Airborne transmission

LUNG CENTER OF THE PHILIPPINES PEDIATRIC INTENSIVE CARE UNIT
ISOLATION ROOM (LCP PICU-ISOL) SPECIFICATIONS
It is recommended that the LCP PICU-ISOL be:
1.
A single patient room which will serve as an isolation room for diseases transmitted by the airborne route.
2.
A room which would utilize special ventilation (6-12 air changes per hour, air flow from surrounding area to the room, and room air exhausted directly to the outside or recirculated through a high-efficiency particulate air (HEPA) filter.
3.
A unit which would adhere to strict infection control procedures to prevent transmission of health care-associated infections.
INFECTION CONTROL FOR HOSPITALIZED CHILDREN
Health care-associated infections are a major cause of morbidity and mortality in hospitalized children, particularly children in intensive care units. Hand hygiene before and after each patient contact remains the single most important practice in prevention and control of health care-associated infections.
ISOLATION PRECAUTIONS
Isolation precautions are designed to protect hospitalized children, health-care personnel, and visitors from health care-associated infections.
Routine and optimal performance of STANDARD PRECAUTIONS is appropriate for the care of all patients regardless of their diagnosis or suspected or confirmed infection status. In addition to Standard Precautions, pathogen and syndrome-
based TRANSMISSION-BASED PRECAUTIONS are used when caring for patients who are infected or colonized with pathogens transmitted by the airborne, droplet, or contact routes.
Standard Precautions
Standard Precautions are used to prevent transmission of all infectious agents through contact with any body fluid except sweat (regardless of whether these fluids contain visible blood), nonintact skin, or mucous membranes.
Recommendations for Application of Standard Precautions for Care of All
Patients in All Health Care Settings are as follows:
Hand hygiene
Component
Personal Protective Equipment
Gloves
Gown
Recommendations
After touching blood, body fluids, secretions, excretions, or contaminated items; immediately after removing gloves; between patient contact.
Alcohol-containing antiseptic hand rubs preferred except when hands are soiled visibly with blood or other proteinaceous materials or if exposure to spores is likely to have occurred
For touching blood, body fluids, secretions, excretions, or contaminated items; for touching mucous membranes and nonintact skin
During procedures and patient-care activities when contact of clothing/exposed skin with blood/body fluids, secretions, and excretions is
Mask, goggles, face shield
Soiled patient-care equipment
Environmental Control
Textiles and laundry
Injection Practices (use of needles and other sharps)
Patient resuscitation anticipated
During procedures and patient-care activities likely to generate splashes or sprays of blood, body fluids, or secretions, especially suctioning and endotracheal intubation to protect health care personnel. For patient protection, use of a mask by the person inserting an epidural anesthesia needle or performing myelograms when prolonged exposure of the puncture site is likely to occur
Handle in a manner that prevents transfer of microorganisms to others and to the environment; wear gloves if visibly contaminated; perform hand hygiene
Develop procedures for routine care, cleaning, and disinfection of environmental surfaces, especially frequently touched surfaces in patient care areas
Handle in a manner that prevents transfer of microorganisms to others and the environment
Do not recap, bend, break, or hand manipulate used needles; if recapping is required, use a one-handed scoop technique only; place used sharps in a puncture-resistant container. Use a sterile, single-use, disposable needle and syringe for each injection given.
Single-dose medication vials are preferred when medications are administered to more than one patient
Use mouthpiece, resuscitation bag, or
Patient placement
Respiratory hygiene/cough etiquette
(source containment of infectious respiratory tract secretions in symptomatic patients) beginning at the initial point of encounter (eg, triage and reception areas in emergency department and physician offices other ventilation devices to prevent contact with mouth and oral secretions
Prioritize for single-patient room if patient is at increased risk of transmission, is likely to contaminate the environment, does not maintain appropriate hygiene, or is at increased risk of acquiring infection or developing adverse outcome following infection
Instruct symptomatic people to cover mouth/nose when sneezing/coughing; use tissues and dispose in no-touch receptacle; observe hand hygiene after soiling of hands with respiratory tract secretions; wear surgical mask if tolerated or maintain spatial separation
(more than 3 feet if possible)
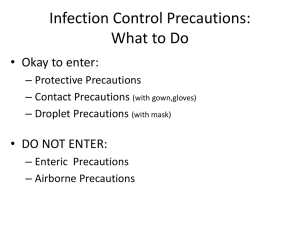
TRANSMISSION-BASED PRECAUTIONS
Transmission-Based Precautions are designed for patients documented or suspected to have colonization or infection with pathogens for which additional precautions beyond Standard Precautions are recommended to prevent transmission. The 3 types of transmission routes on which these precautions are based are airborne, droplet, and contact.
