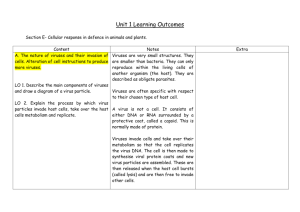
Physiology Ch. 34 p433-444 [4-25
advertisement

Physiology Ch. 34 p433-444 Resistance of the Body to Infection: Immunity and Allergy Human body can resist most types of organisms and toxins that damage tissues, capability is called immunity Acquired Immunity – does not develop until after body is first attacked by a bacterium, virus, or toxin, and can take weeks or months to develop this immunity Innate Immunity – a more general process not specific for certain organisms, and includes: 1. Phagocytosis of bacteria by WBC and tissue macrophage system 2. Destruction of swallowed organisms by stomach acids 3. Resistance of skin to invasion 4. Presence of chemicals in blood that attach to foreign organisms and destroy them a. Lysozyme, b. Polypeptides c. Complement complex d. Natural killer lymphocytes -innate immunity helps make body resistant to diseases such as paralytic viral infections Acquired (Adaptive) Immunity – specific immunity against individual pathogenic agents such as lethal bacteria, viruses, toxins, and other animals, and is caused by system that forms antibodies and activated lymphocytes that attack and destroy the specific invading organism Basic Types of Acquired Immunity – Humoral and Cell-Mediated – body creates two types of immunity 1. Humoral Immunity – circulating antibodies produced by B-lymphocytes 2. Cell-Mediated Immunity – T-cell immunity where active T-lymphocytes targeting 1 agent -antigens initiate both types of immunity, and are proteins or large polysaccharides that the body recognizes as different from their own -for substance to be antigenic, it must have high molecular weight of 8000 or more, and antigenicity requires certain regularly occurring groups called epitopes on the surface of the molecule Lymphocytes Responsible for Acquired Immunity – people with lack of lymphocytes cannot mount an acquired immune response -lymphocytes located mainly in lymph nodes but also found in spleen, GI tract, thymus and marrow -invading agent first enters tissue fluids and is then carried by lymph to lymph nodes or lymphoid tissue T and B Lymphocytes Promote Acquired Immunity -T-lymphocytes provide cell-mediated immunity and B lymphocytes provide humoral immunity -both are derived from pluripotent hematopoietic stem cells that form common lymphoid progenitor cells as they differentiate -lymphoid progenitor cells that become T lymphocytes migrate to thymus -B-lymphocytes are pre-processed in the liver during mid-fetal life and in bone marrow in late fetal life and after birth (called B lymphocytes after a bird organ called bursa of fabricius Preprocessing of T and B Lymphocytes – all lymphocytes come from lymphocyte-committed stem cells in embryo which cannot directly form active T or B cells and must further differentiate Thymus Gland Preprocesses T Lymphocytes – After origination in bone marrow, T cells migrate to thymus, divide rapidly, and develop specific reactivity to one antigen. The next lymphocyte develops specific reactivity against another antigen until thousands of T cells exist which leave thymus and spread throughout body in lymphoid tissue -Thymus also makes certain any T lymphocytes will not autoreact against body’s own proteins by mixing T cell with all specific self-antigens from body’s own tissues, and if it reacts, the T cell is destroyed and phagocytized and not released -happens to 90% of all T cells, and only those non-autoreactive will be released into the blood -most preprocessing occurs before birth and for a little while after birth, after which removal of thymus gland does not diminish T cell immune system. -if thymus is removed beforehand, T cell immune system does not function Liver and Bone Marrow Preprocess B Lymphocytes – B cells preprocessed in liver during mid-fetal life and in bone marrow during late fetal life and after birth -B lymphocytes actively secrete antibodies that are reactive protein molecules capable of combining and destroying antigenic substance -B lymphocytes have greater diversity than T lymphocytes by forming millions of antibodies with different reactivities -B cells migrate to lymphoid tissue around body and attach near to, but removed from T cells T Lymphocytes and B-Lymphocyte Antibodies React Highly Specifically against Specific Antigens-specific antigens will come in contact with B cells to cause them to produce antibodies against that particular antigen, and T cells to form activated T cells Millions of Specific Types of Lymphocytes