Human Factors Categories and GMC TD Outcomes v6
advertisement

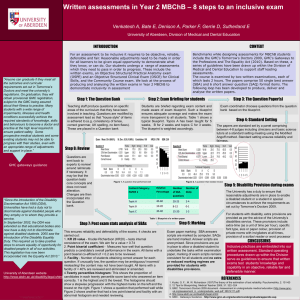
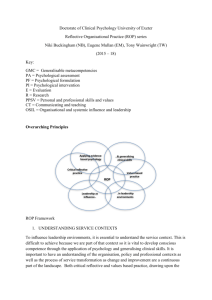
Human Factors Curriculum Mapping Aim To provide a structure that allows students, teachers and external reviewers to see how we teach and assess Human Factors science Objectives 1. 2. 3. 4. Align Human Factors constructs with one or more GMC TD outcomes and Situational Judgement Test domains. Enable indexing of Human Factors learning and assessment resources Identify gaps in current GMC TD outcomes Discuss the pros and cons of aligning each GMC TD outcome with only one Human Factors construct. For example: Pro: this will facilitate linking of assessment and teaching resources to Human Factors constructs because GMC TD outcomes are already used to index these resources. Con: this sets artificial boundaries on the content of the Human Factors constructs Notes The Table is constructed around Human Factors Categories (Systems, Human interaction, Environment, Equipment and Personal) from Human Factors in Healthcare1. These categories have been used because they are the foundation for the forthcoming Human Factors Course Components from NES and the Clinical Skills Managed Education Network. The Human Factors Constructs are listed to provide additional detail but the order of these Constructs is not intended to suggest that they link to specific GMC TD outcomes, which are in numerical order. The sources for the Human Factors Categories and Constructs are Safety at the Sharp End, A Guide to Non-Technical Skills,2 Human Factors in Healthcare,1 Evie Fioratou and Steph Russ. Figure 1: Human Factors Approach: Adapted from Flin 20082, Flin 20093 and Moray 20004 with Human Factors Categories from Rosenorn-Lanng 20141 SYSTEMS ENVIRONMENT Coping Ergonomics Leadership Compatibility Standardisation Safety culture, management style Situation awareness Communication, co-ordination PATIENT User interaction and training PERSONAL Physical environment (noise, temperature) EQUIPMENT Decision making Adverse event management and reporting HUMAN INTERACTION Interruptions/ distractions Team working, team culture Regulatory influences, guidelines, standards , policies References 1. Rosenorn-Lanng D. Human Factors in Healthcare Level One. Oxford: Oxford University Press, 2014. 2. Flin R, O'Connor P, Crichton M. Safety at the Sharp End: A Guide to Non-Technical Skills. Oxford: Ashgate, 2008. 3. Flin R, Winter J, Sarac C, Raduma M. Human Factors in Patient Safety: Review of Topics and Tools 2009 [Cired 29 May 2011] Available from: http://www.who.int/patientsafety/research/methods_measures/human_factors/human_factors_review.pdf 4. Moray N. Culture, politics and ergonomics. Ergonomics 2000;43(7):858-68. Justification for Introduction to Human Factors Science in Principles: GMC Outcome 9 Apply psychological principles, method and knowledge to medical practice. 9.a Explain normal human behaviour at an individual level Human Factors Constructs linked to GMC Tomorrow’s Doctors Outcomes and Situational Judgement Test (SJT) Domains Key to sources for constructs Black: All sources (Safety at the Sharp End, Rhona Flin, NES, Human Factors in Healthcare, Evie Fioratou and Steph Russ) Blue: Evie Fioratou and Steph Russ Red: NES Human Factors Course Components and/or Human Factors in Healthcare, Debbie Rosenorn-Lanng Category Human Factors Science Constructs GMC Tomorrow’s Doctors Outcomes or Standards and Situational Judgement Test (SJT) Domains Systems GMC TD Outcomes Regulatory influences (standards, 11 Apply to medical practice the principles, method and knowledge of population health and the guidelines, SOPs) improvement of health and healthcare. Culture 11b Assess how health behaviours and outcomes are affected by the diversity of the patient population. Adverse event management and 11c Describe measurement methods relevant to the improvement of clinical effectiveness and care. reporting 11d Discuss the principles underlying the development of health and health service policy, including issues Normalisation of deviance relating to health economics and equity, and clinical guidelines. Staffing levels 11j Discuss from a global perspective the determinants of health and disease and variations in healthcare Information systems delivery and medical practice. Information flow 23 Protect patients and improve care 23.a Place patients’ needs and safety at the centre of the care process. 23.b Deal effectively with uncertainty and change. 23.c Understand the framework in which medicine is practised in the UK, including: the organisation, management and regulation of healthcare provision; the structures, functions and priorities of the NHS; and the roles of, and relationships between, the agencies and services involved in protecting and promoting individual and population health. 23.d Promote, monitor and maintain health and safety in the clinical setting, understanding how errors can happen in practice, applying the principles of quality assurance, clinical governance and risk management to medical practice, and understanding responsibilities within the current systems for raising concerns about safety and quality. Standard 66 Medical schools’ policies for the training, conduct and assessment of students should have regard for the variety of cultural, social and religious backgrounds of students, while maintaining consistency in educational and professional standards. Standard 104 From the start, students must have opportunities to interact with people from a range of social, cultural, and ethnic backgrounds and with a range of disabilities, illnesses or conditions. Such contact with patients encourages students to gain confidence in communicating with a wide range of people, and can help develop their ability to take patients’ histories and examine patients. SJT Domains Commitment to Professionalism; Learning and Professional Development Patient Focus; Human Interaction Communication – written and verbal Leadership Team working Workload management Conflict resolution Supporting others Checklists Handovers Safety briefs/ debriefs Hierarchy and authority gradients Transitions Praise and respect GMC TD Outcomes 15 Communicate effectively with patients and colleagues in a medical context 15.a Communicate clearly, sensitively and effectively with patients, their relatives or other carers, and colleagues from the medical and other professions, by listening, sharing and responding. 