchese M, et al. Serum markers, conventional Doppler echocardiography and two-dimensional systolic strain in the diagnosis of chemotherapyinduced myocardial toxicity. Rev Argent Cardiol 2013; 81(2): 151-8. Sawaya H, Sebag IA, Plana JC, et al. Assessment of echocardiography and biomarkers for the extended prediction of cardiotoxicity in patients treated with anthracyclines, taxanes, and trastuzumab. Circ Cardiovasc Imaging 2012; 5(5): 596-603. Sawaya H, Sebag IA, Plana JC, et al. Early detection and prediction of cardiotoxicity in chemotherapy-treated patients. Am J Cardiol 2011; 107(9): 1375-80. Fallah-Rad N, Walker JR, Wassef A, et al. The utility of cardiac biomarkers, tissue velocity and strain imaging, and cardiac magnetic resonance imaging in predicting early left ventricular dysfunction in patients with human epidermal growth factor receptor IIpositive breast cancer treated with adjuvant trastuzumab therapy. J Am Coll Cardiol 2011; 57(22): 2263-70. Hare JL, Brown JK, Leano R, Jenkins C, Woodward N, Marwick TH. Use of myocardial deformation imaging to detect preclinical myocardial dysfunction before conventional measures in patients undergoing breast cancer treatment with trastuzumab. Am Heart J 2009; 158(2): 294-301. Mavinkurve-Groothuis AM, Marcus KA, Pourier M, et al. Myocardial 2D strain echocardiography and cardiac biomarkers in children during and shortly after anthracycline therapy for acute lymphoblastic leukaemia (ALL): a prospective study. European heart journal cardiovascular Imaging 2013; 14(6): 562-9. McMurray JJ, Adamopoulos S, Anker SD, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. European journal of heart failure 2012; 14(8): 803-69. Eschenhagen T, Force T, Ewer MS, et al. Cardiovascular side effects of cancer therapies: a position statement from the Heart Failure Association of the European Society of Cardiology. European journal of heart failure 2011; 13(1): 1-10. Bovelli D, Plataniotis G, Roila F, Group EGW. Cardiotoxicity of chemotherapeutic agents and radiotherapy-related heart disease: ESMO Clinical Practice Guidelines. Ann Oncol 2010; 21 Suppl 5: v277-82. Children's Oncology Group. Long-term follow-up guidelines for survivors of childhood, adolescent and young adiult cancers, Version 3.0. 2008. http://www.survivorshipguidelines.org/pdf/LTFUGuidelines.pdf (accessed Nov 22, 2013 2013). Carver JR, Shapiro CL, Ng A, et al. American Society of Clinical Oncology clinical evidence review on the ongoing care of adult cancer survivors: cardiac and pulmonary late effects. J Clin Oncol 2007; 25(25): 3991-4008. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. Hunt SA, American College of C, American Heart Association Task Force on Practice G. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol 2005; 46(6): e1-82. Cheitlin MD, Armstrong WF, Aurigemma GP, et al. ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography--summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). J Am Coll Cardiol 2003; 42(5): 954-70. Ho E, Brown A, Barrett P, et al. Subclinical anthracycline- and trastuzumab-induced cardiotoxicity in the long-term follow-up of asymptomatic breast cancer survivors: A speckle tracking echocardiographic study. Heart 2010; 96(9): 701-7. Yu HK, Yu W, Cheuk DK, Wong SJ, Chan GC, Cheung YF. New three-dimensional speckle-tracking echocardiography identifies global impairment of left ventricular mechanics with a high sensitivity in childhood cancer survivors. J Am Soc Echocardiogr 2013; 26(8): 846-52. Yu W, Li SN, Chan GC, Ha SY, Wong SJ, Cheung YF. Transmural strain and rotation gradient in survivors of childhood cancers. European heart journal cardiovascular Imaging 2013; 14(2): 175-82. Yagci-Kupeli B, Varan A, Yorgun H, Kaya B, Buyukpamukcu M. Tissue Doppler and myocardial deformation imaging to detect myocardial dysfunction in pediatric cancer patients treated with high doses of anthracyclines. Asia Pac J Clin Oncol 2012; 8(4): 36874. Cheung YF, Li SN, Chan GC, Wong SJ, Ha SY. Left ventricular twisting and untwisting motion in childhood cancer survivors. Echocardiography 2011; 28(7): 738-45. Cheung YF, Hong WJ, Chan GC, Wong SJ, Ha SY. Left ventricular myocardial deformation and mechanical dyssynchrony in children with normal ventricular shortening fraction after anthracycline therapy. Heart 2010; 96(14): 1137-41. Mavinkurve-Groothuis AM, Groot-Loonen J, Marcus KA, et al. Myocardial strain and strain rate in monitoring subclinical heart failure in asymptomatic long-term survivors of childhood cancer. Ultrasound in medicine & biology 2010; 36(11): 1783-91. Park JH, Kim YH, Hyun MC, Kim HS. Cardiac functional evaluation using vector velocity imaging after chemotherapy including anthracyclines in children with cancer. Korean circulation journal 2009; 39(9): 352-8. Ganame J, Claus P, Uyttebroeck A, et al. Myocardial Dysfunction Late After Low-Dose Anthracycline Treatment in Asymptomatic Pediatric Patients. Journal of the American Society of Echocardiography 2007; 20(12): 1351-8. Erven K, Florian A, Slagmolen P, et al. Subclinical cardiotoxicity detected by strain rate imaging up to 14 months after breast radiation therapy. International Journal of Radiation Oncology Biology Physics 2013; 85(5): 1172-8. Erven K, Jurcut R, Weltens C, et al. Acute radiation effects on cardiac function detected by strain rate imaging in breast cancer patients. International Journal of Radiation Oncology, Biology, Physics 2011; 79(5): 1444-51. 40. 41. 42. Tsai HR, Gjesdal O, Wethal T, et al. Left ventricular function assessed by twodimensional speckle tracking echocardiography in long-term survivors of hodgkin's lymphoma treated by mediastinal radiotherapy with or without anthracycline therapy. American Journal of Cardiology 2011; 107(3): 472-7. Chang HF, Jiang ZR, Wang XF, Wang ZN. Strain rate imaging in assessment of the relationship between the dose of thoracic radiotherapy and the radiotherapy-induced myocardial damage. [Chinese]. Chinese Journal of Medical Imaging Technology 2009; 25(6): 1032-5. Wang YA, Li GS, Cui HY, Xia DZ. Strain rate imaging in early assesment of thoracic radiotherapy-induced myocardial damage. [Chinese]. Chinese Journal of Medical Imaging Technology 2006; 22(8): 1194-6.