Ophthalmology
advertisement

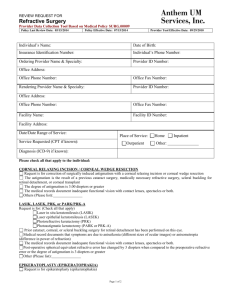
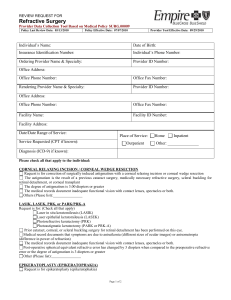
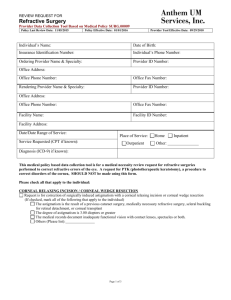
DAvMed 44 Ophthalmology - 46/695 KCL 2011 OPHTHALMOLOGY 3 Introduction 3 Visual requirements for aviation RAF visual standards Poor vision in one eye 3 3 3 Refractive error in aviation Variation of refraction with age Hypermetropia (HM) Myopia Astigmatism Anisometropia Presbyopia 3 3 4 4 4 5 5 Management of refractive error in aircrew Corrective Flying Spectacles (CFS) Aircrew Contact Lenses (CL) Refractive surgery Radial keratotomy (RK) Photorefractive keratotomy (PRK) LASEK LASIK Wave-front aberrometry Other techniques Aeromedical disposal 5 5 6 6 6 6 6 7 7 7 7 Ophthalmic history and examination Visual acuity Testing for hypermetropia Testing accommodation Testing convergence Stereopsis Testing ocular muscle balance Cover/uncover test Alternate cover test Prism cover test Maddox rod Maddox wing Colour vision Electronic Flight Instrumentation Systems (EFIS) Measuring and grading colour perception Visual fields Amsler grid 8 8 8 8 8 8 9 9 9 10 10 10 10 11 11 12 12 Ophthalmic diseases commonly encountered in aviators Ocular adnexae Blepharitis Chalazion (meibomian cyst) Epiphora Orbital blow-out fracture Ocular anterior segment Episcleritis Recurrent erosion syndrome Keratoconjunctivitis sicca Microbial keratitis Adenviral keratoconjunctivitis Herpetic keratitis Keratoconus 13 13 13 13 13 13 14 14 14 14 14 15 15 15 ©Jean-Michel Ferrieux-2011 1 DAvMed 44 Uveitis Ocular hypertension and glaucoma Cataracts Retinal diseases Retinal detachment Centroserous chorioretinopathy (CSC) Central retinal vein occlusion Neurophthalmology Amblyopia and squint Optic neuropathy Abnormal pupillary reactions Migraine Ophthalmic drugs ©Jean-Michel Ferrieux-2011 Ophthalmology - 46/695 KCL 2011 16 16 17 18 18 18 18 19 19 19 20 20 20 2 DAvMed 44 Ophthalmology - 46/695 KCL 2011 Ophthalmology INTRODUCTION Sight is the most important sense used in aviation. When it comes to pilots, any new ophthalmic interventions must be evaluated carefully to ensure that the risks are outweighed by the benefits of the procedure. VISUAL REQUIREMENTS FOR AVIATION 2 eyes to see distant and near objects clearly. Normal ocular muscle balance. Normal colour vision Full visual fields Stereopsis present to the required standards. RAF visual standards Poor vision in one eye An individual with a single or a single-seing eye can fly safely with certain restrictions. o Slightly reduced VF o No stereoscopic vision o Increased risk of complete visual incapacitation. Class I pilots who become uniocular are restricted OML. REFRACTIVE ERROR IN AVIATION Variation of refraction with age The majority of neonates are hypermetropic. The magnitude then increases. @ ≈ 8 years, the refraction becomes relatively myopic. By the end of the 3rd decade, refractive stability is attained. During middle age, accommodation decreases (increasing hypermetropia). Myopia develops after the 7th decade (higher refractive index of the nucleosclerotic crystalline lens) Myopes ➪earlier and more rapid myopic progression than hypermetropes. o ⚠in assessing and accepting young (low) myopic candidates for aviation training. ©Jean-Michel Ferrieux-2011 3 DAvMed 44 Ophthalmology - 46/695 KCL 2011 Hypermetropia (HM) Light is focused behind the retina (eye too small) o Both distance and near objects are blurred. o The young eye can compensate with accommodation o Reading glasses are required @ an younger age than normal. Axial HM is the most common type. Aphakia is an extreme example of acquired refractive HM. Hypermetropia can be divided into: o Manifest HM: = strongest convex lens correction accepted for clear distance vision. o Latent hypermetropia: = remainder of the HM, masked by ciliary tone and involuntary accommodation. o Facultative hypermetropia: = HM that is overcome by accommodation. o Absolute hypermetropia: = HM in excess of the amplitude of accommodation. Hypermetropia is corrected with a convex (+) lens. Myopia Light is focused in front of the retina (eye too large). o Distant objects are blurred. o Near objects are seen clearly. Caused by: o Often abnormally long eye: In high myopia, ➪out-pouching of the posterior segment (posterior staphyloma) o Increased dioptric power (refractive or index myopia): Keratoconus Nucleosclerosis Grades of myopia: o Low myopia: < -4.00 D o Moderate myopia: -4.OO to -7.75 D o High myopia: -8.00 to -12.00 D o Extreme myopia: > -12.00 D o The 2 latter are associated with myopic macular degeneration and peripheral retinal degeneration, and a 4% lifetime risk of detachment. Myopia is corrected with