Open Access version via Utrecht University Repository
advertisement

How changes in lipid metabolism contribute to proinflammation in
cystic fibrosis
Florijn Dekkers, Utrecht University, July 2010
Cystic fibrosis
Cystic fibrosis (CF) is the most common lethal autosomal recessive disorder in Western countries
affecting approximately 40,000 children and young adults in the European Union and a similar
number in the United States (K. A. Becker, Grassme, Zhang, & Gulbins, 2010). It is caused by
mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene (B. Kerem et al.,
1989; Riordan et al., 1989; Rommens et al., 1989) which encodes an ATP-binding cassette located in
the apical membrane of different epithelial cells where it functions as anion transporter (Davis,
Drumm, & Konstan, 1996). CFTR is primarily expressed in the ciliated and submucosal gland epithelial
cells of the lung (Engelhardt, Yankaskas, Ernst, Yang, Marino, Boucher, Cohn, & Wilson, 1992a).
Genetic defects of the CFTR gene, mainly mutations of amino acid 508 and 551, cause many
clinical symptoms of which the most important are pulmonary and gastrointestinal abnormalities (B.
Kerem et al., 1989; Riordan et al., 1989; Rommens et al., 1989). Gastrointestinal symptoms include
malabsorbtion, intestinal obstruction, pancreatic insufficiency and alterations in the liver, like liver
cirrhosis. At present, pulmonary problems are most important for the CF disease course and life
expectancy (K. A. Becker et al., 2010).
CF is characterized by recurrent and eventually chronic pulmonary infections with
Pseudonomas aeruginosa that drive the vast majority of clinical deterioration and life-shortening
mortality encountered in this disease. During disease course, P. aeruginosa undergoes significant
genetic adaptations and selections in the lung resulting in the emergence of a mucoid phenotype
that is the primary determinant of the clinical course of CF (Emerson, Rosenfeld, McNamara, Ramsey,
& Gibson, 2002; Li et al., 2005).
However, it is still incompletely understood how mutation or absence of CFTR promotes
these recurrent and chronic pulmonary infections. Two quite different theories are proposed
regarding defective ion transport and increased bacterial infections in CF patients. These theories
include the ‘salt hypothesis’ and the ‘dehydration hypothesis’ (Boucher, 2007; Guggino, 1999). The
human airway has a mucous layer that traps inhaled bacteria and a thin airway surface liquid layer
(ALS) that provides a microenvironment enabling lung cilia to clear mucus from the airway. This
mucociliary clearance (MCC) system is an important component of the innate immunity to protect
the respiratory tract against pathogens (Com & Clancy, 2009).
The ‘salt hypothesis’ suggests that CFTR regulates production of low NaCl concentrations on
the airway surface in healthy individuals that is essential for the efficient activity of antimicrobial
substances secreted by airway epithelial cells. This layer of antimicrobial substances protects the
epithelium against bacterial infection. In this model, CFTR-deficiency leads to hypertonic salt
concentrations on the respiratory tract that inactivates salt-sensitive antimicrobial peptides enabling
bacteria to multiply and initiate chronic infection (Boucher, 2007; Guggino, 1999; Smith, Travis,
Greenberg, & Welsh, 1996; Zabner, Smith, Karp, Widdicombe, & Welsh, 1998).
On the other hand, the ‘dehydration hypothesis’ suggests that CFTR-deficiency leads to
hypotonic salt concentrations on the airway surface epithelium. As the airways of the lung are very
water-permeable, the epithelium cell absorbs water from the airway surface due to the high salt
concentration within the cell that causes surface ‘dehydration’ (Matsui et al., 1998; Tarran et al.,
2001). The hydration state in the lungs, finely balanced trough sodium absorption by ENaC and
chloride secretion by CFTR, optimizes the volume of the ASL to promote ciliary activity and
mucociliary clearance of inhaled particles. Thus, loss of CFTR function leads to depletion of the ASL
volume and interruption of mucociliary clearance (Com & Clancy, 2009)(Com & Clancy, 2009; Ulrich
et al., 1998; Worlitzsch et al., 2002). This facilitates bacterial colonization, chronic infection and
1
relentless inflammation (Engelhardt, Yankaskas, Ernst, Yang, Marino, Boucher, Cohn, & Wilson,
1992b; Lehrer & Ganz, 2002; Selsted & Ouellette, 2005; Verkman, Song, & Thiagarajah, 2003).
However, changes in salt concentration of mucus lining the bronchial epithelium and
impaired mucociliary clearance can not solely explain the severe pathophysiology observed in CF.
Namely, patients suffering from pseudohypoaldosteonism (PHA) have loss of function mutations in
ENaC that results in altered ALS volume, but they lack lung diseases (E. Kerem et al., 1999).
Furthermore, patients with primary ciliary dyskinesia (PCD) have an impaired mucociliary clearance
system that results in recurrent bacterial infection. However, in contrast to CF, diagnosis is often
delayed until adulthood (Levison et al., 1983).
Many studies have now shown that CF is a very complex disorder in which CFTR dysfunction
leads to, besides changes in the mucociliary clearance system, impaired functions of cationic
antimicrobial peptides (Goldman et al., 1997), neutrophils and macrophages (Campodonico, Gadjeva,
Paradis-Bleau, Uluer, & Pier, 2008; Di et al., 2006; Painter et al., 2008; Roghanian & Sallenave, 2008)
and alterations in bacterial internalization into lung epithelial cells (Bajmoczi et al., 2009; Bajmoczi,
Gadjeva, Alper, Pier, & Golan, 2009; Painter et al., 2008), frequency of cell death induced by
pathogens and lipid metabolism (Worgall, 2009).
CF and proinflammation
Although several studies address that CFTR-deficient and normal cells have equal activation of
inflammatory pathways (M. N. Becker et al., 2004; Hybiske et al., 2007), many studies imply that CF
cells and lung tissues have an excessive proinflammatory status. Defects of CFTR have been
associated with a marked increase of proinflammatory cytokines, such as TNF-α, IL-6, IL-1β and IL-17
(Dubin, McAllister, & Kolls, 2007; Osika et al., 1999) and the neutrophil chemoattractant and
activator IL-8, which recruits large numbers of neutrophils into the airways (Ratjen & Doring, 2003).
There is also in vivo evidence for reduced production of the anti-inflammatory cytokine IL-10
(Bonfield et al., 1995; Bonfield, Konstan, & Berger, 1999). In addition, many studies report that CF
airway epithelial cells have increased activation of the proinflammatory transcription factor NF-κB
(Bodas & Vij, 2010; Carrabino et al., 2006; Joseph, Look, & Ferkol, 2005; Schroeder et al., 2002; Vij,
Mazur, & Zeitlin, 2009).
This proinflammatory status, however, is regardless of any infections, because CFTRdefective cell lines spontaneously develop similar proinflammatory features under sterile conditions
(Perez et al., 2007; Verhaeghe, Remouchamps, Hennuy, Vanderplasschen, Chariot, Tabruyn, Oury, &
Bours, 2007a). Furthermore, in the absence of pathogens, CF patients present exaggerated
inflammation in the respiratory tract (Dakin et al., 2002; Khan et al., 1995; Muhlebach, Stewart,
Leigh, & Noah, 1999) and a high density of neutrophils and macrophages (Bergoin et al., 2002; Roum,
Buhl, McElvaney, Borok, & Crystal, 1993a). These data suggest that the proinflammatory state in CF
results from intrinsic activated inflammatory pathways in CFTR-deficient epithelial cells. Although the
origin of these spontaneously initiated inflammatory cascades is still incompletely defined, possible
causes have been discussed (summarized in figure 1).
Intrinsic alterations and proinflammation
There are over 1,600 mutations described for CFTR of which the ΔF508 mutation is present in about
70% of the patients with CF (Hampton & Stanton, 2010). ΔF508CFTR is incorrectly folded and
accumulates in the ER-Golgi intermediate compartment (Gilbert, Jadot, Leontieva, Wattiaux-De
Coninck, & Wattiaux, 1998) that leads to disrupted ER function, called ‘ER stress’(Rao, Ellerby, &
Bredesen, 2004). Under ER stress conditions, the unfolded protein response (UPR) and ER-associated
degradation (ERAD) pathways are activated to reduce synthesis of newly formed proteins and
increase degradation of incorrectly-folded proteins. When these responses do not overcome ER
stress, the ER-overload response (EOR) is activated that leads to apoptosis (Lai, Teodoro, & Volchuk,
2007). Indeed, accumulation of ΔF508CFTR in the ER activates the UPR (Kerbiriou, Le Drevo, Ferec, &
2
Trouve, 2007) that results in decreased expression of CFTR (Bartoszewski, Rab, Jurkuvenaite et al.,
2008; Bartoszewski, Rab, Twitty et al., 2008). ΔF508CFTR is detected in the cytosol and within the ER
membrane by components of the ERAD system which induce removal of ΔF508CFTR from the ER and
proteasome-dependent degradation in the cytosol (Meusser, Hirsch, Jarosch, & Sommer, 2005;
Turnbull, Rosser, & Cyr, 2007). Accumulation of misfolded CFTR in the ER contributes to endogenous
activation of NF-κB (Verhaeghe, Remouchamps, Hennuy, Vanderplasschen, Chariot, Tabruyn, Oury, &
Bours, 2007b; Weber, Soong, Bryan, Saba, & Prince, 2001). Furthermore, rescue of ΔF508CFTR to the
plasma membrane by inhibition of VPC, an ERAD component, is associated with inhibition of NF-κB
activation. As VPC had been shown to be upregulated in CF bronchial epithelial cells from ΔF508CFTR
homozygote patients compared to wild type cells, this could in part explain the exaggerated NF-κB
response in CFTR-deficient cells (Vij et al., 2009). It has also been proposed that the constitutive NFκB activation could be the consequence of EOR induction by CFTR accumulation in ER membrane
(Knorre, Wagner, Schaefer, Colledge, & Pahl, 2002; Rottner, Kunzelmann, Mergey, Freyssinet, &
Martinez, 2007). So, CFTR-induced ER stress could be a key element in the enhanced
proinflammatory response in CF cells.
Besides sequestration of CFTR in the ER, it has been shown that defective CFTR leads to
alterations in calcium homeostasis. CF cells show an expanded ER and enhanced calcium mobilization
from the ER (Antigny, Norez, Becq, & Vandebrouck, 2008; Ribeiro et al., 2005; Ribeiro, Paradiso,
Carew, Shears, & Boucher, 2005). Tabary et al. (Tabary et al., 2006) hypothesized that calcium
mobilization may regulate NF-κB activation. They show that inflammatory cytokine IL-1β induces an
increase of calcium release from the ER that was accompanied by NF-κB activation in living airway CF
epithelial cells. The IL-1β-induced calcium response is decreased by depletion of calcium stores from
the ER or inhibition of NF-κB activation. This suggests that inflammatory cytokines control the
calcium release in CF epithelial cells that leads to activation of NF-κB. This, in turn, leads to the
production of inflammatory cytokines that stimulate the cycle of calcium release and NF-κB
activation (Tabary et al., 2006).
CFTR regulates the transport of the antioxidant glutathione (GSH) between cells and the
extracellular environment (Linsdell, Evagelidis, & Hanrahan, 2000). Several studies noted alterations
in GSH concentration and transport in CFTR-deficient cells. While some studies note low levels of
GSH in lung fluid of CF patients, plasma or mitochondria of murine or human lung epithelial cells
(Gao, Kim, Yankaskas, & Forman, 1999; Roum, Buhl, McElvaney, Borok, & Crystal, 1993b; Velsor, van
Heeckeren, & Day, 2001), others found increased intracellular GHS levels in epithelial cells
transfected with ΔF508CFTR (Jungas et al., 2002). Low GSH levels in CF cells may be associated with
NF-κB activation sequential proinflammation, as GSH inhibits degradation of IκB, an inhibitor of NFκB (Haddad, 2002; Rottner, Freyssinet, & Martinez, 2009).
Furthermore, CFTR-deficiency has been associated with elevated levels of cellular and
mitochondrial reactive oxygen species (ROS) (Brown, McBurney, Lunec, & Kelly, 1995; Brown, Wyatt,
Price, & Kelly, 1996; Collins et al., 1999; Velsor et al., 2001; Velsor, Kariya, Kachadourian, & Day,
2006). Elevated ROS levels in CF may either induce cellular stress that inhibits CFTR maturation or
activate MAPK signaling pathways (Genestra, 2007; Rab et al., 2007). As MAPK regulates
transcription of pro-inflammatory mediators in CF cells, increased levels of ROS possibly contribute to
the initiation or maintenance of enhanced inflammation observed in CFTR-deficient cells (Verhaeghe,
Remouchamps, Hennuy, Vanderplasschen, Chariot, Tabruyn, Oury, & Bours, 2007c).