Airborne transmission
Airborne transmission occurs by dissemination of airborne droplet nuclei (< or =
5um in size) of evaporated droplets containing microorganisms that remain suspended in the air for long periods or small respirable particles containing the infectious agent or spores. Special air-handling and ventilation are required to prevent airborne transmission. Examples of microorganisms transmitted by
airborne-droplet nuclei are Mycobacterium tuberculosis, rubeola (measles) virus, and varicella-zoster virus. Specific recommendations for Airborne Precautions are as follows:
Single-patient room/Isolation Room
Use special ventilation, 6-12 air changes per hour, air flow from surrounding area to the room, and room air exhausted directly to the outside or recirculated through a high-efficiency particulate air (HEPA) filter.
If infectious pulmonary tuberculosis is suspected or proven, respiratory protective devices (personally “fitted” and “sealing” respirator, such as N95 or N100 respirators), should be worn while inside the patient’s room.
Droplet Transmission
Droplet transmission occurs when droplets containing microorganisms generated from an infected person, primarily during coughing, sneezing, or talking and during the performance of certain procedures, such as suctioning and bronchoscopy, are propelled a short distance (3 feet or less) and deposited on the conjunctivae, nasal mucosa, or mouth. Because these relatively large droplets do not remain suspended in air, special air handling and ventilation are not required to prevent droplet transmission.
Specific recommendations for Droplet Precautions are as follows:
Single-patient room if possible. If unavailable cohorting patients with the same organism is permissible. Spatial separation of more than 3 feet should be maintained between the bed of the infected patient and the beds of the other patients in multiple bed rooms. Standard precautions plus a mask should be used.
Wear a mask on entry into the room.
When performing aerosol-generating procedures (bronchoscopy, intubation, nebulizer treatment), N95 or higher respirators should be used by people in the vicinity of the patient, because small droplet nuclei may be generated by such procedures and could be transmitted to others.
Specific illnesses and infections requiring Droplet Precautions include the following:
Viral pneumonia
Diphtheria (pharyngeal)
Haemophilus influenza type b (invasive)
Influenza
Mumps
Mycoplasma pneumonia
Neisseria meningitides (invasive)
Parvovirus B19 infections (before rash onset)
Pertussis
Rhinovirus
Rubella
SARS
Group A streptococcal pharyngitis pneumonia or scarlet fever
Viral hemorrhagic fevers
CONTACT TRANSMISSION
Contact Transmission is the most common route of transmission of health careassociated infections.
Specific recommendations for Contact Precautions are as follows:
Single-patient room if possible. If unavailable, cohorting patients is permissible
Gloves (clean, nonsterile) should be used at all times
Hand hygiene should be performed after glove removal
Gowns should be used during direct contact with a patient, environmental surfaces, or items in the patient room. Gowns should be worn on entry into the room and should be removed before leaving the patient’s room or area.
Specific illnesses and infections with organisms requiring Contact Precautions:
Multidrug-resistant bacteria (vancomycin-resistant enterococci; MRSA, multidrugresistant gram-negative bacilli) or other epidemiologically important susceptible bacteria
C difficile
Conjunctivitis, viral and hemorrhagic
Diphtheria (cutaneous)
Enteroviruses
E. coli O157:H7 and other Shiga toxin-producing E. coli
Hepatitis A virus
Herpes simplex virus (neonatal, mucocutaneous, or cutaneous
Herpes zoster (local)
Impetigo
Major abscess, cellulitis, or decubitus ulcer
Parainfluenza virus
Pediculosis (lice)
Respiratory syncitial virus
Rotavirus
Salmonella
Scabies
Shigella
S. aureus (cutaneous or draining wounds)
Viral hemorrhagic fevers
Summary of Transmission-Based Precautions for Hospitalized Patients to
Prevent Health care-associated Infections
Category of
Precautions
Airborne
Single-Patient
Room
Yes, with negative airpressure
Respiratory
Tract/Mucous
Membrane
Protection
N95 respirator or higher lever
Gowns
No*
Gloves
No*
Droplet ventilation, 6-
12 air exchanges per hour, +/- HEPA filtration
Yes
Yes
Surgical masks
(upon entry into room)
No
No*
Yes
No*
Contact Yes
* Gowns and gloves may be required as a component of Standard Precautions