concave (-) lenses. Axial myopia becomes manifest in the early teens and is stabilized around the age of 24. Reading associated with higher education induces progression of myopia. Astigmatism The refractive power of the astigmatic eye varies in different meridians. Several types of regular astigmatism: o Compound hypermetropic astigmatism (CHA): all rays are focused behind the retina. o Simple hypermetropic astigmatism (SHA): rays in one meridian focus on the retina and the other come to focus behind the retina. o Mixed astigmatism (MA): one line focus in front of the retina and the other focuses behind the retina. o Simple myopic astigmatism (SMA): Converse of SHA o Compound myopic astigmatism (CMA): Converse of CHA. Astigmatism is corrected with a lens that is stronger in one meridian than the other. o 2 types of astigmatic lenses: Cylindrical lenses: have one plain surface and form a part of a cylinder. Toric lenses: spherical lens with a cylindrical lens superimposed upon it. Can be defined as a fraction DS/DC ©Jean-Michel Ferrieux-2011 4 DAvMed 44 Ophthalmology - 46/695 KCL 2011 o e.g. if +2.OO in one meridian and +4.00 in the other (at 90°): o ➪+2.00DS/+2.00DC×90° = +2.00/+2.00DC×90° Anisometropia The refraction of the two eyes differs. o Small degrees of anisometropia are commonplace and of no significance. o Large degrees in childhood ➪significant cause of refractive amblyopia. A disparity > 1D in a hypermetrope ➪amblyopia of the most hypermetropic eye. Myopes with anisometropia are less likely to develop amblyopia because both eyes have clear vision. o But if one eye is highly myopic, it usually becomes amblyopic. o Myopes who have been anisometropic for all their lives tolerate a higher degree of anisometropia (≥ 2D) Adulthood anisometropia ➪eye strain and diplopia. Presbyopia The amplitude of accommodation declines steadily with age: o Sclerosis of the crystalline lens fibres. o Decrease efficiency of the ciliary muscle. o 14 dioptres accommodation in infancy o 4 dioptres @ 45. o ⅓ of the available accommodation must be kept for comfortable near vision: o ➪Difficulty or discomfort with near vision @ 25 cm when accommodation has decayed to 6 dioptres (40-45 year old) The onset of presbyopia occurs earlier with uncorrected hypermetropia. MANAGEMENT OF REFRACTIVE ERROR IN AIRCREW Refraction error in aircrew is corrected with: o Corrective Flying spectacles (CFS) o High-water-content soft contact lenses (CL). Corrective Flying Spectacles (CFS) Aircrew requiring refractive correction are not permitted to use their own civilian spectacles for flying duties. Defence-issue CFS are suitable for working environment (performance and robustness). A spare pair of CFS must be carried in an accessible place during flying. 2 CFS designs: o General-purpose frame (9021A) o Wrap-around shape frame (9013A) for use with aircrew respirators and AR5 hood. o Both have anti-scratch and anti-reflection coatings. A full range is available: o Single-vision lens o Multifocal lenses: Bifocal (+ executive bifocals, D-segment bifocals Trifocal Progressive lenses have an area of peripheral distortion outside the transition zone of increasing power ➪limited VF. Contraindicated for fast-jet aircrew. o Half-eye reading design. Significant problems in terms of comfort and safety: ©Jean-Michel Ferrieux-2011 5 DAvMed 44 Ophthalmology - 46/695 o Mechanical failure of the CFS o Lens obscuration due to misting or sweat accumulation. KCL 2011 Aircrew Contact Lenses (CL) Preferred option for visual correction across all aircrew groups. Most of them wear daily disposable CL, but they are not used in astigmatism or dry eye. Different methods to stabilize CL orientation (astigmatism correction): o Prism-ballast. o Thin zones that use the eyelid pressure on blinking. Silicone-hydrogel CL are made of low-water-content, highly O2-permeable material. o Used for dry eyes and eyes with high corneal O2 demands. Aircrew problems with CL: o Are usually related to dehydration from individual or environmental factors: Aircrew have a reduced blink rate. Dry atmosphere due to air-conditioning. Often inadequate fluid intake. o Occasional problems with lens movement. o Corneal hypoxia: Wear CL max 12 hours/ day and 6 days/ week. Not during sleep. o Microbial keratitis is a risk of soft CL use. Presbyopia is a problem as there is no truly successful soft bifocal CL. Refractive surgery Radial keratotomy (RK) Series of corneal cuts: o In a spoke-shaped pattern around the pupil o Penetrating 85-95% of the depth of the cornea o ➪Flattening the centre in order to correct myopia. Problems of RK: o Permanently weakened cornea o Healing of the incisions ➪regression