3
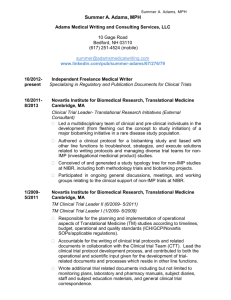
Figure 1. Intrinsic alterations
in CFTR-defective cells that
lead to proinflammation.
Besides the sequestration of CFTR in the ER and changes in calcium mobilization, GSH
content and ROS levels in CF cells, several recent in vitro and in vivo studies describe that alterations
in lipid metabolism are critically involved in enhanced activation of inflammatory pathways in CF
cells. The two main findings of these studies are that defective CFTR is associated with either
decreased levels of the nuclear peroxisome proliferator-activated receptor gamma (PPAR-γ)
(Andersson, Zaman, Jones, & Freedman, 2008a; Gulbins, 2010; Harmon et al., 2010; Maiuri et al.,
2008; Ollero et al., 2004; Perez et al., 2008) that regulates expression of genes involved in lipid
metabolism and inflammation (Berger & Moller, 2002; Jiang, Ting, & Seed, 1998) or changes in
sphingolipid metabolism, in particular ceramide metabolism (K. A. Becker et al., 2009; Guilbault et al.,
2008; Guilbault et al., 2009; Riethmuller et al., 2009; Teichgraber et al., 2008). Sphingolipids are
important signaling molecules that can modulate inflammatory responses (Nixon, 2009; Pettus,
Chalfant, & Hannun, 2004). The present review highlights these two topics and gives an overview of
how intrinsic cellular alterations of PPAR-γ levels and sphingolipid metabolism caused by defective
CFTR may contribute to increased inflammatory activity in CF tissues.
PPAR-γ signaling in cystic fibrosis
PPAR-γ is a nuclear receptor that regulates the expression of a number of genes involved in cellular
differentiation, apoptosis and lipid metabolism. In general, its activation augments lipid catabolism
and induces differentiation of fibroblasts into adipocytes (Berger & Moller, 2002). Other regulatory
functions of PPAR-γ include the modulation of inflammatory responses and the enhancement of
insulin sensitivity. PPAR-γ regulates inflammation via inhibition of AP-1, STAT, and NFκβ pathways in
monocytes, macrophages and epithelial cells that results in inhibition of proinflammatory cytokines
secretion, such as TNF-α, IL-6 and IL-1 (Jiang et al., 1998; Nagy, Tontonoz, Alvarez, Chen, & Evans,
1998; Ricote, Li, Willson, Kelly, & Glass, 1998).
Ollero et al. (Ollero et al., 2004) noted for the first time a connection between PPAR-γ
signaling and the pathophysiological inflammation in cystic fibrosis. They analyzed PPAR-γ mRNA and
protein expression as well as subcellular distribution of PPAR-γ in colonic mucosa, ileal mucosa,
adipose tissue, lung, and liver tissue from wild-type and CFTR-/- mice. Results demonstrated a
decrease in PPAR-γ expression and function in CFTR-regulated tissues (colon, ileum, and lung) from
CFTR-/- mice compared to wild-type mice that associates PPAR-γ with the abnormal function of CFTR.
4
They suggested that the decrease in expression and function of PPAR-γ, as being a repressor of
inflammatory responses and activator of lipid catabolism, could explain the excessive host
inflammatory response and alterations in lipid metabolism observed in CF cells (Ollero et al., 2004).
Others further focused on the molecular link between defected CFTR and the excessive
inflammatory responses typical of CF airways and targeted the role of the defective CFTR on PPAR-γ
in sterile conditions to exclude the influence that recurrent infections might have on the lung
epithelium and inflammation. Defective CFTR induced a remarkable up-regulation of tissue
transglutaminase (TG2) in nasal polyp mucosa from CF patients and CFTR-defective bronchial
epithelial cell lines. The increased TG2 activity leads to functional sequestration of the antiinflammatory PPAR-γ and an increase of classic parameters of inflammation, such as TNF-α, tyrosine
phosphorylation and mitogen-activated protein kinases (MAPKs). These results highlight a central
role for TG2 in the molecular mechanisms that underlie CF inflammation and suggest that TG2
inhibition could become a therapeutic target to control inflammation in CF and possibly in other
chronic inflammatory diseases (Maiuri et al., 2008).
The cytokines IL-8, IL-6 and GM-CSF as well as other features of the CF inflammatory
response such as ICAM expression and release of MMPs, are most consistently in excess in cystic
fibrosis and depend on NF-κB signaling. Besides, several studies have shown increased NF-κB
activation in CF airway epithelial cells (Bodas & Vij, 2010; Joseph et al., 2005; Schroeder et al., 2002;
Vij et al., 2009). Based on the results that PPAR-γ is a inhibitor of NF-κB activation and that PPAR-γ
expression and function is reduced in CF tissues (Ollero et al., 2004), Perez et al. (Perez et al., 2008)
studied whether PPAR-γ modulates inflammation of airway epithelial cells via NF-κB. Cell models of
CF airway epithelium were used to evaluate PPAR-γ expression and binding to NF-κB under basal
conditions and conditions of inflammation by stimulation with P. aeruginosa or TNFα/IL-1β. In
accordance with the decrease in PPAR-γ function observed in CFTR-regulated tissues of CFTR-/- mice
(Ollero et al., 2004), experiments using nasal polyp mucosa from CF patients or CFTR-defective
bronchial epithelial cell lines (Maiuri et al., 2008) indicated that PPAR-γ quantity or function is
reduced in CF airway epithelial cells in culture compared to normal cells. In addition, they confirm
interaction between PPAR-γ and NF-κB and show that inflammatory stimulation causes changes in
NF-κB or in PPAR-γ that reduce their interaction, particularly in CF cells. The specific mechanism by
which the PPAR-γ-NF-κB interaction is reduced by proinflammatory stimuli is not clear, but was
suggested to involve ERK-mediated conformational changes in PPAR-γ that alters its binding to NFκB. The reduced interaction of PPAR-γ and NF-κB may contribute to the excess activation of genes
driven by NF-κB and enhanced inflammation in CF.
A recent study (Harmon et al., 2010) shows that a defect in PPAR-γ function in colonic
epithelial cells and whole lung tissue from CFTR-/- mice contributes to a pathologic gene expression.
Analysis of downregulated genes revealed significant enrichment for genes involved in lipid
metabolism and analysis of downregulated genes revealed enrichment for genes linked to
inflammatory responses in CFTR-deficient mice. Lipodomic analysis of colonic epithelial cells suggests
that this defect in PPAR-γ function results from reduced amounts of PPAR-γ ligands, which include
15-keto-prostaglandin E2 (15-keto-PGE2). They studied why the production of 15-keto-PGE2 is
reduced in CFTR-deficient mice and traced the defect to a significant reduction in the expression of
15-hydroxyprostaglandin dehydrogenase (HPGD), the enzyme that converses PGE2 to 15-keto-PGE2
(Harmon et al., 2010).
The functional defect in PPAR-γ seems to contribute to the intestinal phenotype of CFTR-/mice, as the synthetic PPAR-γ ligand roziglitazone lowered mortality and disease severity observed in
CFTR-deficient mice. Roziglitazone treatment corrected a large number of down- and upregulated
genes in CFTR deficient colonic epithelial cells, indicating that multiple genes contribute to
the CF phenotype. Overexpression of inflammatory responses and accumulation of airway mucus are
two important CF characteristics that are inhibited by roziglitazone in a PPAR-γ-dependent way
5
(Harmon et al., 2010). More about the therapeutic value of this and other PPAR-γ ligands for cystic
fibrosis treatment is discussed below.
Although inhibition of inflammation is a well established function of PPAR-γ (Lewis et al.,
2001; Su et al., 1999), this study describes for the first time a role for PPAR-γ in regulation of mucus
production (Fig. 2). As roziglitazone increases the expression of carbonic anhydrases in CFTR-/- cells,
they hypothesize that this increased expression enhances bicarbonate secretion resulting in reduced
mucus viscosity (Gulbins, 2010; Harmon et al., 2010) that is in agreement with other articles that
note that changes in pulmonary mucus is possibly due to defects in bicarbontate transport (Garcia,
Yang, & Quinton, 2009; Quinton, 2008). High viscous mucus may negatively affect the migration of
neutrophils (Matsui et al., 1998; Matsui et al., 2005) and secretion of antimicrobial peptides such as
β-defensins and cathelicidins that facilitates bacterial colonization, chronic infection and relentless
inflammation (Engelhardt, Yankaskas, Ernst, Yang, Marino, Boucher, Cohn, & Wilson, 1992b; Lehrer &
Ganz, 2002; Selsted & Ouellette, 2005; Verkman et al., 2003).
Figure 2. Regulation of mucus production in cystic fibrosis by the 15-keto-PGE2-PPAR-γ system. In wild type
cells, the ligand 15-keto-PGE2 binds to the PPAR-γ to induce gene expression that results in synthesis of
carbonic anhydrases that regulate mucus viscosity. In CFTR-deficient cells, the 15-keto-PGE2-PPAR-γ system is
impaired that results in a reduced expression of carbonic anhydrases and eventually in accumulation of viscous
mucus (Gulbins, 2010)(Gulbins, 2010; Harmon et al., 2010).
Fatty acids and PPAR-γ
The first documentations of altered fatty acid profiles in cystic fibrosis are the result of studies
carried out more than 40 years ago. They noted decreased linoleic acid and increased myristic,
palmitoleic, stearic and oleic fatty acids in CF cells (KUO, HUANG, & BASSETT, 1962; Rosenlund, Kim,
& Kritchevsky, 1974). Many consecutive studies confirmed these initial findings and showed, in
addition, altered plasma levels of docosahexaenoic acid (DHA), a n-3 fatty acid, and arachidonic acid
(AA) (Christophe, Robberecht, De Baets, & Franckx, 1992; Roulet, Frascarolo, Rappaz, & Pilet, 1997).
DHA levels are decreased and arachidonic acid levels increased in plasma of cystic fibrosis patients
(Roulet et al., 1997) as well as in CFTR regulated tissues from CFTR -/- mice (Freedman et al., 1999).
Alterations in fatty acid profiles are significant enough that the product of linoleic acid and DHA can
distinguish cystic fibrosis patients from healthy controls (Batal et al., 2007).
PPARs are activated by polyunsaturated fatty acids such as DHA as well as fatty acid
metabolites that are produced during inflammatory responses. Thus, inflammatory mediators
activate PPARs thereby initiating the resolution phase of inflammation (Devchand et al., 1996).
Correction of decreased DHA levels with high doses of orally administered DHA reversed the
6
excessive inflammatory response in the lungs and bile ducts of CFTR-/- mice (Blanco et al., 2004;
Thomas et al., 2000). However, the exact mechanisms by which DHA ameliorates the inflammatory
response as well as how CFTR dysfunction leads to fatty acid abnormalities are still incompletely
defined.
While most research to date has been focusing on the dysregulated immune response of
airway epithelial cells, a recent study used peritoneal macrophages to examine the effect of DHA on
immune responses induced by LPS. They showed that PPARs as well as liver X receptors (LXR), which
resemble function of PPARs in regulating lipid metabolism and inhibiting proinflammatory cytokine
production, are linked to primed CF-dependent inflammation in macrophages (Andersson, Zaman,
Jones, & Freedman, 2008b). In agreement with the previous study of PPAR-γ expression in CFTR
regulated tissues from CFTR-/- mice (Ollero et al., 2004), mRNA expression of PPAR-γ was
significantly lower in CF macrophages. They suggested that defective regulation of proinflammatory
pathways due to impaired expression and function of PPARs and LXRs in macrophages may
contribute to the excessive inflammation in CF. Treatment of DHA increased PPAR activity, decreased
NF-κB activity and decreased TNF-α secretion from CF macrophages suggesting that DHA acts trough
PPARs to inhibit CF associated inflammation (Andersson, Zaman, Jones, & Freedman et al., 2008b).
Furthermore, these results increase evidence that macrophages are involved in the defective
immune regulation in CF.
Ollero et al. (Ollero et al., 2004) suggested that decreased DHA plasma levels observed in
CFTR-deficient cells (Freedman et al., 1999; Roulet et al., 1997) could result from decreased
expression and function of PPAR-γ observed in CF tissues. Namely, the biosynthesis of DHA occurs in
peroxisomes and requires a β-oxidation step. Since PPAR-γ regulates expression of a key element in
fatty acid β-oxidation, called acyl coenzyme-A oxidase (Dreyer et al., 1992), a decrease in PPAR-γ
function would affect peroxisomal function possibly resulting in low DHA levels (Ollero et al., 2004).