are Stored in Lymphoid Tissue – preformed B and T cells can form highly specific types of antibodies or T cells and are stored in lymph tissue -Only the specific type of antigen to specific T or B cell can activate it -Once lymphocyte is activated, it reproduces wildly, forming lots of duplicates, and if B cell, will make and secrete specific antibody that then circulates throughout the body -if a T lymphocyte sees antigen, its progeny will be released into lymph and carried to blood and circulate through all tissue fluids and back to lymph, sometimes circulating for years -all the different cells capable of forming one specific antibody or T cell are called clones of lymphocytes Origin of Clones of Lymphocytes – only 100-1000 genes code for millions of different antibodies and T cells -hundreds of gene segments for these antibodies are mixed during preprocessing in random combinations to form different, whole genes; millions of combinations can be formed in single cells Mechanism for Activating a Clone of Lymphocytes – each clone of lymphocytes is responsive to a single antigen -B cells have 100,000 antibody molecules on their surfaces that will react with only one antigen, and when it does come along, it attaches to antibody on cell membrane and leads to activation -T cells have surface receptor proteins on their surface that are highly specific for antigens that will activate only those cells that have complementary receptors for that antigen Role of Macrophages in Activation Process – macrophages are present in addition to lymphocytes in the tissue. Most organisms are first phagocytized and digested by macrophages, and the antigenic products are released into macrophage cytosol -macrophages pass antigens by cell-to-cell contact to lymphocytes to generate activation of clones -macrophages also secrete IL-1, which further promotes growth and reproduction of lymphocytes Role of T cells in Activation of B cells – most antigens activate both T cells and B cells at the same time -some of the T cells that are formed, T Helper Cells, secrete lymphokines that can activate specific B cells. -without help from helper cells, amount of antibodies formed from B cells is only slight Specific Attributes of B-lymphocyte System – Humoral Immunity and Antibodies -clones of B cells lie dormant in lymphoid tissue before exposure to antigen -macrophages come in contact with antigen, phagocytize it, and present it to adjacent B cells -antigens are also presented to T cells to form T helper cells -B cells specific for that antigen enlarge and appear like lymphoblasts which further differentiate into plasmablasts (precursors to plasma cells) -plasmablast cytoplasm expands and rough ER proliferates begin to divide once/10 hours for 9 divisions, giving 500 cells in 4 days that produce Ig antibodies at 2000 molecules/s/cell, which are secreted into the lymph and carried into blood Formation of Memory Cells (primary vs secondary response) – a few lymphoblasts formed from activation of B cells do not form plasma cells but instead form low numbers of new B cells similar to original clone that circulate in the blood and lodge in tissues, but do not become activated until new antigen comes along later -primary response forms a lower amount of antibody than a secondary response -after 1 week the same antigen is injected and a huge response is seen, indicated that preformed memory B cells were created after the first response, explains immunizations Antibodies – gamma globulins called immunoglobulins constitute 20% of all plasma proteins -composed of light and heavy chains and are a combination of two light and two heavy chains -some could be combination of 10 light and 10 heavy chains, but each heavy chain is paralleled by a light chain to form heavy-light pair -the end of each light and heavy chain is called the variable portion while the remainder is constant portion -variable portion is different for each antibody and is part that attaches to the antigen -constant portion determines other properties such as diffusivity of antibody in tissues, adherence of antibody to specific structures, attachment to complement complex, Specificity of Antibodies – unique structural organization of antibody makes it specific for particular antigen in the variable regions -multiple prosthetic groups of antigen fit as mirror image with those on antibody to allow tight binding -when antibody is highly specific, there are many bonding sites that the antibody-antigen coupling is strong and held together