of the myopic correction o Change of refraction during the day and at altitude RK is not approved for flying duties. Photorefractive keratotomy (PRK) The anterior corneal surface is reshaped by photo-ablation (UV excimer laser). o Corneal epithelium removed before treatment and grows back over the treated zone after 4-6 days. o Unaffected integrity of the globe. o Refractive stability within 3-6 months Problems with PRK: o Night vision abnormalities (minimized if a sufficient corneal zone is reshaped) o Haze by corneal tissue healing o Regression of the refractive correction by corneal tissue healing Abolished with improvements in laser techniques and indication to lower orders of myopia (< -6.00 dioptres). Approved for flying duties LASEK LASer Epithelial Keratomileusis o Displacement of an epithelial flap ©Jean-Michel Ferrieux-2011 6 DAvMed 44 Ophthalmology - 46/695 o Replaced after the laser treatment and acts as a bandage o Recovery is faster and less painful than with standard PRK. Approved for flying duties. KCL 2011 LASIK LASer In-situ Keratomileusis o Most popular refractive surgical technique at present o More predictable and safer method of correcting high levels of myopia and low hypermetropia o Cutting a thin flap of corneal tissue, ablating the underlying stromal bed and replacing the flap. o ≈ 85% of patients will achieve 6/6 or better. Problems with LASIK: o Night-vision abnormalities Loss of contrast sensitivity Haloes and starbusts around light sources o Often dry eye, requiring lubricants (up to 6 months post-op) o The flap often takes several months to years to heal, and sometimes doesn't heal at all. o The flap can become inflamed and melt or be displaced. Epithelial cells may grow under it. o Corneal ectasia can occur after LASIK for high myopia. LASIK is not approved for flying duties. Wave-front aberrometry Allows very accurate correction of ametropia, (++ after CRS with a "poor" result) Increases the proportion of patients who achieve excellent vision after treatment and is the most suitable for aircrew ("super-vision"). Other techniques Implantation of multifocal or accommodative intraocular lens (IOL) for correction of prebyopia. Implantable contact lenses (ICL), capable of correcting individuals with high amounts of near- or far-sightedness beyond the range of LASIK (< -15.00 and > +6.00 dioptres). Intrastromal corneal ring implants (INTACS™) place at the edge of the cornea. Are useful for correcting keratoconus. Diode lasers that gently heat spots near the edge of the cornea to correct hypermetropia and astigmatism. Indication ++ for patients > 40 years. Laser thermal keratoplasty (LTK) uses a similar technique. Aeromedical disposal Military: o PRK, LASEK and wave-front are approved (at the risk and expense of the individual). o RK and LASIK are not approved. Civilian: o Class 1 after minimum 1 year after operation Preoperative refraction must be ≤ ±5.00 dioptres Assessment by CAA eye specialist before certification o Class 2 after minimum 1 year after operation Preoperative refraction must be maximum +5.00 or -8.00 dioptres. AME report from an ophthalmologist about the surgery and results. ©Jean-Michel Ferrieux-2011 7 DAvMed 44 Ophthalmology - 46/695 KCL 2011 OPHTHALMIC HISTORY AND EXAMINATION Visual acuity Uniocular distance visual acuities are assessed with a backlit Snellen chart at 6 metres. o The VA is recorded as the lowest line that is read correctly and completely. o Test performed unaided and then with spectacle correction. Common errors: o Wrong distance o Too much light in the chart causing glare and surface reflection o Pressed occluded eye o Use or narrowed palpable fissures Uni- and binocular near acuity are tested: o With the normal reading correction o Using standard test types at 33 cm. Testing for hypermetropia Important to identify individuals who may be manifestly hypermetropic and who "compensate" their refractive error by accommodating to achieve a normal unaided VA. o Manifest HM can be diagnosed with a convex lens (+2.50D): An emmetropic individual who achieves 6/6 without correction will not be able to achieve that with a +2.5D lens. If the patient can read the line with the lens, ➪manifest HM is at least +2.5D. It is necessary sometimes to measure the total degree of HM by refraction using a topical cycloplegic (Mydrilate) which causes cycloplegia and mydriasis. Testing accommodation Accommodation may be quantified uniocularly and binocularly with and without correction, using the RAF near-point rule. Testing convergence The line-and-dot test on the RAF near-point rule is used: o Subjective convergence: distance at which the patient declares