As CFTR defects are connected with decreased PPAR-γ function, these defects might indirectly
account for low DHA levels.
Several studies assessed the clinical benefit of supplementation with the n-3 fatty acids DHA
and eicosapentaenoic (EPA). Together these studies demonstrate that supplementation can increase
DHA and EPA levels, but their clinical efficacy remains to be established (Worgall, 2009).
PPAR-γ ligands
As decreased PPAR-γ expression and function seems to contribute to the proinflammatory state in
CFTR regulated cells, PPAR ligands or agonists have been considered for treatment of cystic fibrosis
on the basis of their anti-inflammatory properties (Nichols, Konstan, & Chmiel, 2008). PPAR-γ
agonists have been shown to inhibit the expression of the proinflammatory cytokine TNF-α and block
the NF-κβ proinflammatory signaling pathway (Ollero et al., 2004).
The thiazolidinedione (TZD) drugs rosiglitazone and pioglitazone are oral insulin-sensitizing
agents used for glycemic control in patients with Type 2 diabetes (Yki-Jarvinen, 2004). The same
drugs are currently investigated for their prospective benefits in fighting other human diseases, such
as hypertension, atherogenesis, inflammation, and cancer. The therapeutic effects of rosiglitazone
and pioglitazone are generally attributed to their action as synthetic high-affinity ligands of PPAR-γ
(Tontonoz & Spiegelman, 2008).
Harmon et al. (Harmon et al., 2010) showed that rosiglitazone decreased overexpression of
inflammatory responses and accumulation of airway mucus. These findings indicate that drugs that
activate PPAR-γ may (partly) resolve abnormal lung symptoms of CF patients by normalizing mucus
production, preventing obstruction in the lung and inhibiting the exaggerated immune response.
Besides rosiglitazone, the function of pioglitazone was tested in a complex in vivo model, in
which CF and wild-type mice were challenged with P. aeruginosa. The relative and absolute numbers
of neutrophils, as well as levels of TNF-α, IL-1β, and macrophage inflammatory protein 2 (MIP-2)
were significantly reduced in P. aeruginosa-challenged CF mice treated with pioglitazone compared
7
to non-treated CF mice. They note pioglitazone treatment is capable of normalizing lung
inflammation in CF mice. The same study shows that troglitazone can drastically reduce the
enhanced NF-κB activation observed in CF airway epithelium cells. This is explained by the finding
that PPAR-γ activation by ligand binding can prevent excess activation of NF-κB. They discuss that this
pioglitazone-mediated reduction in NF-kB activation observed in vitro may also contribute to the
pioglitazone-mediated inhibition of inflammatory response to infection with P. aeruginosa in CF mice
in vivo (Perez et al., 2008).
Together, these findings indicate that drugs that modify PPAR-γ signaling may be useful for
treating the pathofysiological lung symptoms in CF patients. However, additional long term studies in
CFTR-deficient mice or other CF models are required to prove the clinical benefits of PPAR-γ ligands.
Sphingolipids
Besides that decreased levels of PPAR-γ may contribute to pathologic inflammation in CF cells,
several studies highlight the role for sphingolipids in regulating CFTR-dependent inflammation. Lipids
have a variety of biological roles; they serve as highly concentrated energy stores, fuel molecules,
signal molecules and constituents of membranes. The three major kind of amphipathic membrane
lipids are phospholipids, glycolipids and steroids (cholesterol). The platform on which phospholipids
are build may be glycerol, a 3-carbon alcohol or sphingosine. The membrane lipids that contain a
sphingosine backbone are called sphingolipids. In humans, sphingomyelin is believed to be the only
shingosine-based cell membrane phospholipid. Sphingolipids are found in the plasma membrane of
all eukaryotic cells. During the de novo synthesis of sphingolipids, Palmitoyl CoA and serine condense
to form dehydrosphingosine, which is then converted into sphingosine (Biochemistry). Sphingolipids
were long regarded primarily as structural components of cell membranes. (Hannun & Obeid, 2008)
It is now clear that altered levels of bioactive lipid can have profound consequences on cellular
behavior and cell phenotype (Cuvillier et al., 1996). Recently, several studies have noted that
spingolipids have a profound role in regulation of inflammation (Pettus et al., 2004). Recent findings
indicate that CFTR affects the metabolism of sphingolipids (Guilbault et al., 2008; Hamai, Keyserman,
Quittell, & Worgall, 2009; Teichgraber et al., 2008; Xiao & Ghosh, 2005). Changes in sphingolipid
metabolism are, besides altered PPAR-γ signaling, presumably of great importance with regard to the
mechanism that causes inflammation and susceptibility to infection in cystic fibrosis.
The sphingomyelin cycle involves degradation and re-systhesis of sphingomyelin via a
number of intermediates (Fig. 3). The breakdown of sphingomyelin is regulated by acid, neutral or
secretory sphingomyelinase (SMase) that results in the generation of ceramide. Acid SMase is
primarily located in lysosomes and secretory lysosomes, secretory SMase is targeted to the golgi
apparatus and neutral SMase is a membrane-bound protein. Acid SMase hydrolyzes sphingomyelin
to ceramide, preferentially at an acidic pH, but is also able to hydrolyze sphingomyelin under almost
normal conditions. Ceramide can be either further degraded to sphingosine by ceramidase or
phosphorylated to ceramide-1-phosphate (C1P) by ceramide kinase. Like ceramide, sphingosine can
be phosphorylated to sphingosine 1-phosphate (S1P) by sphingosine kinase (SK). S1P can be
dephosphorylated by sphingosine phosphatase or degraded by S1P lyase resulting in S1P removal
from the cycle. Sphingomyelin can be re-synthesized from sphingosine by ceramide synthase
(converting sphingosine to ceramide) and sphingomyelin synthase (converting ceramide to
sphingomyelin). Ceramide is not only generated by the actions of SMases in the membrane, but also
by alternative routes, such as de novo pathways via ceramide synthase or the hydrolysis of complex
glycosylated lipids (Nixon, 2009; Pettus et al., 2004). The de novo synthesis begins with the
condensation of serine with palmitoyl-CoA and is catalyzed in the cytoplasmic leaflet of the
endoplasmic reticulum (K. A. Becker et al., 2010). So, breakdown of sphingomyelin leads to the
production of ceramide and sphingosine that can both be either phosphorylated or not.
8
Figure 3. The sphingomyelin cycle.
Schematic representation of the
metabolic cycling of sphingomyelin that
involves its degradation and re-systhesis
via a number of intermediates. Enzymes
for each reaction are depicted in red
{{122 Nixon,G.F. 2009}}.
Activation of the sphingomyelin cycle is important for cellular signaling
(Cuvillier et al., 1996)SMases are activated by different stimuli, such as inflammatory cytokines, Gcoupled-receptors, growth factors or cell stress. The pool of acid SMase in secretory lysosomes
seems to participate in signal transduction events (Bao et al., 2010; Grassme et al., 2001; Herz et al.,
2009) as activation of several receptors, such as CD95, DR5, CD40, and the platelet-activating factor
(PAF) receptor, but also some bacterial and viral infections or stress stimuli, trigger the fusion of
secretory lysosomes with the cell membrane to expose acid SMase in cell membrane rafts at the
membrane outer leaflet where the enzyme generates ceramide (Cremesti et al., 2001; Dumitru &
Gulbins, 2006; Goggel et al., 2004; Grassme et al., 2000; Grassme et al., 2001; Grassme, Jendrossek,
Bock, Riehle, & Gulbins, 2002; Grassme et al., 2003; Rotolo et al., 2005). Rafts are small distinct
membrane microdomains that are enriched with spingolipids and cholesterol. Ceramide formation
spontaneously induces fusion of small sphingolipid-enriched lipid rafts into larger membrane
platforms that may act to assemble signaling complexes (Grassme et al., 2003). CD95, DR5 and CD40
have been shown to cluster in ceramide-rich membrane domains upon their activation (Dumitru &
Gulbins, 2006; Grassme et al., 2001; Grassme et al., 2002). Besides assembly of lipid rafts, ceramide
might also mediate intracellular signaling via direct interaction with proteins that contain a ceramide
binding domain (Nixon, 2009; Zhang et al., 1997). Ceramide can be phosphorylated by ceramide
kinase in various intracellular locations. C1P has been shown to directly interact with signaling
proteins (Pettus et al., 2004). Activation of G-coupled receptors, growth factor receptors and
cytokine receptors results in the production of S1P. Unlike ceramide and C1P that are only located in
cell membranes, S1P also occurs naturally in plasma at high concentrations (Alemany, van Koppen,
Danneberg, Ter Braak, & Meyer Zu Heringdorf, 2007).
Spingolipids in inflammation and bacterial infection
Many studies have demonstrated that shingolipids have specific functions in regulating inflammatory
responses and may themselves initiate parts of the inflammatory process (summarized in figure 4)
(Nixon, 2009). TNF and LPS can activate acid SMase that results in ceramide production and
activation of acid SMase leads to activation of the pro-inflammatory transcription factor NF-κB that
promotes production of proinflammatory cytokines, such as IL-1β, IL-6 and IL-8, and proinflammatory enzymes, such as COX-2 (Xiao & Ghosh, 2005). COX-2 catalyzes the breakdown of
arachidonic acid to eicosanoids, including pro-inflammatory leukotriens and prostaglandins (PGs)
9
(Pettus et al., 2004). Ceramide generated by TNF-induced activation of neutral SMase leads to
increased activity of cPLA2 that generates arachidonic acid from phospholipids (Manthey &
Schuchman, 1998). Besides NF-κB, ceramide can also upregulate CCAAT/enhancer binding proteins
(c/EBP) that induces gene expression of several pro-inflammatory cytokines, including TNF, IL-1β, IL-6
and IL-8 (Poli, 1998). As little is known about the regulation of ceramide kinase, it is difficult to assess
whether some of the effects ascribed to ceramide may be the result of ceramide conversion to C1P
or even due to conversion to S1P (Nixon, 2009). Presumably, C1P is predominantly involved in
inflammation by activating cPLA2 (Pettus et al., 2004). Intracellular SK activation can produce S1P in
response to different stimuli, including IgE, TNF and LPS. In mast cells C1P is exported from the cell
via ATP-binding cassette binding family of transport proteins, such as CFTR, where it can have
autocrine or paracrine effects. It is possible that regulation of S1P receptors in the membrane in
different cell types is involved in inducing S1P-mediated inflammatory effects. In fibroblasts and lung
epithelial cells, SK1 was dependent for TNF-induced up-regulation of COX-2 and subsequent PGE2
production. Furthermore, S1P activates cPLA2 in lung epithelial cells to produce arachidonic acid via
an S1P receptor. Some in vivo studies show that S1P receptors are important for COX-2-induced
inflammation (Nixon, 2009).
Figure 4. Main signaling pathways that show
the potential involvement of sphingolipids in
inflammation. Several factors can induce
sphyngomyelinases (SMases) or sphingosine
kinase (SK) that leads to the production of
respectively ceramide/ceramide 1-phospate
(C1P) or sphingosine 1-phosphate (S1P). These
sphingolipids in turn induce the enzymes cPLA 2
and COX-2 and the transcription factors c/EBP
and NF-κB. The overall response of activation of
the sphingolipid cycle is production of proinflammatory mediators, including cytokines,
chemokines
and
prostaglandins
{{122
Nixon,G.F. 2009}}.
