PFC WG Tourniquet Conversion Recommendations
advertisement

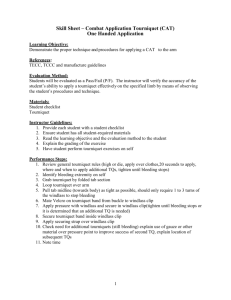
PFC WG Tourniquet Conversion Recommendations June, 2014 Background and General Notes: Tourniquets (TQs) save lives. In care under fire, liberal use of tourniquets is encouraged on all concerning extremity hemorrhage. In this phase, life-saving actions take precedence over diagnostic maneuvers. There are no documented cases of permanent tissue damage, permanent vascular injury or permanent nerve injury from a properly applied TQ (arterial flow to extremity stopped) in place for less than 2 hours. TQ conversion is the deliberate process of trying to downgrade hemorrhage control to hemostatic agents/pressure dressings. Conversion has been advocated since World War II (Wolff and Adkins 1945) and at each stage of TCC development but an up-to-date and formalized protocol has not been completed Conversion should be initiated as soon as the Care Under Fire Phase has stopped (or sooner if tactically appropriate). Conversion should be attempted with each progressive movement to the next level of care, but not for TQs that have been in place for more than 6 hours unless at a definitive care facility. Recommended procedure for TQ conversion: - Add 1 loose TQ to each extremity that already has a TQ applied (“Plus 1”). This is done for two reasons: 1-If the TQ that is already in place breaks during the conversion process, there is already a back up in place ready to be tightened. TQs carried exposed to the environment are subject to degradation based on this exposure (references below) 2-It is difficult to determine where the patient is on the resuscitation curve. Administration of fluids (crystalloids, colloids or blood) and/or ketamine has the potential to raise blood pressure beyond your hypotensive target. A second TQ in place reduces bleeding time if bleeding suddenly recurs. - With “Plus 1” in place, loosen the first TQ. If no bleeding from the wound is noted, then leave both TQs in place but not tightened and dress the wound. - If bleeding is noted, apply a hemostatic agent and hold pressure for 3-5 minutes. If no further bleeding is noted, leave the loose TQs in place and dress the wound. - If hemostatic agents fail to control the bleeding, tighten the original TQ in as distal a position as possible to control the bleeding. Leave the “Plus 1” TQ loose and proximal to the tightened TQ. FREQUENTLY ASKED QUESTIONS: How long can TQs stay on before conversion should no longer be attempted? The definitive answer to this is unknown. Most complications in the literature are a result of improper application (venous occlusion without arterial occlusion is a major concern). There is a case with documented total TQ time of up to 16 hours, but the extremity was exposed to the cold environment and the TQ was placed distally. This patient had residual motor and sensory deficits but no systemic complications of reperfusion. (Kragh, J Orthop Trauma 2007) <2 hours is considered safe (attempt conversion) 2-6 hours is likely safe (attempt conversion) >6 hours requires caution (conversion not advised in PFC) Should the TQ be loosened periodically to perfuse the distal tissues? Absolutely not. This results in “incremental exsanguination.” The patient is bled to death in short bursts. Conversion should be attempted as soon as possible and with each movement to the next level of care. References TQ Failure: Childers et al. Tourniquets exposed to the Afghanistan combat environment have decreased efficacy and increased breakage compared to unexposed tourniquets. Mil Med. 2011;176(12):1400-3. Weppner et al. Efficacy of tourniquets exposed to the Afghanistan combat environment stored in individual first aid kits versus on the exterior of plate carriers. Mil Med. 2013;178(3):334-7. Prolonged TQ Use: Kragh et al. Extended (16-hour) tourniquet application after combat wounds: a case report and review of the current literature. J Orthop Trauma. 2007;21(4):274-8. Dayan et al. Complications Associated with Prolonged Tourniquet Application on the Battlefield. Mil Med. 2008;173(1):63-66. Broad TQ Review including History/Complications/Conversion: Wolff LH, Adkins TF. Tourniquet problems in war injuries. Bulletin of the U.S. Army Medical Department 1945: 77-85. Lakstein et al. Tourniquets for hemorrhage control on the battlefield: a 4-year accumulated experience. J Trauma. 2003;54:S221-S225. Walters TJ. Issues related to the use of tourniquets on the battlefield. Mil Med. 2005;170(9):7705. Richey SL. Tourniquets for the control of traumatic hemorrhage: a review of the literature. World Journal of Emergency Surgery. 2007;2(28). Lee et al. Tourniquet use in the civilian prehospital setting. Emerg Med J. 2007;24:584-587. MacIntyre A, Quick J, Barnes S. Hemostatic dressings reduce tourniquet time while maintaining hemorrhage control. Am Surg 2011;77:152-165.