seeing the line being doubled o Objective convergence: distance at which one eye diverges suddenly as the drum advances. Convergence weakness will often cause eyestrain (asthenopia). Stereopsis Ability to obtain an impression of depth by the superimposition of 2 images. o Results from normal visual pathways, optimally developed. o Only a subject possessing fully developed and integrated vision and eye-movement control may perceive stereopsis. o Full maturity between the ages of 7-10 years. o Subsequent stimulation to the visual system will have no significant effect in enhancing stereoscopic vision in a similar fashion to amblyopia. Psychological 3-dimensional vision is depth perception independent of stereopsis, gained by knowledge and experience of the known environment. Stereopsis is a requirement for pilots. ©Jean-Michel Ferrieux-2011 8 DAvMed 44 Ophthalmology - 46/695 Assessment of stereopsis with the TNO test (Toatepast Natuurwetenschep Onderzoek). o The plates contain: Visible features which can be seen with and without the red-green spectacles Hidden shapes, which are only apparent when the red-green spectacles are worn and stereopsis is present. o TNO test provides a true measurement of stereopsis, as there are no monocular clues. KCL 2011 The Frisby test is a simpler test that can also be used in aircrew. Testing ocular muscle balance Normally, when the eyes are regarding a distant object, the visual axes are parallel. Orthophoria: = State of ocular balance with image fusion without effort. Ocular imbalance results of varying degrees of squint or strabismus: o Manifest deviation = tropia o Latent deviation = phoria Phoria = latent ocular misalignment, in which the ocular balance is maintained with effort. Diplopia is rare in a congenital squint. Cover/uncover test Monocular test designed to diagnose heterotropia. o If the left eye shows any displacement of the corneal light reflex, then the examiner should cover the opposite (right) eye in search for any movement of that eye. o Exotropia: nasal movement to take up fixation o Esotropia: temporal movement to take up fixation o Hypertropia: downward movement o Hypotropia: upward movement. Alternate cover test Test for heterophoria and is performed only if the cover/uncover test is normal. o One eye is covered for ≈ 2", the shifted quickly to the other eye. o Note any movement of the uncovered eye: Orthophoria: no movement Exophoria: nasal movement Esophoria: temporal movement Hyperphoria: downward movement Hypophoria: upward movement. A patient with heterophoria will have: o Straight eyes during the cover/uncover test o Straight eyes before and after the alternate cover test o A deviation during the test is being performed. ©Jean-Michel Ferrieux-2011 9 DAvMed 44 Ophthalmology - 46/695 KCL 2011 Prism cover test Measures the total deviation (latent & manifest). Does not separate tropia from phoria. The angle of deviation is measured from the strength of the prism. Gold standard in the measurement of ocular deviation. Maddox rod The red rods are placed, by convention, in front of the right eye The amount of dissociation is measured by the superimposition of the 2 images (white dot from left eye and red streak from right eye) using the handheld prism. o The base of the prism is placed in a position opposite to the direction of the deviation. Maddox wing Dissociates the 2 eyes for near fixation at 33 cm and measures the amount of heterophoria. o The right eye sees only a white vertical arrow and a red horizontal arrow o The left eye sees only a horizontal and a vertical row of numbers. o The horizontal deviation (exo/eso) is measured by the seen position of the vertical arrow o The vertical deviation (hyper/hypo) is measured by the seen position of the horizontal arrow. o A cyclophoria (rotational deviation) can be measured by asking the patient to move the horizontal arrow so that it is parallel with the horizontal row of numbers. Colour vision Modern cockpits, military and civilian, and ATC screens use colour displays. Colour-defective pilots have significantly reduced target acquisition and lower reaction times to coloured visual stimuli. 