Several studies demonstrate that acid SMase is activated and ceramide released when cells are
infected with bacteria and that this increased ceramide synthesis is essential for bacterial
internalization (K. A. Becker et al., 2010). Is has also been shown that activation of acid SMase and
the release of ceramide in murine or human lung epithelial cells and macrophages is triggered by
infection with P. aeruginosa. The release of ceramide upon infection with P. aeruginosa results in the
formation of ceramide-rich membrane platforms that occurred as early as 5-10 minutes after
infection. These lipid membrane platforms colocalize with P. aeruginosa and are required for cellular
apoptosis and bacterial internalization. These events did neither occur in acid SMase-deficient cells
nor in mice lacking acid SMase upon P. aeruginosa infection. In addition, these acid SMase-deficient
mice show an uncontrolled and exaggerated release of cytokines upon infection. These results
highlight the importance for ceramide-rich membrane platforms in mammalian epithelial cell
infection with P. aeruginosa (Grassme et al., 2003). So,
10
Ceramide and CFTR
Kowalski and associates showed that localization of CFTR into lipid rafts in both human and canine
epithelial cells is essential for P. aeruginosa-induced internalization, NF-κB activation and apoptosis
(Kowalski & Pier, 2004). Likewise, Grassme et al. tested whether the CD95 receptor and CFTR cluster
in ceramide-enriched membrane platforms upon P. aeruginosa infection, as both molecules are
important for bacterial internalization (Bajmoczi et al., 2009; Grassme et al., 2000), and showed
clustering of CD95 and CFTR in ceramide-rich membrane domains upon cellular infection (Grassme et
al., 2003). CD95 is crucial for induction of cellular apoptosis and bronchial epithelial cell death in vivo
upon infection with P. aeruginosa and a defect in apoptosis in animals lacking CD95 results in a high
susceptibility to P. aeruginosa (Grassme et al., 2000). Interestingly, recent studies note that cystic
fibrosis patients have demonstrated that allelic variation of the CD95 gene modulates the
manifestiation in CF (Kumar et al., 2008). These findings suggest that CD95-mediated signaling or
apoptosis is involved in P. aeruginosa infection in CF patients. Clustering of CD95 and CFTR in
ceramide-enriched membrane rafts upon infection might be involved in P. aeruginosa internalization
and cellular apoptosis (K. A. Becker et al., 2010).
Recently, Yu et al. studied the role for acid SMase in CFTR-deficient cells and in the lungs of
CFTR-deficient mice. They confirmed that infection with P. aeruginosa triggers the activation of acid
SMase and the release of ceramide. In addition, they found that activation of acid SMase and
sequential release of ceramide do not occur after P. aeruginosa infection in cells that are deficient of
CFTR. Cells lacking CFTR or cells in which acid SMase was suppressed by transfection with small
interfering RNA (siRNA) show to fail P. aeruginosa internalization. CFTR-deficient cells did not
respond to P. aeruginosa by inducing apoptosis upon lung infection. P. aeruginosa-induced apoptosis
in CFTR-deficient cells could be restored by adding exogenous SMase (Yu et al., 2009). These results
confirm the importance of CFTR in SMase induction and sequential ceramide formation upon
infection with P. aeruginosa.
Increased ceramide levels in CF
Teichgraber at al. further studied the role for sphingolipids in the pathogenesis in cystic fibrosis and
confirmed that that ceramide accumulation is critically involved in CF pathogenesis. They observed
excessive ceramide accumulation in respiratory tract epithelium and submucosa and in alveolar
macrophages of CFTR-deficient mice, but not in wild type mice (Fig. 5). Ceramide predominantly
located to intracellular vesicles in CFTR-deficient lung epithelial cells compared to normal cells.
Besides ceramide accumulation in pulmonary cells of CFTR-deficient mice, accumulation of ceramide
was found in the membrane of nasal epithelial cells, respiratory epithelial cells and submucosa
glands of CF patients, while ceramide levels were normal in the respective cells or tissues from
healthy individuals (Teichgraber et al., 2008).
They attribute the accumulation of ceramide to an altered pH in intracellular vesicles in CFTRdeficient cells (Teichgraber et al., 2008). The process of sphingomyelin degradation to ceramide and
eventually to sphingosine is thought to be located primarily in lysosomes (Lahiri & Futerman, 2007).
The CFTR-mediated acidification of intracellular vesicles is crucial for the correct regulation of
ceramide production by acid SMase and acid ceramidase (Teichgraber et al., 2008), presumably
through the provision of counter ions to permit higher H+ concentrations within the vesicle (Di et al.,
2006; Hara-Chikuma et al., 2005). Alkalinization of CFTR-deficient vesicles in respiratory cells of CFTRdeficient mice results in an imbalance of acid SMase and acid ceramidase causing net accumulation
of ceramide. Degradation of acid SMase by amitriptyline or genetic heterozygosity of acid SMase
almost normalizes pulmonary ceramide levels in CFTR-deficient mice. (Teichgraber et al., 2008).
11
Figure 5. CFTR deficiency leads to ceramide accumulation in bronchial epithelial cells. Paraffin sections of
lungs from CFTR-deficient and wild type mice were stained Cy3-conjugated anti-ceramide antibodies and
analyzed by confocal microscopy. Results show that ceramide accumulation in greatly enhanced in the
epithelial cells of CFTR-deficient mice compared to those in wild type mice.
In accordance with previous studies (Emerson et al., 2002; Li et al., 2005; Worlitzsch et al., 2002),
CFTR-deficient mice were significantly more susceptible to P. aeruginosa infection compared to wild
type mice. Pharmacological or genetic inhibition of acid SMase protected mice lacking CFTR from
pulmonary P. aeruginosa infections and reduced P. aeruginosa-induced mortality (Teichgraber et al.,
2008). This increased susceptibility to P. aeruginosa may be caused by the by an imbalance between
proinflammatory and anti-inflammatory cytokines that results from altered lipid metabolism (K. A.
Becker et al., 2010). CFTR-deficient mice show a constitutive increase in expression of IL-1 and
keratinocyte-derived chemokine (KC, the mouse homolog of human IL-8) and an increase in
macrophage and neutrophil cell numbers in their lungs. Inhibition of acid SMase in the lungs of CFTRdeficient mice normalizes the expression of the proinflammatory cytokines IL-1 and KC as well as the
number of macrophages and neutrophils (Teichgraber et al., 2008). As mentioned previously,
ceramide activates the transcription factor NF-κB that regulated expression of IL-1 and IL-8 (Fig. 4).
Therefore, the increased ceramide level in CFTR-deficient cells likely mediates the upregulation of
proinflammatory cytokines by stimulating NF-κB.
Analysis of cell death in the lungs revealed a higher cell death rate of bronchial epithelial cells
in CFTR-deficient mice compared to wild type mice. This enhanced cell death rate in the bronchial
lumen results in formation of DNA-containing plugs and deposits the lungs. These DNA-containing
cell remnants are very viscous and may decrease mucociliary clearance. Normalization of ceramide
levels by pharmacological or genetic inhibition of acid SMase normalized the death rate of bronchial
epithelial cells in CFTR-deficient mice. DNA deposits may not only decrease mucociliary clearance but
also enhance P. aeruginosa adherence and infection in the lungs (Teichgraber et al., 2008). Clustering
of the CD95 receptor, which is crucial for induction of apoptosis, in ceramide-enriched platforms
(Grassme et al., 2001) may possibly be a link between enhanced ceramide and cell death triggering in
CFTR-deficient cells. However, the true mechanism by which enhanced ceramide levels trigger
apoptosis remains to be elucidated.
In summary, these results identify ceramide as one of the key regulators of inflammation and
subsequent infection in cystic fibrosis airway
Acid sphingomyelinase inhibitors in CF
Normalization of ceramide levels by amitriptyline may represent a new and important strategy to
prevent the onset of lung symptoms and reduce an existing pulmonary infection in individuals with
CF (Teichgraber et al., 2008). However, previous studies using mice that completely lack acid SMase
showed that these mice are unable to clear bacteria from airways by internalization via epithelial cell
ceramide-dependent rafts and to induce cellular apoptosis and thus fail to control bacterial infection
12
(Grassme et al., 2003). It is therefore important that any future cystic fibrosis drug targeting the acid
SMase is carefully titrated to normalize ceramide levels in the lungs of CF patients, but not reduce
ceramide concentrations below a critical cellular level that would impair the biological functions of
ceramide (Teichgraber et al., 2008).
The genetic or systemic inhibition of the acid sphingomyelinase (Asm) is not feasible for
treatment of patients or might cause adverse effects. Therefore, Becker et al. investigated the
manipulation of ceramide specifically in lungs of CF mice. They studied the reduction of acid SMase
activity and ceramide accumulation in lungs of CF mice by inhalation of different acid SMase
inhibitors (K. A. Becker et al., 2009). The drugs inhibit acid SMase by the following mechanism:
binding of acid SMase to lysosomes and secretory lysosomes protects the enzyme from proteolytic
inactivation. Weak bases such as amitriptyline accumulate within the acidic lysosomes and displace
acid SMase from the membrane by membrane binding that results in proteolytic degradation of the
enzyme (K. A. Becker et al., 2010). Inhalation of the acid SMase inhibitors amitriptyline, trimipramine,
desipramine, chlorprothixene, fluoxetine, amlodipine, or sertraline restored normal ceramide
concentrations in bronchial epithelial cells of CF mice, reduced inflammation in the lung of CF mice
and prevented infection with P. aeruginosa. All drugs showed very similar efficacy and inhalation of
the drugs did neither cause systemic effects nor inhibit neutral SMase. These findings address that
inhaling an acid SMase inhibitor may be a beneficial treatment for CF, with minimal adverse systemic
effects (K. A. Becker et al., 2009).
A recent clinical study (Riethmuller et al., 2009) established that amitriptyline treatment may
improve lung function in patients with cystic fibrosis and that use of acid SMase inhibitors is safe in
CF patients. Low doses of amitriptyline that was given systemically significantly improved lung
function in three of four patients as determined by measuring the forced expiratory volume in the
first second (FEV1). Furthermore, several CF patients that were treated with amitriptyline for several
years showed a continuous increase in lung function. Finally, amitriptyline treatment normalized
body weight and reduced the number of upper respiratory infections (Riethmuller et al., 2009). So,
amitriptyline is a safe and effective drug for treating CF patients. However, larger clinical trials are
essential to establish the positive effects for these acid SMase inhibiting drugs in the treatment of CF
pathogenesis.
Decreased ceramide levels in CF
Remarkably, results of studies by Radzioch and associates (Guilbault et al., 2008; Saeed et al., 2008)
show a decrease of ceramide in the lungs of CFTR-deficient mice compared to control mice that is
inconsistent with the data of Teichgraber and colleagues (Teichgraber et al., 2008). They report
diminished ceramide levels in CF related organs, including lung, pancreas and ileum, of CFTRdeficient mice and CFTR heterozygote mice. The specific mechanisms for this ceramide decrease
were not discussed. However, analysis of plasma from eight CF patients expressing the ΔF508CFTR
mutation and two patients with another CF genotype also showed a decrease in the average mass of
total plasma ceramide and decrease of several ceramide sphingolipid species (C14:0, C20:1, C22:0,
C22:1, and C24:0 ceramides, and dihydroxy ceramide DHC16:0). Administration of fenretinide, a
synthetic vitamin A derivative, increased ceramide concentrations in CF related organs and was
associated with a significant increase to fight P. aeruginosa-induced infection in CFTR-knockout mice
(Guilbault et al., 2008).
A consecutive study characterized the protective effect of fenretinide on the early onset of
osteoporosis in CFTR-knockout mice. Reduced bone mineral density which results in osteopenia and
osteoporosis is the most recently described phenotype associated with CF (Saeed et al., 2008). They
analyzed the effect of fenretinide on bone composition and architecture and quantified plasma fatty
acids. Fenretinide treatment dramatically increased trabecular bone volume compared to controls
that was related to increased plasma concentrations of ceramide. Increased ceramide levels resulted
in down-regulation of phospholipid-bound arachidonic acid in CFTR-deficient mice. These results
13
strongly suggest that fenretinide can potentially to be used as a prophylaxis by preventing the early
onset of osteoporosis in CF (Saeed et al., 2008).
CFTR discrepancy
It is currently not clear what leads to these discrepant results of ceramide levels in CFTRknockout models, but possible causes are discussed (K. A. Becker et al., 2010; Teichgraber et al.,
2008; Worgall, 2009). Studies that showed decreased ceramide levels used mice that are completely
deficient for CFTR. As these mice lack CFTR in the intestine, they usually die after birth due to
intestinal obstruction and therefore require a special liquid diet such as Petamen. Teichgraber et al.
tested this diet and showed that Petamen treatment results in very high cellular cholesterol
concentrations (about 300% increase) that in turn results in reduced acid SMase activity and
pulmonary ceramide concentrations in the lungs of CFTR-deficient mice (Teichgraber et al., 2008).
These effects are consistent with previously published data that note the interference of cholesterol
with acid SMase activity (Bhuvaneswaran, Venkatesan, & Mitropoulos, 1985). So, it is possible that
the Petamen diet in stead of CFTR-deficiency underlies the observation of decreased ceramide levels
in CFTR-knockout mice.
Furthermore, the different studies used different methods to determine ceramide mass
and define ceramide differenty. Radzoich et al. used an antibody to detect ceramide that detects
both unsatured ceramides and dihydroceramide. In addition, they used fenretinide to normalize
ceramide levels, a drug which is known to inhibit the activity of dihydroceramide desaturase and
stimulate activity of dihydroceramide synthase. Therefore, it is likely that the methods used by
Radzoich and associates predominantly determine the concentration of dihydroceramide. On the
other hand, Teichgraber and colleagues used antibodies that do not detect dihydroceramide. They
use the term ceramide to exclusively refer to unsatured ceramides. They speculate that unsatured
ceramides and dihydroceramide are differentially regulated in CF and an increase in the end product
unsatured ceramide, would result in a compensatory decrease in the dihydroceramide concentration
(K. A. Becker et al., 2010; Guilbault et al., 2008; Teichgraber et al., 2008).