by: hydrophobic bonding, H+ bonding, ionic interactions, and van der Waals Ka = [bound antibody-antigen] / ([antibody][antigen]) ::: (Ka is affinity constant and measure of how tightly antibody binds with antigen) -antibody with two variable sites can bind 2 antigens, making it bivalent Classes of Antibodies – five general classes: IgG, IgM, IgA, IgD, and IgE -Ig stands for immunoglobulin, while the letter after stands for the respective class -IgG is bivalent antibody and constitutes 75% of antibodies in a normal person -IgE is especially involved in allergy -IgM class of antibodies are formed during the primary response, and have 10 binding sites Mechanism of Action of Antibodies – antibodies act by either direct attack on invader or activation of the complement system that then has many ways of destroying the invader Direct Action of Antibodies – antibodies inactivate the invading antigens in these ways: 1. Agglutination – multiple large particles with antigens on surface are bound in a clump 2. Precipitation – molecular complex of soluble antigen and antibody becomes so large that it is rendered insoluble precipitate 3. Neutralization – antibodies cover toxic sites of antigenic agent 4. Lysis – some potent antibodies are occasionally able to directly attack membranes of cellular agents to cause rupture -these are often not strong enough to play a major role in protection, complement does Complement System of Antibody Action – complement is system of 20 proteins which are enzyme precursors, the major ones are 11 proteins designated C1 through C9, B and D -all of these proteins are present in the blood as well as in tissue spaces after leaking out -normally inactive, but can be activated by the classic pathway Classic Pathway of Complement Activation – initiated by antibody-antigen reaction, when specific reactive site in the constant region becomes uncovered and binds with C1 of the complement system to set off the cascade **DRAWING OF CASCADE IS ON SEPARATE PAPER -C1 sets of cascade that activates other enzymes in the later stages of the system so that a small beginning can form a large amplified reaction where multiple end products are formed to help prevent damage to body’s tissues by invading organism. These are: 1. Opsonization and Phagocytosis – one of the products of complement system, C3b, activates phagocytosis by neutrophils and macrophages causing them to engulf bacteria to which antibody is attached, called opsonization 2. Lysis – most important of all complement products (combination of many factors) is C5b6789, which has a direct effect of rupturing cell membranes of bacteria 3. Agglutination – complement products also change surfaces of invading organisms to cause them to adhere to one another 4. Neutralization of Viruses – complement enzymes can attack viruses and make them nonvirulent 5. Chemotaxis – fragment C5a initiates chemotaxis of neutrophils and macrophages to cause them to migrate to tissue area adjacent to antigenic target 6. Activation of mast cells and basophils – fragments C3a, C4a, and C5a activate mast cells and basophils to make them release histamine, heparin and other substances into local fluids a. These cause increased blood flow, increased leakage of fluid/plasma into tissue and help to inactivate or immobilize antigenic agent 7. Inflammatory Effects – several other complement factors contribute to local inflammation to cause increased blood flow, capillary leakage of proteins, and coagulation of interstitial fluids Specific Attributes of T Cell System- Activated T cells and Cell-Mediated Immunity – on exposure to antigen, as presented by macrophages, T cells of specific clone proliferate and release activated, reacting T cells into the lymph circulation and distributed to body -T lymphocyte memory cells are formed in same way as B memory cells, where som T cells are preserved and not activated upon activation of the rest so that the next time an antigen is exposed, a more rapid response is seen Antigen-Presenting Cells, MHC Proteins, and Antigen Receptors – T-cell responses are very antigenspecific, and they play a major role in helping eliminate invading pathogens -T cells respond to antigens ONLY when they are bound to MHC proteins on surface of antigen presenting cells in lymphoid tissues -three types of APCs are macrophages, B cells, and dendritic cells -dendritic cells are most potent APCs and are located throughout the body – their only known function is to present antigens to T cells -MHC proteins