3 classes of cones are responsible for colour vision in the human eye: o S-Blue cones (1) o M-Green cones (10) o L-Red cones (10) o Concentrated in the macular region. Colour deficiency may be congenital or acquired: o Congenital Red/Green deficiency is sex-linked, 8% ♂ and 0.4% ♀ o Normal trichromats have normal amounts of all 3 types of cones. o Trichromanomalous are colour weak and are slightly deficient in one type of cones: Protanomaly: slight deficiency in the red cone type (1%♂) Deuteranomaly: slight deficiency in the green cone type (5-6%♂) Tritanomaly: slight deficiency in the blue cone type (2-7‰ of population) o Dichromats are completely colour-blind and have only 2 cone types: Protonopes lack the red cones (1%) Deuteranopes lack the green cone type (1%) Tritanopes lack the blue cone type (2-7/100000). o Red/Green deficiencies are all X-linked characteristics o Blue-blue/yellow deficiency is an allelic characteristic with an equal sex-ratio. ©Jean-Michel Ferrieux-2011 10 DAvMed 44 Ophthalmology - 46/695 KCL 2011 Acquired colour defects occur in 5-15% of the population, with no sex-ratio and typically cause a blue-yellow defect. o Associated with: Ageing Ocular disease Medications Drug ingestion: Oral contraceptives Oral diabetic agents Tetracyclines antimalarial drugs Digoxin Ethanol alcohol Tobacco Sildefanil (Viagra®) associated with a bluish tinge visually during 1-6 hours. Aviators must wait 24 hours before flying. Thiazide diuretics. Electronic Flight Instrumentation Systems (EFIS) EFIS allow colour-coded alphanumerical and analogue data for flight management and control. o Polychromatic data using more than 8 colours o Each colour can be displayed at different light intensities o With graphics ranging from very small areas to entire backgrounds. The pilot now observes these colour displays for long periods of time. The colour: o Has safety connotations o Is also used to save time when reading information: Yellow concerns power information Magenta concerns track or trajectory processing… Cockpit control images may have several juxtaposed or superimposed colours. EFIS maximizes data presentation to colour-normal aviators by exploiting the increased sensitivity of blue-yellow colour discrimination. Colour-defective people have significant functional impairment when using EFIS. Measuring and grading colour perception At present, congenital red/green colour deficiency is tested in aircrew. In the future, a test for acquired defects may be required. In the UK: o Ishihara pseudo-isochromatic plate test for colour confusion in protanopes and deuteranopes. o Standard 24-plate test. If correct answers ➪the individual is declared CP2 colour-normal. If errors ➪Holmes-Wright lantern test (military and European class 1). If no mistake in the first run ➪CP3 colour-safe. If any red/green errors ➪CP4 colour-unsafe. If any other mistakes in round one, two extra runs are performed. If no mistake on these ➪CP3. If mistakes other than red/green errors: another run is performed after a 20' dark adaptation: CP3 if no mistake, otherwise CP4. ©Jean-Michel Ferrieux-2011 11 DAvMed 44 Ophthalmology - 46/695 KCL 2011 CP1 for passing test performed with low brightness in a light room: is an entry standard for Royal Naval aviation. Visual fields "Is an island of vision surrounded by a sea of darkness". 3 dimensional structure covering ≈ o 60° nasally o 90° temporally o 50° superiorly o 70° inferiorly o VA is sharpest at the very top of the island and then declines progressively towards the periphery. Nasal slope steeper than the temporal slope. o Blind spot located temporally between 10-20°. Absolute scotoma = total loss of vision Relative scotoma = area of partial loss within which some targets can be seen and others not. No set minimum VF set for aviation. Homonymous or bitemporal defects, both hemianopic and quadranopic, are not accepted as safe. Amsler grid Is used to test macular function and to detect central or paracentral scotomata. Failure to see the central dot indicates a central scotoma. ©Jean-Michel Ferrieux-2011 12 DAvMed 44 Ophthalmology - 46/695 KCL 2011 OPHTHALMIC DISEASES COMMONLY ENCOUNTERED IN AVIATORS Ocular adnexae Blepharitis Chronic blepharitis is an inflammation of the eyelid margins. Very common. May interfere with the wearing of CL. May aggravate the treatment of dry eyes. Foreign body sensation + mild photophobia + lid crusting. Frequently worse in the morning. Treatment of anterior blepharitis is with lid hygiene. Treatment of posterior blepharitis is with systemic antibiotics. Chalazion (meibomian cyst) Chronic inflammatory lesion caused by blockage of one of the meibomian gland orifices, with stagnation of the sebaceous secretion. Treatment by incision or Sterdex. Epiphora Excessive tearing and can be a cause of poor vision. Cause by reflex overproduction of tears by corneal or conjunctival irritation (misdirected eyelashes or foreign bodies). Orbital blow-out fracture Does not involve the orbital rim. Is caused by a sudden increase in the orbital pressure by a striking object, Ø > 5 cm. Most frequently involves the orbital floor. o Ecchymosis o Oedema o (Subcutaneous emphysema). o Often