A recent in vitro study (Hamai et al., 2009) also addresses changes in sphingolipid metabolism
due to decreased or defective CFTR. They found increased sphingolipid synthesis in human lung
epithelial cells that express ΔF508CFTR or decreased CFTR levels resulting in a significantly increased
mass of sphinganine, sphingosine and sphyngomyelin. Sphinganine is a ceramide precursor during
the de novo sphingolipid synthesis. Sphingolipid synthesis and mass are increased by overexpression
of ΔF508CFTR in CFTR-/- cells and decreased by overexpression of CFTR, but not by another ABCtransporter, ABCA7. Furthermore, decreased expression of CFTR, in contrast to expression of
ΔF508CFTR, affected the composition of ceramide species. The mass of four saturated long chain
ceramide species was increased and the mass of C18 and unsaturated C18:1 ceramide was
decreased. A decreased CFTR expression was also associated with increased expression of the longchain base subunit 1 (LCB1) of serine-palmitoyl transferase, the rate limiting enzyme of de novo
sphingolipid synthesis, and increased sphingolipid synthesis (Hamai et al., 2009).
So, Hamai and colleagues show an increase in mass of several saturated ceramides and only
one unsaturated ceramide in vitro (Hamai et al., 2009), Teichgraber et al. detected increased
unsaturated ceramide species in vivo (Teichgraber et al., 2008) and Radzoich and associates
(Guilbault et al., 2009) likely determine predominantly the concentration of dihydroceramide in vivo
(Teichgraber et al., 2008). As these studies use different techniques to measure sphingolipid levels
and consequently refer to different spingolipid species, it is difficult to conclude how the sphingolipid
metabolism really differs in the lungs of CF patients compared to healthy persons. However, as
ceramide, ceramide 1-phosphate and spingosine 1-phosphate induce proinflammatory mediators
(Nixon, 2009) (Fig. 4), increased levels of these sphingolipids would agree with the enhanced
inflammation observed in CF (Fig. 6).
14
Although several studies address opposite conclusions about ceramide levels in CFTRdeficient mice, together they strongly suggest an important role for CFTR in sphingolipid metabolism
and for sphingolipids in the regulation of inflammatory parameters and the defense against lung
infection with P. aeruginosa. Normalization of ceramide levels represents an important strategy to
prevent bacterial infections in patients with cystic fibrosis.
Ceramide, CFTR and eicosanoids
Clinical studies reported an increase in the levels of eicosanoids in bronchoalveolar lavage fluid
(BALF), saliva and urine from CF patients (Konstan, Walenga, Hilliard, & Hilliard, 1993). This
overproduction might contribute to the exaggerated inflammation in CF lungs, since PGE2 induces
the expression of a number of cytokines, including IL-6 and IL-8 by epithelial cells and T-lymphocytes.
Medjane et al. investigated the role for the ΔF508 mutation of CFTR in the production of the
eicosanoid PGE2 and expression of PLA2 in human respiratory epithelial cell lines (Medjane, Raymond,
Wu, & Touqui, 2005). As mentioned previously, PLA2 catalyzes the hydrolysis of phospholipids that
leads to the production of free fatty acids such as arachidonic acid. In turn, the breakdown of
arachidonic acid is catalyzed by COX-2 (Fig. 5). They show that CFTR dysfunction leads to enhanced
PGE2 release that can be amplified by LPS. The enhanced PGE2 release observed in CF cells is due to
both increased expression of COX-2 and accumulation of free arachidonic acid (Medjane et al., 2005).
These results are in agreement with previous studies that note increased arachidonic acid levels in
plasma of cystic fibrosis patients (Roulet et al., 1997) as well as in CFTR regulated tissues from CFTR /- mice (Freedman et al., 1999).
These studies did not yet mention sphingolipids as a possible link between the deficiency in
CFTR and increased COX-2 expression, arachidonic acid levels and PGE2 release. Possibly, enhanced
ceramide levels in CFTR-deficient cells (Teichgraber et al., 2008) induces PLA2 and COX-2 that leads to
enhanced production of arachidonic acid and PGE2. The increased production of PGE2 could also
(partly) be caused by reduced expression of HPGD (converses PGE2 to 15-keto-PGE2) observed in
tissues of CFTR-deficient mice (Harmon et al., 2010). However, additional studies should be
performed to clarify the mechanisms that underlie overproduction of eicosanoids in CFTR-deficient
cells.
CFTR and sphingosine 1-phosphate
CFTR is member of the ATP binding cassette transporter family that regulates transport of
sphingosine 1-phosphate. Cells expressing wild type CFTR show significantly higher uptake of
sphingosine 1-phosphate than either cells expressing the ΔF508CFTR mutant or mock-transfected
cells. Besides sphingosine 1-phosphate, CFTR can function as specific, dose-dependent and cAMP
independent transporter of dihydrosphingosine 1-phosphate and lysophosphatidic acid (Boujaoude
et al., 2001). Differences in sphingosine 1-phosphate uptake or release due to defective CFTR might
contribute to altered inflammation in CF patients, as sphingosine 1-phosphate has been shown to
modulate inflammatory signaling in several ways (Fig. 4). However, Teichgraber and colleagues did
not detect a significant change in sphingosine 1-phosphate abundance in the lungs of CFTR-deficient
mice compared to wild type mice (Teichgraber et al., 2008). If changes in CFTR-mediated transport of
sphingosine 1-phosphate contribute to the pathophysiology in CF still needs to be established.
15
Conclusion
Thus, cystic fibrosis is a complex disease characterized by the presence of thick pulmonary mucus
and recurrent and eventually chronic lung infections. Many studies report that CFTR-deficient cells
show enhanced proinflammatory signaling and proinflammatory cytokine secretion, even in the
absence of any infection. CFTR deficiency not only affects anion transport, but also many intracellular
mechanisms, such as apoptosis, calcium homeostasis, GSH transport, ROS production and lipid
metabolism. Many studies found that these intrinsic cellular changes result in activation of
inflammatory signaling routes leading to enhanced inflammation in CF cells compared to normal
cells.
The most important alterations in lipid metabolism that may contribute to the proinflammatory state
in CF cells are a decreased function and expression of the nuclear receptor PPAR-γ and an altered
sphingolipid metabolism, in particular altered ceramide levels (summarized in figure 6). The CFTRdependent defect in PPAR-γ function may either result from decreased PPAR-γ ligands, including 15keto-PGE2 and DHA, or from PPAR-γ sequestration by TG2. The decreased 15-keto-PGE2 level in CFTRdeficient cells likely results from decreased levels of HPGD, the enzyme that converts PGE2 to 15keto-PGE2. However, the specific molecular mechanisms and signaling events that connect CFTR
defects with decreased PPAR-γ function still need to be defined.
Two in vivo studies address opposite conclusions about ceramide levels in murine CF cells. While
Teichgraber and colleagues found excessive ceramide accumulation in respiratory tract epithelium of
CFTR-deficient mice, Radzoich and associates note diminished ceramide levels in CF related organs of
CF mice. Ceramide accumulation was attributed to a disturbed balance of pH-sensitive acid SMase
and ceramidase present in lysosomes. However, as ceramide activates production of
proinflammatory mediators, rather increased ceramide levels observed by Teichgraber and
colleagues than decreased ceramide levels observed by Radzoich et al. correspond with enhanced
inflammation observed in CF. Ceramide accumulation in CF cells could also explain enhanced
production of arachidonic acid and PGE2 via induction of PLA2 and COX-2 (Fig. 6).
Activation of PPAR-γ by PPAR-γ ligands resolve abnormal lung symptoms in a murine model. Besides,
normalization of ceramide levels in mice by either treatment with acid SMase inhibitors or
fenretinide has beneficial effects on CF pathogenesis. These findings indicate that drugs that
normalize altered lipid metabolism are promising for treating the pathofysiological lung symptoms in
CF patients.
16
Figure 6. CFTR-associated lipid
metabolism in a normal and
CFTR-defective cell. The most
important alterations in lipid
metabolism that contribute to
the proinflammatory state in CF
cells are a decreased function and
expression of the nuclear
receptor
PPAR-γ
and
accumulation of ceramide. This
leads
to
altered
gene
transcription
resulting
in
proinflammation and production
of high viscous mucus.
17
References
Alemany, R., van Koppen, C. J., Danneberg, K., Ter Braak, M., & Meyer Zu Heringdorf, D. (2007). Regulation and functional
roles of sphingosine kinases. Naunyn-Schmiedeberg's Archives of Pharmacology, 374(5-6), 413-428.
doi:10.1007/s00210-007-0132-3
Andersson, C., Zaman, M. M., Jones, A. B., & Freedman, S. D. (2008a). Alterations in immune response and PPAR/LXR
regulation in cystic fibrosis macrophages. Journal of Cystic Fibrosis : Official Journal of the European Cystic Fibrosis
Society, 7(1), 68-78. doi:10.1016/j.jcf.2007.05.004
Andersson, C., Zaman, M. M., Jones, A. B., & Freedman, S. D. (2008b). Alterations in immune response and PPAR/LXR
regulation in cystic fibrosis macrophages. Journal of Cystic Fibrosis : Official Journal of the European Cystic Fibrosis
Society, 7(1), 68-78. doi:10.1016/j.jcf.2007.05.004
Antigny, F., Norez, C., Becq, F., & Vandebrouck, C. (2008). Calcium homeostasis is abnormal in cystic fibrosis airway
epithelial cells but is normalized after rescue of F508del-CFTR. Cell Calcium, 43(2), 175-183.
doi:10.1016/j.ceca.2007.05.002
Bajmoczi, M., Gadjeva, M., Alper, S. L., Pier, G. B., & Golan, D. E. (2009). Cystic fibrosis transmembrane conductance
regulator and caveolin-1 regulate epithelial cell internalization of pseudomonas aeruginosa. American Journal of
Physiology.Cell Physiology, 297(2), C263-77. doi:10.1152/ajpcell.00527.2008
Bao, J. X., Jin, S., Zhang, F., Wang, Z. C., Li, N., & Li, P. L. (2010). Activation of membrane NADPH oxidase associated with
lysosome-targeted acid sphingomyelinase in coronary endothelial cells. Antioxidants & Redox Signaling, 12(6), 703712. doi:10.1089/ars.2009.2461
Bartoszewski, R., Rab, A., Jurkuvenaite, A., Mazur, M., Wakefield, J., Collawn, J. F., et al. (2008). Activation of the unfolded
protein response by deltaF508 CFTR. American Journal of Respiratory Cell and Molecular Biology, 39(4), 448-457.
doi:10.1165/rcmb.2008-0065OC
Bartoszewski, R., Rab, A., Twitty, G., Stevenson, L., Fortenberry, J., Piotrowski, A., et al. (2008). The mechanism of cystic
fibrosis transmembrane conductance regulator transcriptional repression during the unfolded protein response. The
Journal of Biological Chemistry, 283(18), 12154-12165. doi:10.1074/jbc.M707610200
Batal, I., Ericsoussi, M. B., Cluette-Brown, J. E., O'Sullivan, B. P., Freedman, S. D., Savaille, J. E., et al. (2007). Potential utility
of plasma fatty acid analysis in the diagnosis of cystic fibrosis. Clinical Chemistry, 53(1), 78-84.
doi:10.1373/clinchem.2006.077008
Becker, K. A., Grassme, H., Zhang, Y., & Gulbins, E. (2010). Ceramide in pseudomonas aeruginosa infections and cystic
fibrosis. Cellular Physiology and Biochemistry : International Journal of Experimental Cellular Physiology, Biochemistry,
and Pharmacology, 26(1), 57-66. doi:10.1159/000315106
Becker, K. A., Riethmuller, J., Luth, A., Doring, G., Kleuser, B., & Gulbins, E. (2009). Acid sphingomyelinase inhibitors
normalize pulmonary ceramide and inflammation in cystic fibrosis. American Journal of Respiratory Cell and Molecular
Biology, doi:10.1165/rcmb.2009-0174OC
Becker, M. N., Sauer, M. S., Muhlebach, M. S., Hirsh, A. J., Wu, Q., Verghese, M. W., et al. (2004). Cytokine secretion by
cystic fibrosis airway epithelial cells. American Journal of Respiratory and Critical Care Medicine, 169(5), 645-653.
doi:10.1164/rccm.200207-765OC
Berger, J., & Moller, D. E. (2002). The mechanisms of action of PPARs. Annual Review of Medicine, 53, 409-435.
doi:10.1146/annurev.med.53.082901.104018
Bergoin, C., Gosset, P., Lamblin, C., Bolard, F., Turck, D., Tonnel, A. B., et al. (2002). Cell and cytokine profile in nasal
secretions in cystic fibrosis. Journal of Cystic Fibrosis : Official Journal of the European Cystic Fibrosis Society, 1(3), 110115.