encoded by genes called major histocompatibility complex -MHC proteins bind peptide fragments of antigen proteins that are degraded inside APCs and transport them to cell surface -Two types of MHC proteins: 1. MHC I Proteins – present antigens to cytotoxic T cells 2. MHC II Proteins – present antigens to T helper cells -APC antigens on MHC bind receptors on surface of T cells that have a variable region specific for that antigen, and there are up to 100,000 receptor sites on T cell -There are three classes of T cells: Helper T cells, Cytotoxic T cells, and Suppressor T cells Helper T cells Regulate Overall Immunity – helper T cells are most numerous and help in regulating all immune functions by forming series of protein mediators called lymphokines that act on other cells of immune system as well as bone marrow, the important ones released are: -IL2, IL3, IL4, IL5, IL6, Granulocyte-monocyte colony stimulating factor, interferon-γ Specific Regulatory Functions of Lymphokines – in absence of lymphokines, remainder of immune system is almost paralyzed, such as is the case with the AIDS virus which leaves the body unprotected to infectious disease Stimulation of Growth and Proliferation of Cytotoxic and Suppressor T cells – the lymphokine IL-2 has a strong stimulatory effect in causing growth and proliferation of both cytotoxic and suppressor T cells Stimulation of B-cell Growth and Differentiation to Form Plasma Cells and Antibodies – almost all interleukins are involved in B-cell response, but especially IL-4, IL-5, and IL-6 have super strong effects on stimulating B cell growth Activation of Macrophage System – lymphokines also affect macrophages by slowing or stopping their migration after they have been chemotactically attracted into inflamed area to cause accumulation -lymphokines also activate macrophages to cause more effective phagocytosis Feedback Stimulatory Effect on Helper Cells Themselves – some lymphokines like IL-2 have direct positive feedback effect in stimulating activation of more helper T cells to amplify their response Cytotoxic T Cells are “Killer” Cells – cytotoxic T cell is direct-attack cell that kills microorganisms and some of the body’s own cells -receptors of these cells bind to organisms or cells that contain the appropriate binding-specific antigen and then kill the cell by way of: -Cytotoxic T cells secrete perforins, which are proteins that form holes in target membrane of attacked cell. -Fluid rushes into the cell from interstitial space, and cytotoxic T cell also releases cytotoxic substances directly into the attacked cell, which becomes swollen and dissolves -Cytotoxic T cells can pull away from victim cells after punching holes and move on to kill more cells -These cells can be lethal to tissue cells infected with viruses because virus particles can be entrapped in membranes of tissue cells that attract T cells in response to viral antigenicity -Cytotoxic T cells can also kill cancer cells, heart transplant cells or other foreign cells Suppressor T Cells – capable of suppressing functions of both cytotoxic and helper T cells and can prevent cytotoxic T cells from causing excessive immune reactions that can be damaging to body, so these suppressor T cells can also be called regulatory T cells Tolerance of Acquired Immune System to One’s Own Tissues (Role of Preprocessing) – most tolerance results from preprocessing of T lymphocytes in thymus and B lymphocytes in bone marrow -during preprocessing, all or most of clones that are specific to damage of own body tissues are destroyed by either Thymus for T cells or bone marrow for B cells Failure of Tolerance mechanism Causes Autoimmune Diseases – sometimes people lose immune tolerance of their own tissues, most often in older individuals after destruction of person’s own tissues which release self-antigens that circulate and cause acquired immunity by activated T cells or antibodies -Specific diseases result from autoimmunity such as: -Rheumatic fever – body becomes immunized against tissues in joints and heart valves after exposure to specific type of streptococcal toxin that has an epitope in its structure similar to body’s own proteins -Glomerulonephritis – person becomes immunized against basement membranes of glomeruli -Myasthenia Gravis – immunity develops against acetylcholine receptor of neuromuscular junction and causes paralysis -Lupus Erythematosus – person becomes immunized against many body tissues at same time which can cause damage and death Immunization by