A Haitian Boy`s Needless Death From Diabetes By PALAV BABARIA
advertisement
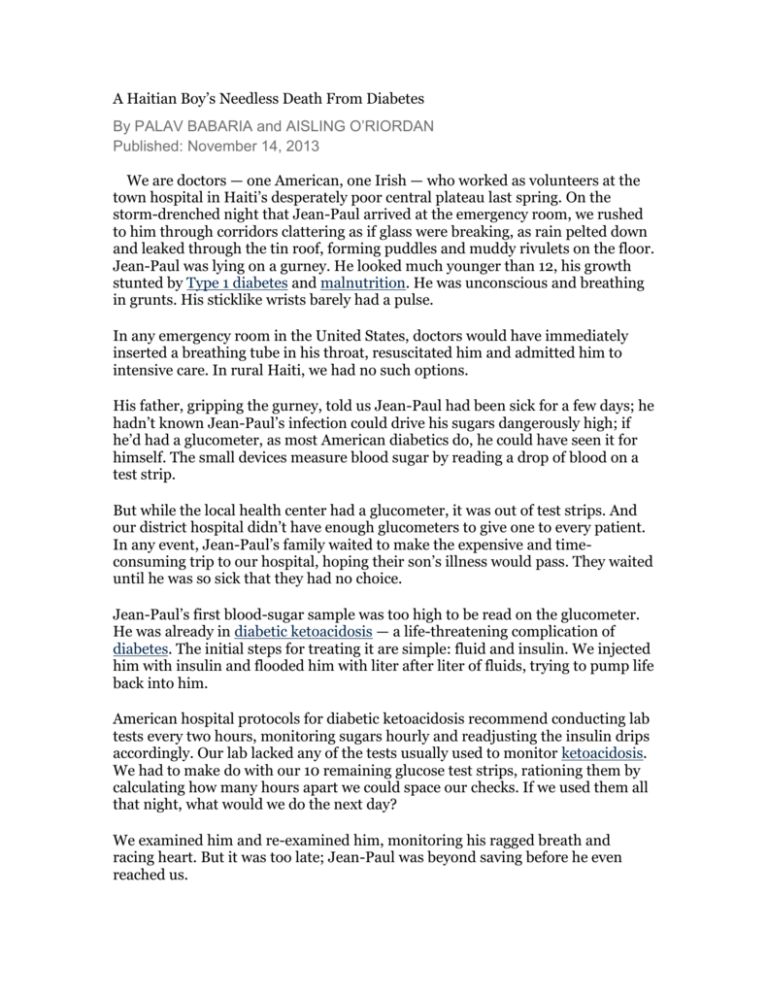
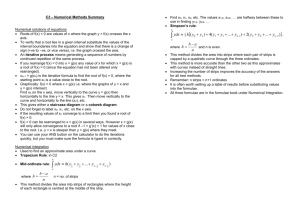
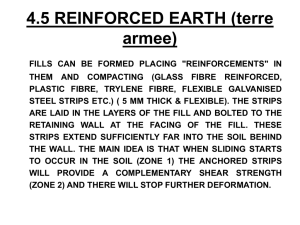
A Haitian Boy’s Needless Death From Diabetes By PALAV BABARIA and AISLING O’RIORDAN Published: November 14, 2013 We are doctors — one American, one Irish — who worked as volunteers at the town hospital in Haiti’s desperately poor central plateau last spring. On the storm-drenched night that Jean-Paul arrived at the emergency room, we rushed to him through corridors clattering as if glass were breaking, as rain pelted down and leaked through the tin roof, forming puddles and muddy rivulets on the floor. Jean-Paul was lying on a gurney. He looked much younger than 12, his growth stunted by Type 1 diabetes and malnutrition. He was unconscious and breathing in grunts. His sticklike wrists barely had a pulse. In any emergency room in the United States, doctors would have immediately inserted a breathing tube in his throat, resuscitated him and admitted him to intensive care. In rural Haiti, we had no such options. His father, gripping the gurney, told us Jean-Paul had been sick for a few days; he hadn’t known Jean-Paul’s infection could drive his sugars dangerously high; if he’d had a glucometer, as most American diabetics do, he could have seen it for himself. The small devices measure blood sugar by reading a drop of blood on a test strip. But while the local health center had a glucometer, it was out of test strips. And our district hospital didn’t have enough glucometers to give one to every patient. In any event, Jean-Paul’s family waited to make the expensive and timeconsuming trip to our hospital, hoping their son’s illness would pass. They waited until he was so sick that they had no choice. Jean-Paul’s first blood-sugar sample was too high to be read on the glucometer. He was already in diabetic ketoacidosis — a life-threatening complication of diabetes. The initial steps for treating it are simple: fluid and insulin. We injected him with insulin and flooded him with liter after liter of fluids, trying to pump life back into him. American hospital protocols for diabetic ketoacidosis recommend conducting lab tests every two hours, monitoring sugars hourly and readjusting the insulin drips accordingly. Our lab lacked any of the tests usually used to monitor ketoacidosis. We had to make do with our 10 remaining glucose test strips, rationing them by calculating how many hours apart we could space our checks. If we used them all that night, what would we do the next day? We examined him and re-examined him, monitoring his ragged breath and racing heart. But it was too late; Jean-Paul was beyond saving before he even reached us. Today is World Diabetes Day, and we cannot help but remember his needless loss. Every day in Haiti, we encountered the problem that killed him: Manufacturers of glucometers would give them away like free candy, and sometimes a half dozen would be scattered across the hospital. But they were useless because the test strips were always out of stock. Glucose test strips are a major source of the profit derived from diabetes testing supplies. Conglomerates like Roche, the leader of the $8 billion a year diabetes testing industry, have made these strips proprietary — in other words, each strip fits only into a specific machine. While glucose test strips cost pennies to make, the branded strips sell for 50 cents to one dollar per strip, and diabetics who depend on insulin typically use several strips per day. In Haiti, we would sometimes deplete an entire box of 50 glucose strips on a single sick patient