18
Bhuvaneswaran, C., Venkatesan, S., & Mitropoulos, K. A. (1985). Lysosomal accumulation of cholesterol and sphingomyelin:
Evidence for inhibition of acid sphingomyelinase. European Journal of Cell Biology, 37, 98-106.
Blanco, P. G., Zaman, M. M., Junaidi, O., Sheth, S., Yantiss, R. K., Nasser, I. A., et al. (2004). Induction of colitis in cftr-/- mice
results in bile duct injury. American Journal of Physiology.Gastrointestinal and Liver Physiology, 287(2), G491-6.
doi:10.1152/ajpgi.00452.2003
Bodas, M., & Vij, N. (2010). The NF-kappaB signaling in cystic fibrosis lung disease: Pathophysiology and therapeutic
potential. Discovery Medicine, 9(47), 346-356.
Bonfield, T. L., Konstan, M. W., & Berger, M. (1999). Altered respiratory epithelial cell cytokine production in cystic fibrosis.
The Journal of Allergy and Clinical Immunology, 104(1), 72-78.
Bonfield, T. L., Konstan, M. W., Burfeind, P., Panuska, J. R., Hilliard, J. B., & Berger, M. (1995). Normal bronchial epithelial
cells constitutively produce the anti-inflammatory cytokine interleukin-10, which is downregulated in cystic fibrosis.
American Journal of Respiratory Cell and Molecular Biology, 13(3), 257-261.
Boucher, R. C. (2007). Evidence for airway surface dehydration as the initiating event in CF airway disease. Journal of
Internal Medicine, 261(1), 5-16. doi:10.1111/j.1365-2796.2006.01744.x
Boujaoude, L. C., Bradshaw-Wilder, C., Mao, C., Cohn, J., Ogretmen, B., Hannun, Y. A., et al. (2001). Cystic fibrosis
transmembrane regulator regulates uptake of sphingoid base phosphates and lysophosphatidic acid: Modulation of
cellular activity of sphingosine 1-phosphate. The Journal of Biological Chemistry, 276(38), 35258-35264.
doi:10.1074/jbc.M105442200
Brown, R. K., McBurney, A., Lunec, J., & Kelly, F. J. (1995). Oxidative damage to DNA in patients with cystic fibrosis. Free
Radical Biology & Medicine, 18(4), 801-806.
Brown, R. K., Wyatt, H., Price, J. F., & Kelly, F. J. (1996). Pulmonary dysfunction in cystic fibrosis is associated with oxidative
stress. The European Respiratory Journal : Official Journal of the European Society for Clinical Respiratory Physiology,
9(2), 334-339.
Campodonico, V. L., Gadjeva, M., Paradis-Bleau, C., Uluer, A., & Pier, G. B. (2008). Airway epithelial control of pseudomonas
aeruginosa infection in cystic fibrosis. Trends in Molecular Medicine, 14(3), 120-133.
doi:10.1016/j.molmed.2008.01.002
Carrabino, S., Carpani, D., Livraghi, A., Di Cicco, M., Costantini, D., Copreni, E., et al. (2006). Dysregulated interleukin-8
secretion and NF-kappaB activity in human cystic fibrosis nasal epithelial cells. Journal of Cystic Fibrosis : Official
Journal of the European Cystic Fibrosis Society, 5(2), 113-119. doi:10.1016/j.jcf.2005.12.003
Christophe, A., Robberecht, E., De Baets, F., & Franckx, H. (1992). Increase of long chain omega-3 fatty acids in the major
serum lipid classes of patients with cystic fibrosis. Annals of Nutrition & Metabolism, 36(5-6), 304-312.
Collins, C. E., Quaggiotto, P., Wood, L., O'Loughlin, E. V., Henry, R. L., & Garg, M. L. (1999). Elevated plasma levels of F2
alpha isoprostane in cystic fibrosis. Lipids, 34(6), 551-556.
Com, G., & Clancy, J. P. (2009). Adenosine receptors, cystic fibrosis, and airway hydration. Handbook of Experimental
Pharmacology, (193)(193), 363-381. doi:10.1007/978-3-540-89615-9_12
Cremesti, A., Paris, F., Grassme, H., Holler, N., Tschopp, J., Fuks, Z., et al. (2001). Ceramide enables fas to cap and kill. The
Journal of Biological Chemistry, 276(26), 23954-23961. doi:10.1074/jbc.M101866200
Cuvillier, O., Pirianov, G., Kleuser, B., Vanek, P. G., Coso, O. A., Gutkind, S., et al. (1996). Suppression of ceramide-mediated
programmed cell death by sphingosine-1-phosphate. Nature, 381(6585), 800-803. doi:10.1038/381800a0
19
Dakin, C. J., Numa, A. H., Wang, H., Morton, J. R., Vertzyas, C. C., & Henry, R. L. (2002). Inflammation, infection, and
pulmonary function in infants and young children with cystic fibrosis. American Journal of Respiratory and Critical Care
Medicine, 165(7), 904-910.
Davis, P. B., Drumm, M., & Konstan, M. W. (1996). Cystic fibrosis. American Journal of Respiratory and Critical Care
Medicine, 154(5), 1229-1256.
Devchand, P. R., Keller, H., Peters, J. M., Vazquez, M., Gonzalez, F. J., & Wahli, W. (1996). The PPARalpha-leukotriene B4
pathway to inflammation control. Nature, 384(6604), 39-43. doi:10.1038/384039a0
Di, A., Brown, M. E., Deriy, L. V., Li, C., Szeto, F. L., Chen, Y., et al. (2006). CFTR regulates phagosome acidification in
macrophages and alters bactericidal activity. Nature Cell Biology, 8(9), 933-944. doi:10.1038/ncb1456
Dreyer, C., Krey, G., Keller, H., Givel, F., Helftenbein, G., & Wahli, W. (1992). Control of the peroxisomal beta-oxidation
pathway by a novel family of nuclear hormone receptors. Cell, 68(5), 879-887.
Dubin, P. J., McAllister, F., & Kolls, J. K. (2007). Is cystic fibrosis a TH17 disease? Inflammation Research : Official Journal of
the European Histamine Research Society ...[Et Al.], 56(6), 221-227. doi:10.1007/s00011-007-6187-2
Dumitru, C. A., & Gulbins, E. (2006). TRAIL activates acid sphingomyelinase via a redox mechanism and releases ceramide to
trigger apoptosis. Oncogene, 25(41), 5612-5625. doi:10.1038/sj.onc.1209568
Emerson, J., Rosenfeld, M., McNamara, S., Ramsey, B., & Gibson, R. L. (2002). Pseudomonas aeruginosa and other
predictors of mortality and morbidity in young children with cystic fibrosis. Pediatric Pulmonology, 34(2), 91-100.
doi:10.1002/ppul.10127
Engelhardt, J. F., Yankaskas, J. R., Ernst, S. A., Yang, Y., Marino, C. R., Boucher, R. C., et al. (1992a). Submucosal glands are
the predominant site of CFTR expression in the human bronchus. Nature Genetics, 2(3), 240-248. doi:10.1038/ng1192240
Engelhardt, J. F., Yankaskas, J. R., Ernst, S. A., Yang, Y., Marino, C. R., Boucher, R. C., et al. (1992b). Submucosal glands are
the predominant site of CFTR expression in the human bronchus. Nature Genetics, 2(3), 240-248. doi:10.1038/ng1192240
Freedman, S. D., Katz, M. H., Parker, E. M., Laposata, M., Urman, M. Y., & Alvarez, J. G. (1999). A membrane lipid imbalance
plays a role in the phenotypic expression of cystic fibrosis in cftr(-/-) mice. Proceedings of the National Academy of
Sciences of the United States of America, 96(24), 13995-14000.
Gao, L., Kim, K. J., Yankaskas, J. R., & Forman, H. J. (1999). Abnormal glutathione transport in cystic fibrosis airway epithelia.
The American Journal of Physiology, 277(1 Pt 1), L113-8.
Garcia, M. A., Yang, N., & Quinton, P. M. (2009). Normal mouse intestinal mucus release requires cystic fibrosis
transmembrane regulator-dependent bicarbonate secretion. The Journal of Clinical Investigation, 119(9), 2613-2622.
doi:10.1172/JCI38662
Genestra, M. (2007). Oxyl radicals, redox-sensitive signalling cascades and antioxidants. Cellular Signalling, 19(9), 18071819. doi:10.1016/j.cellsig.2007.04.009
Gilbert, A., Jadot, M., Leontieva, E., Wattiaux-De Coninck, S., & Wattiaux, R. (1998). Delta F508 CFTR localizes in the
endoplasmic reticulum-golgi intermediate compartment in cystic fibrosis cells. Experimental Cell Research, 242(1),
144-152. doi:10.1006/excr.1998.4101
Goggel, R., Winoto-Morbach, S., Vielhaber, G., Imai, Y., Lindner, K., Brade, L., et al. (2004). PAF-mediated pulmonary edema:
A new role for acid sphingomyelinase and ceramide. Nature Medicine, 10(2), 155-160. doi:10.1038/nm977
Goldman, M. J., Anderson, G. M., Stolzenberg, E. D., Kari, U. P., Zasloff, M., & Wilson, J. M. (1997). Human beta-defensin-1 is
a salt-sensitive antibiotic in lung that is inactivated in cystic fibrosis. Cell, 88(4), 553-560.
20
Grassme, H., Jekle, A., Riehle, A., Schwarz, H., Berger, J., Sandhoff, K., et al. (2001). CD95 signaling via ceramide-rich
membrane rafts. The Journal of Biological Chemistry, 276(23), 20589-20596. doi:10.1074/jbc.M101207200
Grassme, H., Jendrossek, V., Bock, J., Riehle, A., & Gulbins, E. (2002). Ceramide-rich membrane rafts mediate CD40
clustering. Journal of Immunology (Baltimore, Md.: 1950), 168(1), 298-307.
Grassme, H., Jendrossek, V., Riehle, A., von Kurthy, G., Berger, J., Schwarz, H., et al. (2003). Host defense against
pseudomonas aeruginosa requires ceramide-rich membrane rafts. Nature Medicine, 9(3), 322-330.
doi:10.1038/nm823
Grassme, H., Kirschnek, S., Riethmueller, J., Riehle, A., von Kurthy, G., Lang, F., et al. (2000). CD95/CD95 ligand interactions
on epithelial cells in host defense to pseudomonas aeruginosa. Science (New York, N.Y.), 290(5491), 527-530.
Guggino, W. B. (1999). Cystic fibrosis and the salt controversy. Cell, 96(5), 607-610.
Guilbault, C., De Sanctis, J. B., Wojewodka, G., Saeed, Z., Lachance, C., Skinner, T. A., et al. (2008). Fenretinide corrects
newly found ceramide deficiency in cystic fibrosis. American Journal of Respiratory Cell and Molecular Biology, 38(1),
47-56. doi:10.1165/rcmb.2007-0036OC
Guilbault, C., Wojewodka, G., Saeed, Z., Hajduch, M., Matouk, E., De Sanctis, J. B., et al. (2009). Cystic fibrosis fatty acid
imbalance is linked to ceramide deficiency and corrected by fenretinide. American Journal of Respiratory Cell and
Molecular Biology, 41(1), 100-106. doi:10.1165/rcmb.2008-0279OC
Gulbins, E. (2010). Lipids control mucus production in cystic fibrosis. Nature Medicine, 16(3), 267-268. doi:10.1038/nm0310267
Haddad, J. J. (2002). Redox regulation of pro-inflammatory cytokines and IkappaB-alpha/NF-kappaB nuclear translocation
and activation. Biochemical and Biophysical Research Communications, 296(4), 847-856.