infraorbital nerve anaesthesia (lower-lid cheek side of the nose, upper teeth and gums). o Diplopia may be caused by mechanical entrapment of the inferior rectus muscle within the fracture. Conservative initial treatment Fractures involving more than ½ of the orbital floor, with persistent diplopia, should be surgically repaired within 2 weeks. An aviator's flight category will be determined by the results of surgery. ©Jean-Michel Ferrieux-2011 13 DAvMed 44 Ophthalmology - 46/695 KCL 2011 Ocular anterior segment Episcleritis Common, benign, recurrent but self-limiting disorder. Mild uniocular tenderness and watering of the eye. Typically affects young adults. Two types: o Simple episcleritis: Demonstrates sectorial or diffuse redness. Resolves spontaneously witin 1-2 weeks. o Nodular episcleritis: Located to 1 area of the globe. Topical NSAIDs or steroids may be needed Recurrent erosion syndrome Condition in which the corneal epithelial basement membrane complex is damages by superficial corneal trauma (scratch++) Pain on waking, photophobia and blurred vision. Recurrent condition, that may cause problem for months or years. After initial treatment, prophylactic ocular lubricants are indicated. Keratoconjunctivitis sicca = dry eye, in aircrew is usually the result of meibomian gland dysfunction. o May be secondary to autoimmune diseases (Sjögren…). Treatment with topical ocular lubricants. Microbial keratitis The only microbial pathogens able to produce corneal infection in the presence of a intact corneal epithelium are: o Neisseria gonorrhea o Corynebacterium diphteriae o Listeria spp. o Haemophillus spp. Severe ocular pain and loss of vision. Sight-threatening condition. Aviators may be susceptible to this condition, especially when wearing CL in hot and dry environment. ©Jean-Michel Ferrieux-2011 14 DAvMed 44 Ophthalmology - 46/695 KCL 2011 Adenviral keratoconjunctivitis Highly contagious, common (crowded environments) viral keratoconjunctivitis. Acute onset of watering, redness, discomfort and photophobia. Both eyes affected in 60%. In severe cases, subconjunctival haemorrhages chemosis and pseudomembranes can develop. Treatment usually avoided unless the symptoms are severe (topical steroids) Isolation in order to avoid disease spread (shared towels ++) The cornea may also be affected with diffuse punctate epithelial keratitis, which resolves spontaneously. Topical steroids suppress corneal inflammation, but do not shorten the natural course of the disease. Herpetic keratitis HSV1. Dendritic ulcer that stains with fluorescein dye. Initial treatment with aciclovir 3% ointment, 5 times daily during a week. Neurotrophic sterile ulcers may occur after the primary infection. o Sterile ulcer with smooth margins. Corneal stromal disease may occur with disciform keratitis. Treatment with combination of topical steroids and antiviral cover. Necrotizing interstitial keratitis with multiple or diffuse whitish grey corneal stromal infiltrates may also occur. Keratoconus Disorder in which the cornea thins and assumes an irregular conical form. o Paracentral thinning o Corneal protrusion o Irregular astigmatism. Starts at around puberty and progresses slowly thereafter. Both eyes are affected in 85%, but the disease is asymmetrical. Often associated with eczema and atopy, with a hereditary component. Diagnosis: o Retinoscopy o Keratometry o Photokeratoscopy o Slit-lamp biomicroscopy Management: o Spectacle correction at an early stage o Hard CL to provide a regular refractive surface over the cone o Partial or full-thickness penetrating keratoplasty. A diagnosis of keratoconus or forme frustre keratoconus is a bar to aircrew selection. ©Jean-Michel Ferrieux-2011 15 DAvMed 44 Ophthalmology - 46/695 KCL 2011 Uveitis Inflammation of the uveal tract. May be subdivided into: o Anterior uveitis: The iris and, occasionally, the anterior part of the ancillary body are inflamed. o Intermediate uveitis: The posterior part of the ciliary body is affected. o Posterior uveitis: The inflammation is located behind the posterior border of the ciliary body. o Panuveitis: The entire uveal tract is involved. o Posterior and panuveitis are associated with progressive and severe visual loss. Usually requires systemic immunosuppression and will often lead to a severely restricted flying category. Anterior uveitis: o Most common type o May be: acute Photophobia, pain, redness, decreased VA, lacrimation chronic White eye and minimal symptoms even in the presence of severe inflammation. o Purplish reddish hue to the eye, keratic precipitates, cellular deposits on the corneal epithelium, flare and cells in the anterior chamber. o May be