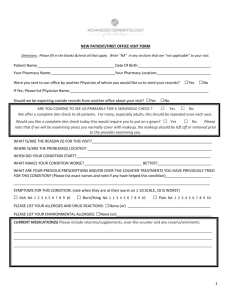
khiem vu, do pa
advertisement

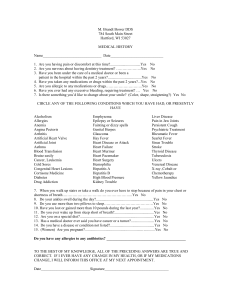
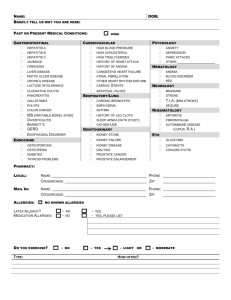
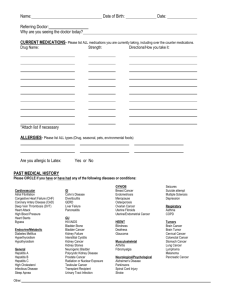
KHIEM VU, DO PA ADULT HEALTH HISTORY FORM NAME: ______________________________________________________ DOB: _______________________ AGE: _____________ PAST MEDICAL HISTORY: Select all that are applicable. Fill in others that are not listed. ADD or ADHD Allergy Testing Y/N Panic Attacks Y/N Injection Therapy Y/N Asthma Attacks per Month Atrial Fibrillation Cardioversion Y/N How Many Years Nebulizer at Home Y/N Anticoagulation Y/N Allergies Anxiety Bronchitis Cancer (Brain / Bone / Breasts / Colon / Lungs / Prostate / Skin) Cerebral Vascular Attack (Stroke or TIA) Remission / Cured Chemo / Radiation / Surgery Oncologist: Deficits Chronic Pain COPD Last Spirometry Last Stress Test Date Home Oxygen Y/N Stress Test Result Coronary Arterial Disease Treatment Diabetes Mellitus Type I / II Diagnosed Date Insulin Oral Medications GERD (reflux) Peptic Ulcer Y/N Endoscopy Date Headache (Cluster / Migraine / Tension) Headaches per Month Heart Failure EF if known Implanted Defibrillator Y/N Controlled Y/N Endoscopy Date Colonoscopy Date Stenting: # of Vessels Cardiologist: Valve Replaced Aortic / Mitral Valve type: Prosthetic /Mechanical Hemorrhoids (External / Internal) Inflammatory Bowel Disease (Crohn’s / Ulcerative Colitis) Kidney Disease Dialysis Y/N Kidney Stones Myocardial Infarction (Heart Attack) Osteoarthritis Bypass Surgery # of Vessels Joint (s) Affected Pacemaker Implanted Rheumatoid Arthritis Joint (s) Affected Skin Disease (Psoriasis / Rash ) Tremor Etiology ? Valvular Replacement Date Replaced Other Other Other Other PREVIOUS SURGERIES: Year Surgery Hospital FAMILY HISTORY: Has any of your family member(s) ever had any of the following conditions? Disease Father Mother Sibling Other Alzheimer Anemia: Pernicious / Thalassemia / Iron Asthma Cancer: Brain / Breasts / Colon / Cervical / Lungs / Lymphoma / Prostate / Skin COPD Cerebral Vascular Accident Diabetes Type I / II High Blood Pressure High Cholesterol Kidney Problems requiring Dialysis Gastrointestinal : Crohn’s / Ulcerative Colitis / Peptic Ulcer / Polyps Liver Disease: Hepatitis / Cirrhosis Osteoarthritis Rheumatoid Arthritis Skin Problems: Psoriasis / Rash SOCIAL HISTORY: Occupation: ______________________ Employer : ________________If Retired, Prior Occupation: ________________ Tobacco Use? N Y If yes, what? ________________ How much? _______________ How long? __________ *If you had a history of tobacco use, but quit, please give quit date: __________________________________________ Alcohol Use? N Y If yes, what? ________________ How much? _______________ How long? __________ Illegal Drug Use? N Y If yes, what? ________________ How much? _______________ How long? __________ Marital Status: Single Engaged Are you sexually active? N Y Married Do you exercise? N Y Y Separated Current sex partner(s)? Male Have you ever had a sexually transmitted disease? N Do you have children? N Widowed Y Divorced Female Birth Control Method: _____________________ If yes, how many? __________________ If yes, how frequently? ___________________ HEALTH MAINTENANCE & SCREENING TEST: DATE NORMAL ABNORMAL NEXT SCHEDULED Bone Density Colonoscopy Pap Smear (female) Mammogram (female) Prostate (male) Digital Rectal Exam IMMUNIZATIONS & TESTS: What vaccinations have you received in the past? Hepatitis A Hepatitis B Meningococcal Positive TB skin test? No Flu Shot MMR Tetanus (TD or Tdap) Pneumonia Shot Shingles Shot Chicken Pox Yes Chest X-ray Result: Normal Abnormal If Abnormal, treated? Polio No Yes ALLERGIES: List any allergies to medications and/or foods. Do you have an Advance Directive? N Y ** If yes, please provide a copy for your chart. Do you have an appointed Power of Attorney or Medical Power of Attorney? N Y ** If yes, please provide a copy for your chart. CURRENT MEDICATIONS: Name *Please use additional form if necessary. Dose/Strength Frequency CURRENT MEDICATIONS: Name Dose/Strength Frequency