Finding Big Questions in the Details No one could accuse Rebecca
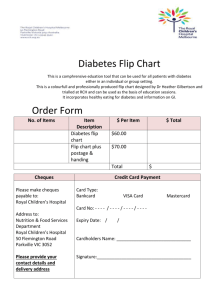
advertisement

Finding Big Questions in the Details No one could accuse Rebecca O’ Connor of taking things at face value. While working as an R.N., O’Connor was surprised to discover red tape prevented willing and able medical workers from helping in the immediate aftermath of the 2004 Asian tsunami. So, she formed a nonprofit to facilitate the placement of medical workers in disaster areas in Sri Lanka after the tsunami, in Pakistan after an earthquake, and in Houston and New Orleans after Hurricane Katrina. Years later, as a research nurse coordinator in the Department of Endocrinology and Diabetes at Seattle Children’s Hospital, O’Connor noticed a high number of young East African immigrants among those treated for type 1 diabetes. “The picture of type 1 diabetes is mostly white, mostly urban, (and hailing) from northern climates,” she said. “To suddenly see all these East African kids was really strange -- I wanted to know what was going on.” Although she originally had no intention of going back to school, in 2009, O’Connor began the PhD program at the UW School of Nursing, with a strong desire to understand the issues behind the rise in type 1 diabetes in East African youth by looking at patients at Seattle Children’s Hospital. During a pilot study, she found that East African immigrant children (children whose families emigrated from Kenya, Uganda, Ethiopia, Somalia, or Eritrea) made up 51% of the Black, type 1 diabetes patients, but only comprised 20% of the overall Black population in Seattle. Initial study results suggested that East African immigrant children may have 2.5 times higher prevalence rates of type 1 diabetes (based on population estimates) and higher rates of family history of type 1 when compared to non-immigrant Black children. Her dissertation research confirmed initial findings that the estimated prevalence rate for type 1 diabetes was nearly four times higher in East African immigrant youth compared to non-immigrant Black youth in King County (6.76/1,000 vs. 1.74/1,000). The research also indicated that these groups had higher rates of family history of type 1 diabetes and suggested differences may exist in the presence of diabetes auto-antibodies at diagnosis for East African immigrant children. O’Connor thinks East African immigrants may be genetically predisposed to developing type 1 diabetes but the overly broad ethnicity classifications used in health care may be masking the disease trend. She points to her own experience in trying to research diabetes among immigrant and non-immigrant youth, all of whom were grouped under the ‘Black/African-American’ race classification. If immigration status and country of origin is not something being tracked, says O’Connor, researchers and clinicians cannot pinpoint group similarities and develop effective interventions. O’Connor would like to expand her study on type 1 diabetes to address the East African community in Seattle. “Vulnerable populations,” she says, “don’t participate frequently in research and don’t benefit from it (which can) lead to further health disparities.” She believes focused, community-engaged clinical research can help build trust in the research process. Eventually, she hopes to develop targeted interventions that are culturally relevant for the East African community and help children with type 1 diabetes better control blood glucose levels.