NORMAL CAROTID and scanning technique
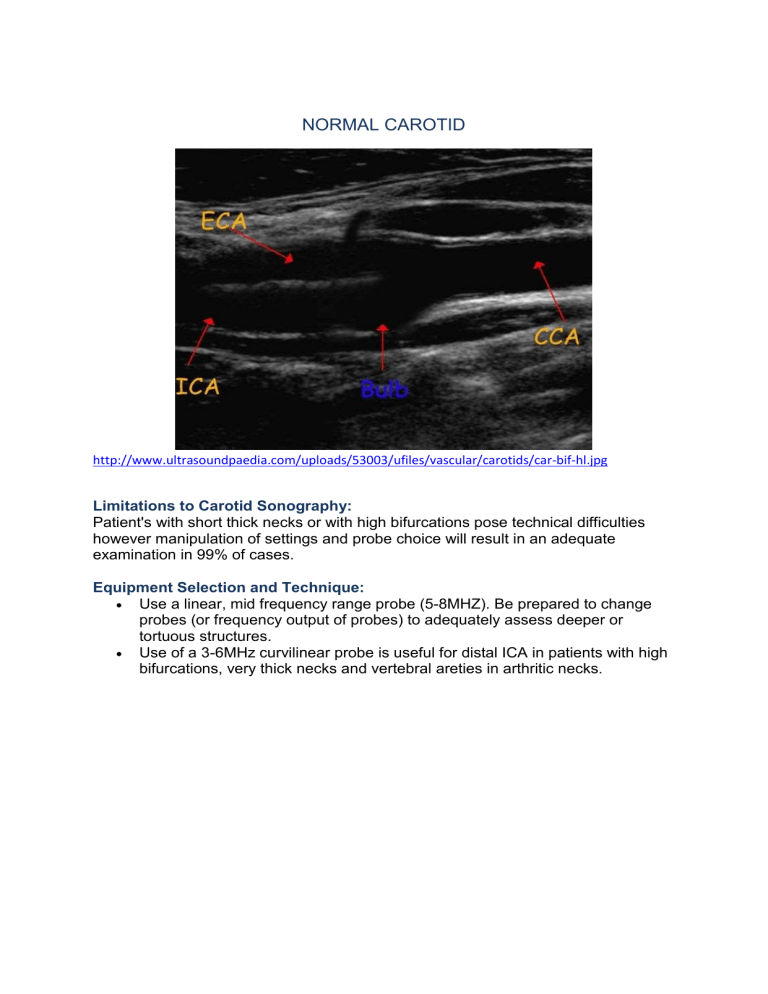
NORMAL CAROTID
http://www.ultrasoundpaedia.com/uploads/53003/ufiles/vascular/carotids/car-bif-hl.jpg
Limitations to Carotid Sonography:
Patient's with short thick necks or with high bifurcations pose technical difficulties however manipulation of settings and probe choice will result in an adequate examination in 99% of cases.
Equipment Selection and Technique:
Use a linear, mid frequency range probe (5-8MHZ). Be prepared to change probes (or frequency output of probes) to adequately assess deeper or tortuous structures.
Use of a 3-6MHz curvilinear probe is useful for distal ICA in patients with high bifurcations, very thick necks and vertebral areties in arthritic necks .
Normal Common Carotid artery (CCA). Note the smooth echogenic intimal surface. http://www.ultrasoundpaedia.com/normal-carotids/
Scanning Technique
https://lms.curtin.edu.au/bbcswebdav/pid-1033599-dt-content-rid-9049991_1/courses/310696-
FacSciEng-1729436055/Module%20Three%20-%20Carotid%20Doppler%202013.pdf
The examination is undertaken with the patient lying supine with their neck extended as much as reasonably comfortable.
A careful history is taken noting any previous examinations, surgery, and relevant symptoms.
It is usual to begin the examination with the same side, eg the right side. The patients head may need to be slightly rotated towards the left. All of the right side is examined and then the head is slightly rotated to the right for optimal imaging of the left carotid vessels.
Using B-mode the innominate (BCA) and subclavian arteries are examined noting any build-up of plaque, calcification etc
And the degree of tortuosity of any of the vessels noted particularly important prior to endarterectomy surgery.
The CCA is then examined proximal to distal in longitudinal and transverse images.
Begin proximally in transverse and follow distally to the bifurcation.
Assess the course (i.e. if tortuous) and the presence of any intimal thickening or plaque.
Repeat in longitudinal plane.
Use colour to assess patency of vessel and the direction of flow.
Use 'Heel/Toe' technique to optimize insonation of vessel, apply colour box and Doppler sample gate with appropriate steering and angle correction.
Measure the Peak Systolic (PSV) and end diastolic velocities (EDV).
The CCA will have a doppler trace that is representative of both upstream and down stream influences. Any cardiac arhythmia or significant left heart valvular problems may be relected in the wave form (eg via a audible and visible 'flutter'). Similarly, the CCA waveform is a combination of both
ICA and ECA waveforms.
http://www.ultrasoundpaedia.com/normal-carotids/
A false impression of intimal thickening may occur with oblique images.
The bifurcation of the common carotid artery into the internal (ICA) and external carotid arteries (ECA) is examined with attention to the bifurcation and the proximal internal carotid artery and external carotid arteries.