Hamai, H., Keyserman, F., Quittell, L. M., & Worgall, T. S. (2009). Defective CFTR increases synthesis and mass of
sphingolipids that modulate membrane composition and lipid signaling. Journal of Lipid Research, 50(6), 1101-1108.
doi:10.1194/jlr.M800427-JLR200
Hampton, T. H., & Stanton, B. A. (2010). A novel approach to analyze gene expression data demonstrates that the
DeltaF508 mutation in CFTR downregulates the antigen presentation pathway. American Journal of Physiology.Lung
Cellular and Molecular Physiology, 298(4), L473-82. doi:10.1152/ajplung.00379.2009
Hannun, Y. A., & Obeid, L. M. (2008). Principles of bioactive lipid signalling: Lessons from sphingolipids. Nature
Reviews.Molecular Cell Biology, 9(2), 139-150. doi:10.1038/nrm2329
Hara-Chikuma, M., Yang, B., Sonawane, N. D., Sasaki, S., Uchida, S., & Verkman, A. S. (2005). ClC-3 chloride channels
facilitate endosomal acidification and chloride accumulation. The Journal of Biological Chemistry, 280(2), 1241-1247.
doi:10.1074/jbc.M407030200
Harmon, G. S., Dumlao, D. S., Ng, D. T., Barrett, K. E., Dennis, E. A., Dong, H., et al. (2010). Pharmacological correction of a
defect in PPAR-gamma signaling ameliorates disease severity in cftr-deficient mice. Nature Medicine, 16(3), 313-318.
doi:10.1038/nm.2101
Herz, J., Pardo, J., Kashkar, H., Schramm, M., Kuzmenkina, E., Bos, E., et al. (2009). Acid sphingomyelinase is a key regulator
of cytotoxic granule secretion by primary T lymphocytes. Nature Immunology, 10(7), 761-768. doi:10.1038/ni.1757
Hybiske, K., Fu, Z., Schwarzer, C., Tseng, J., Do, J., Huang, N., et al. (2007). Effects of cystic fibrosis transmembrane
conductance regulator and DeltaF508CFTR on inflammatory response, ER stress, and Ca2+ of airway epithelia.
American Journal of Physiology.Lung Cellular and Molecular Physiology, 293(5), L1250-60.
doi:10.1152/ajplung.00231.2007
21
Jiang, C., Ting, A. T., & Seed, B. (1998). PPAR-gamma agonists inhibit production of monocyte inflammatory cytokines.
Nature, 391(6662), 82-86. doi:10.1038/34184
Joseph, T., Look, D., & Ferkol, T. (2005). NF-kappaB activation and sustained IL-8 gene expression in primary cultures of
cystic fibrosis airway epithelial cells stimulated with pseudomonas aeruginosa. American Journal of Physiology.Lung
Cellular and Molecular Physiology, 288(3), L471-9. doi:10.1152/ajplung.00066.2004
Jungas, T., Motta, I., Duffieux, F., Fanen, P., Stoven, V., & Ojcius, D. M. (2002). Glutathione levels and BAX activation during
apoptosis due to oxidative stress in cells expressing wild-type and mutant cystic fibrosis transmembrane conductance
regulator. The Journal of Biological Chemistry, 277(31), 27912-27918. doi:10.1074/jbc.M110288200
Kerbiriou, M., Le Drevo, M. A., Ferec, C., & Trouve, P. (2007). Coupling cystic fibrosis to endoplasmic reticulum stress:
Differential role of Grp78 and ATF6. Biochimica Et Biophysica Acta, 1772(11-12), 1236-1249.
doi:10.1016/j.bbadis.2007.10.004
Kerem, B., Rommens, J. M., Buchanan, J. A., Markiewicz, D., Cox, T. K., Chakravarti, A., et al. (1989). Identification of the
cystic fibrosis gene: Genetic analysis. Science (New York, N.Y.), 245(4922), 1073-1080.
Kerem, E., Bistritzer, T., Hanukoglu, A., Hofmann, T., Zhou, Z., Bennett, W., et al. (1999). Pulmonary epithelial sodiumchannel dysfunction and excess airway liquid in pseudohypoaldosteronism. The New England Journal of Medicine,
341(3), 156-162.
Khan, T. Z., Wagener, J. S., Bost, T., Martinez, J., Accurso, F. J., & Riches, D. W. (1995). Early pulmonary inflammation in
infants with cystic fibrosis. American Journal of Respiratory and Critical Care Medicine, 151(4), 1075-1082.
Knorre, A., Wagner, M., Schaefer, H. E., Colledge, W. H., & Pahl, H. L. (2002). DeltaF508-CFTR causes constitutive NF-kappaB
activation through an ER-overload response in cystic fibrosis lungs. Biological Chemistry, 383(2), 271-282.
doi:10.1515/BC.2002.029
Konstan, M. W., Walenga, R. W., Hilliard, K. A., & Hilliard, J. B. (1993). Leukotriene B4 markedly elevated in the epithelial
lining fluid of patients with cystic fibrosis. The American Review of Respiratory Disease, 148(4 Pt 1), 896-901.
Kowalski, M. P., & Pier, G. B. (2004). Localization of cystic fibrosis transmembrane conductance regulator to lipid rafts of
epithelial cells is required for pseudomonas aeruginosa-induced cellular activation. Journal of Immunology (Baltimore,
Md.: 1950), 172(1), 418-425.
Kumar, V., Becker, T., Jansen, S., van Barneveld, A., Boztug, K., Wolfl, S., et al. (2008). Expression levels of FAS are regulated
through an evolutionary conserved element in intron 2, which modulates cystic fibrosis disease severity. Genes and
Immunity, 9(8), 689-696. doi:10.1038/gene.2008.63
KUO, P. T., HUANG, N. N., & BASSETT, D. R. (1962). The fatty acid composition of the serum chylomicrons and adipose tissue
of children with cystic fibrosis of the pancreas. The Journal of Pediatrics, 60, 394-403.
Lahiri, S., & Futerman, A. H. (2007). The metabolism and function of sphingolipids and glycosphingolipids. Cellular and
Molecular Life Sciences : CMLS, 64(17), 2270-2284. doi:10.1007/s00018-007-7076-0
Lai, E., Teodoro, T., & Volchuk, A. (2007). Endoplasmic reticulum stress: Signaling the unfolded protein response. Physiology
(Bethesda, Md.), 22, 193-201. doi:10.1152/physiol.00050.2006
Lehrer, R. I., & Ganz, T. (2002). Defensins of vertebrate animals. Current Opinion in Immunology, 14(1), 96-102.
Levison, H., Mindorff, C. M., Chao, J., Turner, J. A., Sturgess, J. M., & Stringer, D. A. (1983). Pathophysiology of the ciliary
motility syndromes. European Journal of Respiratory Diseases.Supplement, 127, 102-117.
Lewis, J. D., Lichtenstein, G. R., Stein, R. B., Deren, J. J., Judge, T. A., Fogt, F., et al. (2001). An open-label trial of the PPARgamma ligand rosiglitazone for active ulcerative colitis. The American Journal of Gastroenterology, 96(12), 3323-3328.
doi:10.1111/j.1572-0241.2001.05333.x
22
Li, Z., Kosorok, M. R., Farrell, P. M., Laxova, A., West, S. E., Green, C. G., et al. (2005). Longitudinal development of mucoid
pseudomonas aeruginosa infection and lung disease progression in children with cystic fibrosis. JAMA : The Journal of
the American Medical Association, 293(5), 581-588. doi:10.1001/jama.293.5.581
Linsdell, P., Evagelidis, A., & Hanrahan, J. W. (2000). Molecular determinants of anion selectivity in the cystic fibrosis
transmembrane conductance regulator chloride channel pore. Biophysical Journal, 78(6), 2973-2982.
doi:10.1016/S0006-3495(00)76836-6
Maiuri, L., Luciani, A., Giardino, I., Raia, V., Villella, V. R., D'Apolito, M., et al. (2008). Tissue transglutaminase activation
modulates inflammation in cystic fibrosis via PPARgamma down-regulation. Journal of Immunology (Baltimore, Md.:
1950), 180(11), 7697-7705.
Manthey, C. L., & Schuchman, E. H. (1998). Acid sphingomyelinase-derived ceramide is not required for inflammatory
cytokine signalling in murine macrophages. Cytokine, 10(9), 654-661. doi:10.1006/cyto.1998.0344
Matsui, H., Grubb, B. R., Tarran, R., Randell, S. H., Gatzy, J. T., Davis, C. W., et al. (1998). Evidence for periciliary liquid layer
depletion, not abnormal ion composition, in the pathogenesis of cystic fibrosis airways disease. Cell, 95(7), 1005-1015.
Matsui, H., Verghese, M. W., Kesimer, M., Schwab, U. E., Randell, S. H., Sheehan, J. K., et al. (2005). Reduced threedimensional motility in dehydrated airway mucus prevents neutrophil capture and killing bacteria on airway epithelial
surfaces. Journal of Immunology (Baltimore, Md.: 1950), 175(2), 1090-1099.
Medjane, S., Raymond, B., Wu, Y., & Touqui, L. (2005). Impact of CFTR DeltaF508 mutation on prostaglandin E2 production
and type IIA phospholipase A2 expression by pulmonary epithelial cells. American Journal of Physiology.Lung Cellular
and Molecular Physiology, 289(5), L816-24. doi:10.1152/ajplung.00466.2004
Meusser, B., Hirsch, C., Jarosch, E., & Sommer, T. (2005). ERAD: The long road to destruction. Nature Cell Biology, 7(8), 766772. doi:10.1038/ncb0805-766
Muhlebach, M. S., Stewart, P. W., Leigh, M. W., & Noah, T. L. (1999). Quantitation of inflammatory responses to bacteria in
young cystic fibrosis and control patients. American Journal of Respiratory and Critical Care Medicine, 160(1), 186-191.
Nagy, L., Tontonoz, P., Alvarez, J. G., Chen, H., & Evans, R. M. (1998). Oxidized LDL regulates macrophage gene expression
through ligand activation of PPARgamma. Cell, 93(2), 229-240.
Nichols, D. P., Konstan, M. W., & Chmiel, J. F. (2008). Anti-inflammatory therapies for cystic fibrosis-related lung disease.
Clinical Reviews in Allergy & Immunology, 35(3), 135-153. doi:10.1007/s12016-008-8081-2
Nixon, G. F. (2009). Sphingolipids in inflammation: Pathological implications and potential therapeutic targets. British
Journal of Pharmacology, 158(4), 982-993. doi:10.1111/j.1476-5381.2009.00281.x
Ollero, M., Junaidi, O., Zaman, M. M., Tzameli, I., Ferrando, A. A., Andersson, C., et al. (2004). Decreased expression of
peroxisome proliferator activated receptor gamma in cftr-/- mice. Journal of Cellular Physiology, 200(2), 235-244.
doi:10.1002/jcp.20020
Osika, E., Cavaillon, J. M., Chadelat, K., Boule, M., Fitting, C., Tournier, G., et al. (1999). Distinct sputum cytokine profiles in
cystic fibrosis and other chronic inflammatory airway disease. The European Respiratory Journal : Official Journal of the
European Society for Clinical Respiratory Physiology, 14(2), 339-346.
Painter, R. G., Bonvillain, R. W., Valentine, V. G., Lombard, G. A., LaPlace, S. G., Nauseef, W. M., et al. (2008). The role of
chloride anion and CFTR in killing of pseudomonas aeruginosa by normal and CF neutrophils. Journal of Leukocyte
Biology, 83(6), 1345-1353. doi:10.1189/jlb.0907658
Perez, A., Issler, A. C., Cotton, C. U., Kelley, T. J., Verkman, A. S., & Davis, P. B. (2007). CFTR inhibition mimics the cystic
fibrosis inflammatory profile. American Journal of Physiology.Lung Cellular and Molecular Physiology, 292(2), L383-95.
doi:10.1152/ajplung.00403.2005
23
Perez, A., van Heeckeren, A. M., Nichols, D., Gupta, S., Eastman, J. F., & Davis, P. B. (2008). Peroxisome proliferatoractivated receptor-gamma in cystic fibrosis lung epithelium. American Journal of Physiology.Lung Cellular and
Molecular Physiology, 295(2), L303-13. doi:10.1152/ajplung.90276.2008
Pettus, B. J., Chalfant, C. E., & Hannun, Y. A. (2004). Sphingolipids in inflammation: Roles and implications. Current
Molecular Medicine, 4(4), 405-418.
Poli, V. (1998). The role of C/EBP isoforms in the control of inflammatory and native immunity functions. The Journal of
Biological Chemistry, 273(45), 29279-29282.
Quinton, P. M. (2008). Cystic fibrosis: Impaired bicarbonate secretion and mucoviscidosis. Lancet, 372(9636), 415-417.
doi:10.1016/S0140-6736(08)61162-9
Rab, A., Bartoszewski, R., Jurkuvenaite, A., Wakefield, J., Collawn, J. F., & Bebok, Z. (2007). Endoplasmic reticulum stress and
the unfolded protein response regulate genomic cystic fibrosis transmembrane conductance regulator expression.