15.b Communicate clearly, sensitively and effectively with individuals and groups regardless of their age, social, cultural or ethnic backgrounds or their disabilities, including when English is not the patient’s first language. 15.h Communicate effectively in various roles, for example, as patient advocate, teacher, manager or improvement leader. 21 Reflect, learn and teach others 21.d Manage time and prioritise tasks, and work autonomously when necessary and appropriate. 21.e Recognise own personal and professional limist and seek help from colleagues and supervisors when necessary 21.f Function effectively as a mentor and teacher including contributing to the appraisal, assessment and review of colleagues, giving effective feedback, and taking advantage of opportunities to develop these skills. 21.g Demonstrate awareness of the role of doctors as managers, including seeking ways to continually improve the use and prioritisation of resources. 22 Learn and work effectively within a multi-professional team 22.a Understand and respect the roles and expertise of health and social care professionals in the context of working and learning as a multi-professional team. 22.b Understand the contribution that effective interdisciplinary teamworking makes to the delivery of safe and high quality care 22.c Work with colleagues in ways that best serve the interests of patients, passing on information and handing over care, demonstrating flexibility, adaptability and a problem-solving approach. 22.d Demonstrate ability to build team capacity and positive working relationships and undertake various team roles including leadership and the ability to accept leadership by others. 23.e Understand and have experience of the principles and methods of improvement, including audit, adverse incident reporting and quality improvement, and how to use the results of audit to improve practice. 23.f Respond constructively to the outcomes of appraisals, performance reviews and assessments. SJT Domains Effective communication. Working Effectively as part of a team Environment Ergonomics Physical environment (noise, temperature) Interruptions/ distractions Familiarity Patient journeys Equipment Personal Consumables o Medicines o Disposable devices Non-consumables o Medical devices o Domestic (beds, bathrooms) User interaction with equipment Standardisation Compatibility Training Datix/ equipment for complaints and incident reporting Human performance limitations Decision making Situation awareness Managing stress and coping with fatigue Resilience Task management/ workload Speaking up Risk taking behaviour Empathy Person-centred care Cognitive aids Self awareness GMC TD Outcomes 17. Prescribe drugs safely, effectively and economically 17.c Provide a safe and legal prescription 17.d Calculate appropriate drug doses and record the outcome accurately 17.e Provide patients with appropriate information about their medicines 17.f Access reliable information about medicines 17.g Detect and report adverse drug reactions 18 Carry out practical procedures safely and effectively. 18.a Be able to perform a range of diagnostic procedures as listed in Appendix 1and measure and record the findings 18.b Be able to perform a range of therapeutics procedures as listed in Appendix 1 18.c Be able to demonstrate correct practice in general aspects of practical procedures, as listed in Appendix 1 GMC TD Outcomes 14 Diagnose and manage clinical presentations 14.f Make clinical judgements and decisions, based on the available evidence, in conjunction with colleagues and as appropriate for the graduate’s level of training and experience. This may include situations of uncertainty. 14.g Formulate a plan for treatment, management and discharge, according to established principles and best evidence, in partnership with the patient, their carers, and other health professionals as appropriate. Respond to patients’ concerns and preferences, obtain informed consent, and respect the rights of patients to reach decisions with their doctor about their treatment and care and to refuse or limit treatment. 21 Reflect, learn and teach others 21.a Acquire, assess, apply and integrate new knowledge, learn to adapt to changing circumstances and ensure that patients receive the highest level of professional care. 21.b Establish the foundations for lifelong learning and continuing professional development, including a professional development portfolio containing reflections, achievements and learning needs. 21.c Continually and systematically reflect on practice and, whenever necessary, translate that reflection into action, using improvement techniques and audit appropriately − for example, by critically appraising the prescribing of others. 21.e Recognise own personal and professional limits and seek help from colleagues and supervisors when necessary. 22 Learn and work effectively within a multi-professional team 22.i Recognise own personal health needs, consult and follow the advice of a suitably qualified professional, and protect patients from any risk posed by own health. 22 .j Recognise the duty to take action if a colleague’s health, performance or conduct is putting patients at risk SJT Domains Problem solving and decision--‐making; Self--‐awareness and insight; Organisation and planning Coping with pressure