Assess in transverse and longitudinal for pathology.
http://www.ultrasoundpaedia.com/normal-carotids/
(The ECA also usually has a smaller diameter, arises laterally and has a higher resistance waveform (ie lower diastolic flow than a normal ICA).
'Temporal Tapping' may also be used to confirm that you are examining the ECA.
This involves gently tapping the temporal artery (approximately 1-2cm anterior to the top of the ear) whilst sampling the ECA with doppler. You will see reverberations in the trace corresponding to your tapping.)
A normal ICA will have no branches and usually a lower resistance waveform.
Measure the Peak Systolic (PSV) and end diastolic velocities (EDV) of the
ECA.
Unless the vessel is tortuous, you should see a low resistance waveform with a clean spectral window beneath the trace
http://www.ultrasoundpaedia.com/normal-carotids/
The proximal portion of the external carotid artery is examined; you may need to move to a more anterior position to image the external carotid artery. The external carotid artery is then followed as far as possible.
The internal carotid artery is then imaged as far as possible towards the distal portion as it enters the cranium, in longitudinal and transverse positions, altering the transducer position from anterior to oblique and posterolateral gaining the optimal ultrasonic window.
Look for stenoses highlighted by aliasing in the colour doppler.
Take Doppler samples in the proximal and distal segments and anywhere else that pathology or an altered waveform is detected.
Ensure you angle correctly to the direction of the flow indicated by the colour doppler prior to calculating velocity. IMPORTANTLY, this angle may not correspond to the course of the vessel.
The distal internal carotid artery is often optimally seen from a posterolateral view with the patients head turned as far as possible to the contralateral side.
The transducer is then moved down to the innominate (BCA) and colour and spectral Doppler are used to assess the spectral waveform, including peak velocity, and colour filling of the vessels.
Beginning with the subclavian and innominate (BCA), then the common carotid artery proximal, due to the sometimes deep position of these vessels optimal colour filling is often optimised by using a straight colour box and similar optimisation of the spectral waveforms using an angle closer to 60◦.
The common carotid artery is followed to the bifurcation, careful note is made of the colour flow at the bifurcation, some turbulence here is normal.
The proximal external carotid artery is examined noting the presence of branches and the size of the vessel (usually of a smaller calibre then the internal carotid artery), good colour filling and a normal high resistance waveform are noted.
If there is any difficulty in differentiating between the external and internal carotid vessels, usually the more anterior position, vessel size and the presence of branches allow for easy differentiation.
Another method is to place the spectral Doppler in the suspected external carotid artery and to gently tap the temporal artery, find the temporal bone just superior to the zygoma and inferior to the orbit, and gently tap, a change in the waveform correspon ding to the ‘tap’ enables accurate identification of the external carotid artery.
The external carotid artery is examined as far as possible with colour flow and any areas of change in velocity are examined using spectral Doppler.
The internal carotid artery is then examined from the bifurcation as far distally as possible using the ultrasound windows previously mentioned. A normal low resistance waveform is seen along the vessel with good colour filling.
A note is made of the tortuosities of any vessels, any increase in velocity and the level of bifurcation of the common carotid artery.
The vertebral artery is examined with the chin extended and the transducer placed to optimally see the artery coursing between the transverse foramen.
Moving slowly posterior from a longitudinal section of the common carotid or internal carotid artery is usually successful or identifying the vertebral vein which is usually superior to the artery and of a larger calibre may help. Colour filling and a spectral trace of the vertebral artery to identify any increase in velocity and the direction of flow.
Ensure suitable PRF and gain for these smaller, deeper vessels. The flow should be low resistance flow ( presence of forward diastolic flow).
Confirm the flow is antegrade i.e. towards the head - (normal) or retrograde (suggesting subclavian steal syndrome). http://www.ultrasoundpaedia.com/normal-carotids/
The vertebral artery is also examined with the patients head and neck in different positions, extended flexed etc if there is reason to suspect any positional alteration of the vertebral artery flow.
Adjacent Structures:
It is important to be aware of surrounding anatomy in the neck that may be of clinical significance. An example can be enlarged lymph nodes or thyroid pathology. Brief documentation may be made and formal follow up studies can be performed if clinically indicated.
A routine examination of the carotid vessels must contain at least the following images.
B-mode images demonstrating the innominate (brachiocephalic), subclavian and proximal common carotid arteries (right) and proximal common carotid artery (left).
It is often possible to obtain one image demonstrating all three vessels.
Longitudinal and transverse B- mode images of the proximal and distal common carotid artery.
A longitudinal image of the bifurcation of the common carotid artery and the external and internal carotid arteries, if it is not possible to view all three vessels at once at least an image demonstrating the distal common carotid and the proximal internal carotid arteries with a transverse image demonstrating the bifurcation.
Longitudinal image documenting the mid internal carotid artery.
Colour Doppler images of the innominate (BCA), subclavian and proximal common carotid (right) and proximal common carotid (left). A spectral trace in the common carotid artery proximal and distal (at approximately 2cm inferior to the bifurcation).
Colour Doppler image of the bifurcation (demonstrating the distal common carotid and proximal internal carotid arteries.
A spectral waveform in the proximal external carotid artery (preferably not too close to a branch) and proximal mid and distal internal carotid artery.
A spectral waveform in the vertebral artery.
Right and left carotid and vertebral arteries are always examined.