American Journal of Physiology.Cell Physiology, 292(2), C756-66. doi:10.1152/ajpcell.00391.2006
Rao, R. V., Ellerby, H. M., & Bredesen, D. E. (2004). Coupling endoplasmic reticulum stress to the cell death program. Cell
Death and Differentiation, 11(4), 372-380. doi:10.1038/sj.cdd.4401378
Ratjen, F., & Doring, G. (2003). Cystic fibrosis. Lancet, 361(9358), 681-689. doi:10.1016/S0140-6736(03)12567-6
Ribeiro, C. M., Paradiso, A. M., Carew, M. A., Shears, S. B., & Boucher, R. C. (2005). Cystic fibrosis airway epithelial Ca2+ i
signaling: The mechanism for the larger agonist-mediated Ca2+ i signals in human cystic fibrosis airway epithelia. The
Journal of Biological Chemistry, 280(11), 10202-10209. doi:10.1074/jbc.M410617200
Ribeiro, C. M., Paradiso, A. M., Schwab, U., Perez-Vilar, J., Jones, L., O'neal, W., et al. (2005). Chronic airway
infection/inflammation induces a Ca2+i-dependent hyperinflammatory response in human cystic fibrosis airway
epithelia. The Journal of Biological Chemistry, 280(18), 17798-17806. doi:10.1074/jbc.M410618200
Ricote, M., Li, A. C., Willson, T. M., Kelly, C. J., & Glass, C. K. (1998). The peroxisome proliferator-activated receptor-gamma
is a negative regulator of macrophage activation. Nature, 391(6662), 79-82. doi:10.1038/34178
Riethmuller, J., Anthonysamy, J., Serra, E., Schwab, M., Doring, G., & Gulbins, E. (2009). Therapeutic efficacy and safety of
amitriptyline in patients with cystic fibrosis. Cellular Physiology and Biochemistry : International Journal of
Experimental Cellular Physiology, Biochemistry, and Pharmacology, 24(1-2), 65-72. doi:10.1159/000227814
Riordan, J. R., Rommens, J. M., Kerem, B., Alon, N., Rozmahel, R., Grzelczak, Z., et al. (1989). Identification of the cystic
fibrosis gene: Cloning and characterization of complementary DNA. Science (New York, N.Y.), 245(4922), 1066-1073.
Roghanian, A., & Sallenave, J. M. (2008). Neutrophil elastase (NE) and NE inhibitors: Canonical and noncanonical functions
in lung chronic inflammatory diseases (cystic fibrosis and chronic obstructive pulmonary disease). Journal of Aerosol
Medicine and Pulmonary Drug Delivery, 21(1), 125-144. doi:10.1089/jamp.2007.0653
Rommens, J. M., Iannuzzi, M. C., Kerem, B., Drumm, M. L., Melmer, G., Dean, M., et al. (1989). Identification of the cystic
fibrosis gene: Chromosome walking and jumping. Science (New York, N.Y.), 245(4922), 1059-1065.
Rosenlund, M. L., Kim, H. K., & Kritchevsky, D. (1974). Essential fatty acids in cystic fibrosis. Nature, 251(5477), 719.
Rotolo, J. A., Zhang, J., Donepudi, M., Lee, H., Fuks, Z., & Kolesnick, R. (2005). Caspase-dependent and -independent
activation of acid sphingomyelinase signaling. The Journal of Biological Chemistry, 280(28), 26425-26434.
doi:10.1074/jbc.M414569200
Rottner, M., Freyssinet, J. M., & Martinez, M. C. (2009). Mechanisms of the noxious inflammatory cycle in cystic fibrosis.
Respiratory Research, 10, 23. doi:10.1186/1465-9921-10-23
24
Rottner, M., Kunzelmann, C., Mergey, M., Freyssinet, J. M., & Martinez, M. C. (2007). Exaggerated apoptosis and NF-kappaB
activation in pancreatic and tracheal cystic fibrosis cells. The FASEB Journal : Official Publication of the Federation of
American Societies for Experimental Biology, 21(11), 2939-2948. doi:10.1096/fj.06-7614com
Roulet, M., Frascarolo, P., Rappaz, I., & Pilet, M. (1997). Essential fatty acid deficiency in well nourished young cystic fibrosis
patients. European Journal of Pediatrics, 156(12), 952-956.
Roum, J. H., Buhl, R., McElvaney, N. G., Borok, Z., & Crystal, R. G. (1993a). Systemic deficiency of glutathione in cystic
fibrosis. Journal of Applied Physiology (Bethesda, Md.: 1985), 75(6), 2419-2424.
Roum, J. H., Buhl, R., McElvaney, N. G., Borok, Z., & Crystal, R. G. (1993b). Systemic deficiency of glutathione in cystic
fibrosis. Journal of Applied Physiology (Bethesda, Md.: 1985), 75(6), 2419-2424.
Saeed, Z., Guilbault, C., De Sanctis, J. B., Henri, J., Marion, D., St-Arnaud, R., et al. (2008). Fenretinide prevents the
development of osteoporosis in cftr-KO mice. Journal of Cystic Fibrosis : Official Journal of the European Cystic Fibrosis
Society, 7(3), 222-230. doi:10.1016/j.jcf.2007.09.001
Schroeder, T. H., Lee, M. M., Yacono, P. W., Cannon, C. L., Gerceker, A. A., Golan, D. E., et al. (2002). CFTR is a pattern
recognition molecule that extracts pseudomonas aeruginosa LPS from the outer membrane into epithelial cells and
activates NF-kappa B translocation. Proceedings of the National Academy of Sciences of the United States of America,
99(10), 6907-6912. doi:10.1073/pnas.092160899
Selsted, M. E., & Ouellette, A. J. (2005). Mammalian defensins in the antimicrobial immune response. Nature Immunology,
6(6), 551-557. doi:10.1038/ni1206
Smith, J. J., Travis, S. M., Greenberg, E. P., & Welsh, M. J. (1996). Cystic fibrosis airway epithelia fail to kill bacteria because
of abnormal airway surface fluid. Cell, 85(2), 229-236.
Su, C. G., Wen, X., Bailey, S. T., Jiang, W., Rangwala, S. M., Keilbaugh, S. A., et al. (1999). A novel therapy for colitis utilizing
PPAR-gamma ligands to inhibit the epithelial inflammatory response. The Journal of Clinical Investigation, 104(4), 383389. doi:10.1172/JCI7145
Tabary, O., Boncoeur, E., de Martin, R., Pepperkok, R., Clement, A., Schultz, C., et al. (2006). Calcium-dependent regulation
of NF-(kappa)B activation in cystic fibrosis airway epithelial cells. Cellular Signalling, 18(5), 652-660.
doi:10.1016/j.cellsig.2005.06.004
Tarran, R., Grubb, B. R., Parsons, D., Picher, M., Hirsh, A. J., Davis, C. W., et al. (2001). The CF salt controversy: In vivo
observations and therapeutic approaches. Molecular Cell, 8(1), 149-158.
Teichgraber, V., Ulrich, M., Endlich, N., Riethmuller, J., Wilker, B., De Oliveira-Munding, C. C., et al. (2008). Ceramide
accumulation mediates inflammation, cell death and infection susceptibility in cystic fibrosis. Nature Medicine, 14(4),
382-391. doi:10.1038/nm1748
Thomas, G. R., Costelloe, E. A., Lunn, D. P., Stacey, K. J., Delaney, S. J., Passey, R., et al. (2000). G551D cystic fibrosis mice
exhibit abnormal regulation of inflammation in lungs and macrophages. Journal of Immunology (Baltimore, Md.: 1950),
164(7), 3870-3877.
Tontonoz, P., & Spiegelman, B. M. (2008). Fat and beyond: The diverse biology of PPARgamma. Annual Review of
Biochemistry, 77, 289-312. doi:10.1146/annurev.biochem.77.061307.091829
Turnbull, E. L., Rosser, M. F., & Cyr, D. M. (2007). The role of the UPS in cystic fibrosis. BMC Biochemistry, 8 Suppl 1, S11.
doi:10.1186/1471-2091-8-S1-S11
Ulrich, M., Herbert, S., Berger, J., Bellon, G., Louis, D., Munker, G., et al. (1998). Localization of staphylococcus aureus in
infected airways of patients with cystic fibrosis and in a cell culture model of S. aureus adherence. American Journal of
Respiratory Cell and Molecular Biology, 19(1), 83-91.
25
Velsor, L. W., Kariya, C., Kachadourian, R., & Day, B. J. (2006). Mitochondrial oxidative stress in the lungs of cystic fibrosis
transmembrane conductance regulator protein mutant mice. American Journal of Respiratory Cell and Molecular
Biology, 35(5), 579-586. doi:10.1165/rcmb.2005-0473OC
Velsor, L. W., van Heeckeren, A., & Day, B. J. (2001). Antioxidant imbalance in the lungs of cystic fibrosis transmembrane
conductance regulator protein mutant mice. American Journal of Physiology.Lung Cellular and Molecular Physiology,
281(1), L31-8.
Verhaeghe, C., Remouchamps, C., Hennuy, B., Vanderplasschen, A., Chariot, A., Tabruyn, S. P., et al. (2007a). Role of IKK and
ERK pathways in intrinsic inflammation of cystic fibrosis airways. Biochemical Pharmacology, 73(12), 1982-1994.
doi:10.1016/j.bcp.2007.03.019
Verhaeghe, C., Remouchamps, C., Hennuy, B., Vanderplasschen, A., Chariot, A., Tabruyn, S. P., et al. (2007b). Role of IKK and
ERK pathways in intrinsic inflammation of cystic fibrosis airways. Biochemical Pharmacology, 73(12), 1982-1994.
doi:10.1016/j.bcp.2007.03.019
Verhaeghe, C., Remouchamps, C., Hennuy, B., Vanderplasschen, A., Chariot, A., Tabruyn, S. P., et al. (2007c). Role of IKK and
ERK pathways in intrinsic inflammation of cystic fibrosis airways. Biochemical Pharmacology, 73(12), 1982-1994.
doi:10.1016/j.bcp.2007.03.019
Verkman, A. S., Song, Y., & Thiagarajah, J. R. (2003). Role of airway surface liquid and submucosal glands in cystic fibrosis
lung disease. American Journal of Physiology.Cell Physiology, 284(1), C2-15. doi:10.1152/ajpcell.00417.2002
Vij, N., Mazur, S., & Zeitlin, P. L. (2009). CFTR is a negative regulator of NFkappaB mediated innate immune response. PloS
One, 4(2), e4664. doi:10.1371/journal.pone.0004664
Weber, A. J., Soong, G., Bryan, R., Saba, S., & Prince, A. (2001). Activation of NF-kappaB in airway epithelial cells is
dependent on CFTR trafficking and cl- channel function. American Journal of Physiology.Lung Cellular and Molecular
Physiology, 281(1), L71-8.
Worgall, T. S. (2009). Lipid metabolism in cystic fibrosis. Current Opinion in Clinical Nutrition and Metabolic Care, 12(2), 105109.
Worlitzsch, D., Tarran, R., Ulrich, M., Schwab, U., Cekici, A., Meyer, K. C., et al. (2002). Effects of reduced mucus oxygen
concentration in airway pseudomonas infections of cystic fibrosis patients. The Journal of Clinical Investigation, 109(3),
317-325. doi:10.1172/JCI13870
Xiao, C., & Ghosh, S. (2005). NF-kappaB, an evolutionarily conserved mediator of immune and inflammatory responses.
Advances in Experimental Medicine and Biology, 560, 41-45. doi:10.1007/0-387-24180-9_5
Yki-Jarvinen, H. (2004). Thiazolidinediones. The New England Journal of Medicine, 351(11), 1106-1118.
doi:10.1056/NEJMra041001
Yu, H., Zeidan, Y. H., Wu, B. X., Jenkins, R. W., Flotte, T. R., Hannun, Y. A., et al. (2009). Defective acid sphingomyelinase
pathway with pseudomonas aeruginosa infection in cystic fibrosis. American Journal of Respiratory Cell and Molecular
Biology, 41(3), 367-375. doi:10.1165/rcmb.2008-0295OC
Zabner, J., Smith, J. J., Karp, P. H., Widdicombe, J. H., & Welsh, M. J. (1998). Loss of CFTR chloride channels alters salt
absorption by cystic fibrosis airway epithelia in vitro. Molecular Cell, 2(3), 397-403.
Zhang, Y., Yao, B., Delikat, S., Bayoumy, S., Lin, X. H., Basu, S., et al. (1997). Kinase suppressor of ras is ceramide-activated
protein kinase. Cell, 89(1), 63-72.
26