associated with arthritis and ankylosing spondylitis, in the presence of HLA-B27. Reiter's syndrome combines: Non-specific urethritis Conjunctivitis Seronegative arthritis Iritis. Rare in the general population, but more common among the aircrew population (more exposed to sources of non-specific urethritis). o Treatment with topical steroids and cycloplegia. Aircrew can attain a full flying career, but should not fly if the disease is active. Ocular hypertension and glaucoma The aqueous humour passes through the pupil into the anterior chamber, where it drains under resistance through the trabecular meshwork at the iridocorneal angle. Normal intraocular pressure (IOP) between 10-21 mmHg, (mean 16 mmHg). Glaucoma = collection of syndromes demonstrating a characteristic form of optic neuropathy, usually associated with a raised IOP. o Open or Closed iridocorneal angles o Primary or secondary. Ocular hypertension (OHT)= Raised IOP without any clinical signs of glaucoma. o ➪Increased risk of developing glaucoma. o Aircrew with OHT require annual monitoring with VF analysis. ©Jean-Michel Ferrieux-2011 16 DAvMed 44 Ophthalmology - 46/695 KCL 2011 Primary Open-Angle Glaucoma (POAG) has: o Insidious onset o Symptomatic only if extremely high IOP o Common disease (1% of population). o 10% lifetime risk of POAG if close family history. o Associated factors include: Myopia Diabetes Increasing age OHT. o Initial medical treatment using topical ocular antihypertensives. o If failure ➪surgical treatment: ++ trabeculectomy. The majority of aviators with glaucoma will continue their flying duties under medical surveillance, according to the nature of the glaucoma and the state of the VF. Cataracts Congenital or acquired opacities of the crystalline lens. Vast majority are age-related. In aircrew population, cataracts are due: o More commonly to progression of congenital lens opacities o Trauma o Ocular inflammation o Diabetes mellitus o Steroid use o Previous intraocular surgery Asymptomatic cataract o ➪unrestricted flying for trained aircrew, o But is a bar to entry to flying training. Visual symptoms of cataract include: o Blurred and reduced VA o Reduced contrast sensitivity o Significant glare o Multiple uniocular images o Progressive myopia. Surgical management: phacoemulsification with intraocular lens implant. o Unifocal lens in aircrew, selected to give minimal postoperative refractive error with maximal distance vision. o Multifocal lenses are not recommended as they reduce contrast sensitivity and increase glare. o Postoperative posterior lens-capsule opacification may occur (10%), managed using a YAG laser (yttrium-aluminium-garnet) to make a hole in the opaque capsule over the visual axis. o Specific gravity of the lens is ≈ that of the fluids of the eye: No problem under high G forces and ejection. Full return to flying duties can be expected 6-12 weeks after uncomplicated cataract surgery (with adequate visual function). ©Jean-Michel Ferrieux-2011 17 DAvMed 44 Ophthalmology - 46/695 KCL 2011 Retinal diseases Retinal detachment Fluid passes from the vitreous cavity under the retina, causiong it to separate from its retinal pigment epithelium. o Flashes of light o Floaters o "Curtain" or shadow moving across the field of vision o Peripheral or central visual loss. In aircrew population, trauma is the most common cause. Patients should be operated on at the earliest opportunity in order to preserve the macular vision. o Surgical repair: External procedure (indenting the sclera with a silicone explant) Vitrectomy with internal tamponade with silicone oil or gas. The break is then sealed by creation of a chorioretinal scar (laser retinopexy or cryopexy). Air travel contraindicated if intraocular gas. Silicone oil will not expand at altitude and can be removed at a later date, after the travel. Visual recovery depends on whether the macular has been affected and whether the VF recovers after surgical treatment. Centroserous chorioretinopathy (CSC) Idiopathic macular exudative disease that typically affects young to middle-aged men. o Localized neurosensory detachment of the macular region, caused by leakage of fluid at the level of the retinal pigment epithelium. Unilateral sudden onset blurred vision Greenish-brown positive scotoma Micropsia Metamorphopsia. ≈ 80% of eyes with CSC ➪spontaneous resolution with a return to (near)normal VA between 6-26 weeks. o Some degree of subjective visual impairment (micropsia) may persist. o Focal argon laser photocoagulation at the site of the leakage reduces the time of resolution of the serous detachment, but does not reduce the recurrence rate of CSC or prevent visual