who required frequent monitoring. This precious box was often ordered months in advance; it took up to six months for the order to go from the district to Port-au-Prince, Haiti’s capital, and on to the United States, and then for the shipment to arrive in Haiti, clear customs and be transported from a central depot to a peripheral one and finally to our hospital. When a box ran out, we rarely knew when the next would arrive. And by that time, manufacturers might have changed their models, and stopped manufacturing strips for the glucometers we had. For sites like ours, which rely on donated supplies, ensuring that glucometers and test strips are from the same model and manufacturer has been virtually impossible. That mismatch is often the missing lifeline for patients like JeanPaul. The solution is simple, and one that many diabetics have been urging for decades: Create universal test strips that will work in any available machine, in the same manner that USB cables can link nearly all brands of computers and devices. Universal test strips would lead to cheaper strips and increased availability. This would ensure that diabetic patients in places like rural Haiti could monitor their own blood sugars, and local clinics and hospitals could effectively screen for, diagnose and treat diabetes. Patients like Jean-Paul would know their sugars were too high because of an infection, and come in to the hospital before it was too late. Instead, we watched as nurses disconnected Jean-Paul from the intravenous tubing that night and carefully pulled a sheet over him so his father could carry his body out of the hospital. <img src="http://meter-svc.nytimes.com/meter.gif"/> Palav Babaria is a primary care doctor at Highland Hospital in Oakland, Calif. Aisling O’Riordan is a doctor in Dublin. Summary: The speakers, Palav Babaria and Aisling O’Riordan are both doctors from America and Ireland, respectively. At the time they are both volunteering in Haiti when a challenging mission is taken place. The occasion is when Jean-Paul arrived in the emergency room with a devastating condition of diabetic ketoacidosis, and the doctors did not have the proper equipment to treat the condition. The audience of the article is people it appeals to, while the audience in the story is Jean-Paul’s family and the doctors. The purpose of this article is to prove the need for universal test strips for people with diabetes, so they are easily accessible and not extremely expensive to purchase. The subject is Jean-Paul, in order to give an example of why universal test strips are extremely important. The tone of this article is urgency; without these test strips, people will die. One part of this article that I found extremely interesting is the lack of equipment in other countries compared to America: "American hospital protocols for diabetic ketoacidosis recommend conducting lab tests every two hours, monitoring sugars hourly and readjusting the insulin drips accordingly. Our lab lacked any of the tests usually used to monitor ketoacidosis.” I do not think people in America realize how fortunate we are to have an extensive amount of technology that saves lives. If Jean-Paul were in America at this time, it would have been much easier to care for him. Claim: Intercultural doctors Palav Babaria and Aisling O’Riordan fought a harsh battle that could not be won due to lack of medical equipment, and therefore stating that advanced medical equipment is necessary worldwide. Question: There are many deaths due to diabetes, Jean-Paul as an example. Do you think it is more important to invest funds for universal test trips or more common illnesses such as cancer?