EBM_BrownMacIntyre2014_Final - Spiral
advertisement

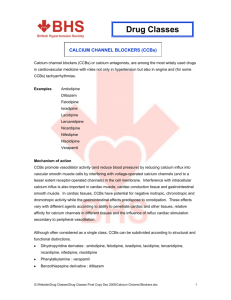
Commentary On : Flenady V, Wojcieszek AM, Papatsonis DN, Stock OM, Murray L, Jardine LA, Carbonne B. Calcium channel blockers for inhibiting preterm birth. Cochrane database Syst Rev. 2014 Jun 5;6:CD002255 Declarative Title- Calcium channel blockers as first line for tocolysis in the management of preterm labour? Richard G Brown1 and David MacIntyre1,* 1Imperial College Parturition Research Group, Division of the Institute of Reproduction and Developmental Biology, Imperial College London, UK *Correspondence to: Dr David MacIntyre, Imperial College Parturition Research Group, Division of the Institute of Reproduction and Developmental Biology, Imperial College London, Hammersmith Campus, London, W12 0NN, UK Context (word count 799) Preterm birth (PTB) remains the leading cause of neonatal morbidity and mortality. Although tocolytics do not reduce the risk of PTB they effectively delay delivery by 48 hours (1). This creates a window of opportunity for corticosteroid administration and transfer to units with neonatal intensive care facilities, which improves neonatal mortality and morbidity (2). However a consensus on the most effective tocolytic does not exist. This study aimed to assess the effects of calcium channel blockers (CCBs) on maternal, fetal and neonatal outcomes when administered to women in preterm labour. Methods This was an updated review of randomised trials using CCBs as tocolytics for PTB management. Maternal, fetal and neonatal outcomes were compared between CCBs (mainly nifedipine), no treatment, placebo and other tocolytics. High and low dose Nifedipine regimes and long-term childhood outcomes were also reviewed. Six core outcomes were identified across all trials; birth <48 hours after trial entry, PTB <34 weeks, serious maternal and infant outcomes, perinatal mortality, and maternal adverse effects (MAE). Results were presented using risk ratio (RR), number needed to treat to benefit (NNTB) and number needed to treat to harm (NNTH) for categorical data and mean difference with 95% confidence intervals (CI) for continuous data. Findings Twenty-six additional trials were included in the update providing a combined total of 38 trials, involving 3550 women. Two trials comparing CCBs with placebo or no treatment showed that CCBs significantly reduced birth <48hrs after trial entry (RR 0.3, 95% CI 0.21 to 0.43) and increased MAE (RR 49.89, 95% CI 3.13 to 795.02). Primary birth and perinatal mortality outcomes were unchanged <48 hours post-treatment, however CCBs performed better than betamimetics with fewer MAEs (RR 0.36, 95% CI 0.24 to 0.53), longer interval between trial entry and birth (4.38 days, 95% CI 0.25 to 8.52), increased gestational age at birth (0.71 weeks, 95% CI 0.34 to 1.09), reduced respiratory distress syndrome (RR 0.64, 95% CI 0.48 to 0.86), necrotizing enterocolitis (RR 0.21, 95% CI 0.05 to 0.96), intraventricular haemorrhage (RR 0.53, 95% CI 0.34-0.84), neonatal jaundice (RR 0.72, 95% CI 0.57 to 0.92) and neonatal intensive care (NICU) admissions (RR 0.74, 95% CI 0.63 to 0.87). CCBs were also associated with fewer MAEs (RR 0.52, 95% CI 0.40 to 0.68) and NICU stays (RR -4.55 days, 95% CI -8.17 to -0.92) compared to magnesium sulphate (MgSO4). In comparison to oxytocin receptor antagonists (ORA), CCBs showed reduced PTB rates (RR 0.64, 95% CI 0.47 to 0.89), reduced admission (RR 0.59, 95% CI 0.41 to 0.85) and length of NICU stay (RR -5.4 days, 95% CI -10.84 to 0.04) plus increased gestational age at birth (1.2 weeks, 95% CI 0.25 to 2.15). However, MAEs were comparatively higher in the CCBs group (RR 2.61, 95% CI 1.43 to 4.74). Using limited data from small trials, no differences were seen between CCBs and other tocolytics (e.g. NSAIDs, GTN), high vs low dose nifedipine or longterm childhood outcomes. Commentary This study provides a timely review and assessment of CCBs for inhibiting preterm labour and birth. The findings suggest that despite increased minor and potentially modifiable MAEs, nifedipine is an effective first line tocolytic. No serious maternal or infant outcomes were recorded in this review. Previous safety concerns regarding CCBs stem primarily from their use in combination with other tocolytics (3). As acknowledged by the authors, findings are limited by lack of blinding in reported trials, raising the possibility of bias particularly for subjective outcomes of maternal and neonatal morbidity. Inconsistent, suboptimal reporting limits definitive conclusions being drawn in key areas including tocolytic use in twin pregnancies and following preterm prelabour rupture of membranes (PPROM). The updated review is strengthened by the inclusion of 26 additional trials, allowing some assessment of efficacy. Two small trials (173 women) indicate that CCBs exhibit superior efficacy compared to placebo or no treatment. Nifedipine is affordable, accessible, orally administered, delays labour for >48 hours and appears beneficial compared to Atosiban and MgSO4, consistent with a recent network metaanalysis identifying prostaglandin inhibitors and CCBs as having the highest likelihood of delaying delivery by 48 hours and improving neonatal outcomes(1). Further randomised, blinded trials with high quality reporting are required to improve the evidence that CCBs be used first line. There remains the need to clarify; optimum dosage and preparation, long-term childhood outcomes, use in combination with MgSO4 (increasingly used in PTB for fetal neuroprotection) and suitability for tocolysis in PPROM and multiple gestations. References 1. Haas DM, Caldwell DM, Kirkpatrick P, McIntosh JJ, Welton NJ. Tocolytic therapy for preterm delivery:systematic review and network meta-analysis. BMJ.345;2012 2. Crowley P. Prophylactic corticosteroids for preterm birth (Cochrane Review) In: The Cochrane Library. ChichesterUK:Wiley;2004 3. Oei SG. Calcium channel blockers for tocolysis: a review of their role and safety following reports of serious adverse events. Eur J Obstet Gynecol Reprod Biol.Jun 1;126(2):137-45.2006