loss. Aviators with CSC are unfit to fly while having visual disturbances. Central retinal vein occlusion Associated with increasing age, systemic hypertension and blood dyscrasias. A subform affects younger patients, typically one eye of a healthy adult under the age of 40 years. o May be caused by a congenital abnormality in the central retinal vein at the level of the lamina cribrosa ➪ turbulent blood flow and thrombus formation. ©Jean-Michel Ferrieux-2011 18 DAvMed 44 Ophthalmology - 46/695 KCL 2011 Presents with: o Visual impairment, worse in the mornings o Disc oedema o Moderate amount of retinal haemorrhage Systemic causes may include: o Sarcoidosis o Behçet's disease o Autoimmune collagen vascular diseases o Anticardiolipin antibody syndrome. Usually good prognosis if no retinal ischaemia (which may give rubeosis iridis) Neurophthalmology Amblyopia and squint Potential aircrew with manifest squint and amblyopia will be screened out on selection. Amblyopia is caused by suppression of central vision from suboptimal retinal stimulation during visual development in the first 6-8 years of life. Occurs in children with: o Strabismus (strabismic amblyopia) o Unequal refractive error (anisometropic amblyopia) o As a result of uniocular visual occlusion from cataracts, ptosis or eye-lid tumours (stimulus-deprivation amplyopia). Rarely bilateral Individuals with mild form of amblyopia may, occasionally, be fit for aircrew duties. The treatment consists in: o Adequate refractive correction o Patching of the good eye before visual maturation is completed (≈ 7 years of age) Acquired squints may arise from extraocular muscle paralysis and will often cause diplopia. An individual with diplopia is unfit to flying duties. Optic neuropathy Inflammatory or demyelinisating disorders of the optic nerve. Retrobulbar neuritis is the most common type, often associated with multiple sclerosis (75% ♀ and 35% ♂) Typical presentation includes: o Acute onset of monocular visual loss o Periocular discomfort (worse on moving the eye) o Front headache o Tenderness of the globe o A few patients have papillitis o ➘➘ VA o ➘ colour vision 75% patients recover their VA within 4-6 weeks, but colour vision and contrast sensitivity often remain abnormal. Treatment of the acute phase with intravenous and oral steroids, but without improvement of the final visual outcome. An aviator must regain normal VA, normal VF and normal colour vision to be allowed to return to flying duties. ©Jean-Michel Ferrieux-2011 19 DAvMed 44 Ophthalmology - 46/695 KCL 2011 Abnormal pupillary reactions Anisocoria is either episodic or constant. Episodic anisocoria: o Migrainous episodes, ocular inflammation or benign pupillary dilation Constant anisocoria: o With sluggish pupil reactions to light is likely to be a Holmes-Adie syndrome (associated with a diminished Achilles tendon reflex) Unilateral in 80% Affected pupil is typically large and irregular Absent or very slow light reflex Patients have difficulties with glare and accommodation. Diagnosis with instillation of Pilocarpine 0.1%: Normal eye will not constrict Holmes-Adie pupil will constrict o Constant anisocoria with good light reactions in both eyes, but which is greater in dim light, ➪Horner's syndrome Usually unilateral Mild ptosis Myosis Apparent enophthalmos caused by the ptosis. Heterochromia iridis if the lesion is congenital May be associated with o Lung tumours o Carotid and aortic aneurysms o Neck lesions o Brainstem vascular disease… Migraine Recurrent attacks of headache, variable in intensity, frequency and duration, and often with familial tendency. Commonly unilateral attacks Associated with anorexia, nausea and vomiting. Classic migraine often includes: o Visual aura (bright or dark spots, zigzag lines, scintillating scotomata) Retinal migraine is a rare variant with acute transient unilateral visual loss (≡ amaurosis fugax, requiring cardiovascular investigations) Migraine is a bar to flying duties. OPHTHALMIC DRUGS Aircrew will usually be able to fly while using topical medications (if no visual function alteration) Cycloplegic drops will cause mydriasis and cycloplegia, glare and visual aberrations: NO FLYING α-sympathetic agonists also cause mydriasis: NO FLYING. Myotic drops (pilocarpine) cause a reduction of VF (pupillary constriction): NO FLYING Topical ß-blockers are used in glaucoma and may have systemic side effects in susceptible individuals, but are usually well tolerated in aircrew. When selecting a treatment for an aviator, the pharmalogical vehicle should be considered. It is prudent to tailor the medication to suit the needs of the aircrew. ©Jean-Michel Ferrieux-2011 20