Injection of Antigens – immunization produces acquired immunity against specific diseases by injecting dead or inactive organisms that can no longer cause disease but still have some chemical antigens. Examples are typhoid fever, whooping cough, diphtheria, and other bacterial diseases -person can be immunized by being infected with live organisms that have been attenuated, or grown in special media so that they have been mutated enough so as to not cause disease but still carry antigen for immunization, such as smallpox, yellow fever, polio, measles Passive Immunity – temporary immunity achieved without any antigen exposure by fusing antibodies, activated T cells, or both obtained from blood of someone else or from animal that has been actively immunized against the antigen -these antibodies last for 2-3 weeks in the body while person becomes protected from disease -activated T cells will last for few weeks if from person, but only few hours if from animal -such transfer of antibodies or T cells is called passive immunity Allergy and Hypersensitivity – an undesirable effect of immunity is development of conditions of allergy or other types of immune hypersensitivity Allergy Caused by Activated T Cells – delayed-reaction allergy is caused by active T cells and not antibodies, such as is the case with poison ivy, where repeated exposure can cause formation of activated helper and cytotoxic T cells -after subsequent exposure to poison ivy toxin, activated T cells diffuse from circulation into the skin to respond to the toxin and elicit cell-mediated immune reaction to release many toxic substances from T cells and extensive invasion of tissue by macrophages -can happen in the skin such as poison ivy, or in the lungs to cause lung edema or asthmatic attacks in the case of airborne antigens Allergies in “Allergic” Person with Excess IgE Antibodies – some people have allergic tendency, and their allergies are called atopic allergies because they are caused by a nonordinary response of immune system -passed genetically from parent to child and is characterized by presence of large quantities of IgE antibodies in the blood -IgE antibodies are called reagins or sensitizing antibodies to distinguish them from IgE -IgE antibodies attract mast cells and basophils, which can each bind half a million IgE antibodies -when an antigen (allergen) binds multiple IgE antibodies that are already attached to mast cell or basophil, it causes change in membrane that cause many mast cells/basophils to rupture -other mast cells/basophils release histamine, protease, slow-reacting substance of anaphylaxis, eosinophil chemotactic substance, neutrophil chemotactic substance, heparin, and platelet activating factors -these substances cause vasodilation, attraction of eosinophils and neutrophils, leaky capillaries, contraction of smooth muscle Anaphylaxis – Injected allergen can react with basophils in blood and mast cells in tissues if they have been sensitized by IgE attachment, which can cause widespread allergic reaction throughout vascular system and related tissues (anaphylaxis). -Histamine is released into circulation and causes body-wide vasodilation and leaky vessels resulting in loss of plasma from circulation -person suffering can die of circulatory shock within a few minutes unless treated with epinephrine to oppose effects of histamine -also released form mast cells/basophils is slow-reacting substance of anaphylaxis – which cause spasm of smooth muscle in bronchioles to elicit asthma-like attack which can cause death by suffocation Urticaria – results from antigen entering specific skin areas and causing localized anaphylactoid reaction -histamine released locally causes vasodilation (red flare of skin) and increased permeability of capillaries that leads to local circumscribed areas of swelling of skin (Hives) -treat with antihistamine drugs before exposure to prevent hives Hay Fever – allergen-reagin (IgE) reaction occurs in the nose, and histamine is released in response to reaction to cause local intranasal vascular dilation and increased capillary pressure/permeability. This causes rapid fluid leakage into the nose and deeper tissues, and nasal linings swell and become secretory -antihistamine drugs can prevent swelling -other products of allergen-IgE can cause sneezing Asthma – allergen-IgE is in bronchioles where slow-reacting substance of anaphylaxis is released to cause bronchiolar smooth muscle contraction and difficulty breathing. Administer antihistamine