docx ~115kb
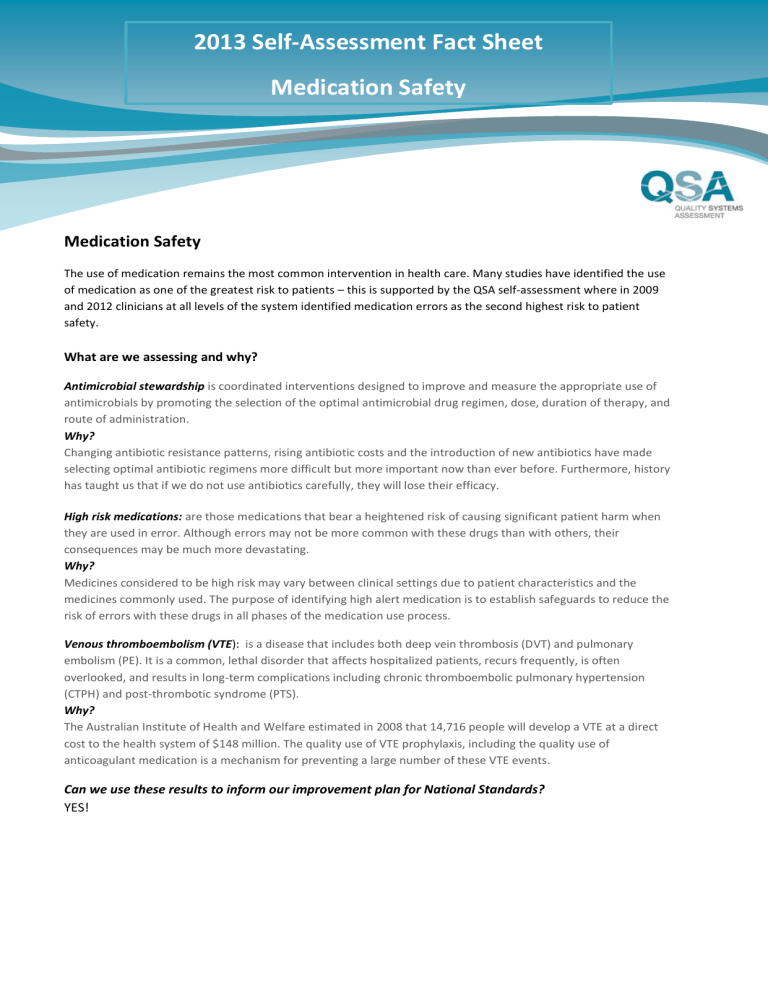
2013 Self-Assessment Fact Sheet
Question context – Medication Safety
2013 Self-Assessment Fact Sheet
Medication Safety
Medication Safety
The use of medication remains the most common intervention in health care. Many studies have identified the use of medication as one of the greatest risk to patients – this is supported by the QSA self-assessment where in 2009 and 2012 clinicians at all levels of the system identified medication errors as the second highest risk to patient safety.
What are we assessing and why?
Antimicrobial stewardship is coordinated interventions designed to improve and measure the appropriate use of antimicrobials by promoting the selection of the optimal antimicrobial drug regimen, dose, duration of therapy, and route of administration.
Why?
Changing antibiotic resistance patterns, rising antibiotic costs and the introduction of new antibiotics have made selecting optimal antibiotic regimens more difficult but more important now than ever before. Furthermore, history has taught us that if we do not use antibiotics carefully, they will lose their efficacy.
High risk medications: are those medications that bear a heightened risk of causing significant patient harm when they are used in error. Although errors may not be more common with these drugs than with others, their consequences may be much more devastating.
Why?
Medicines considered to be high risk may vary between clinical settings due to patient characteristics and the medicines commonly used. The purpose of identifying high alert medication is to establish safeguards to reduce the risk of errors with these drugs in all phases of the medication use process.
Venous thromboembolism (VTE): is a disease that includes both deep vein thrombosis (DVT) and pulmonary embolism (PE). It is a common, lethal disorder that affects hospitalized patients, recurs frequently, is often overlooked, and results in long-term complications including chronic thromboembolic pulmonary hypertension
(CTPH) and post-thrombotic syndrome (PTS).
Why?
The Australian Institute of Health and Welfare estimated in 2008 that 14,716 people will develop a VTE at a direct cost to the health system of $148 million. The quality use of VTE prophylaxis, including the quality use of anticoagulant medication is a mechanism for preventing a large number of these VTE events.
Can we use these results to inform our improvement plan for National Standards?
YES!
2013 Self-Assessment Fact Sheet
Question context – Falls
2013 Self-Assessment Fact Sheet
Falls
Falls
In NSW falls are the single highest injury cost including road trauma. They cost the health system in excess of $500 million per year and are a major contributor to loss of function and reduced quality of life for older people. In both
2009 and 2012 clinicians at all levels of the system completing the QSA self-assessment identified falls as the major risk to patient safety.
What are we assessing and why?
Policy and guidelines for risk assessment
Research indicates that multidisciplinary approaches encompassing comprehensive identification of falls risks, assessment and targeted intervention can reduce falls and fall injury rates. Falls prevention should be integrated into the culture of an organisation, thus providing management and clinicians with a strategic direction for improving the safety and quality of patients and reduce patient falls risks in health care.
Medication review
Medications have commonly been identified as a significant risk factor for falls. The most commonly cited medications that increase the risk of the patient falling are those that act on the central nervous system, such as the sedatives and tranquillisers, benzodiazepines and patients receiving psychoactive drugs.
Education
Provision of information, instruction and training is an effective means of ensuring that all staff have, at least, minimal competence in falls prevention and management activities and are committed and engaged in strategies to improve the safety and quality of health care at the local level.
Post fall admission referral
Other risk factors may be acquired as part of the events of the admission; for example, gait changes or dizziness.
Falls risk is increased for one month after discharge from hospital. Some risk factors for falls (eg certain medications) can be managed during admission. However, some falls risk factors (eg muscle weakness, poor nutrition) require longer term interventions. An exercise program can be started during admission, but needs to continue for some weeks after discharge to achieve optimal muscle strength.
Patient and family
Why?
Consumer participation in health is central to high-quality and accountable health services. It also encourages shared responsibility in health care.
Can we use these results to inform our improvement plan for National Standards?
YES!
2013 Self-Assessment Fact Sheet
Question context – Transfer of Care
2013 Self-Assessment Fact Sheet
Transition of Care
Transition of Care
Transition of care refers to the movement patients make between health care practitioners and settings as their condition and care needs change during the course of a chronic or acute illness 1 . Transitions can occur:
Within health settings like ICU to radiology
Between settings
Up transfer: Transfer to another hospital for inpatient specialist treatment not available at present location
Down transfer: Either return transfer to the primary hospital, or transfer to another hospital for recovery
Sideways transfer: Transfer because the required facilities at the referring hospital are fully occupied
Across health services – like acute care to palliative care
Between providers – GP to specialist
Finally, the patient might return home, where he or she would receive care from a visiting nurse. Each of these shifts from care providers and settings is defined as a care transition .
What are we assessing and why?
Care coordination
NSW Health policy (PD2011_015) outlines a five stage process to guide staff and patients through their hospital stay.
1.
Pre Admission/Admission
2.
Interdisciplinary Team Review
3.
Estimated Date of Discharge
4.
Referrals & Liaison for patient transfer of care
5.
Transfer of care out of the hospital
Transfer of Care (Discharge)
There are multiple points during a transfer/discharge at which care processes can break down. These include: preparation of patient and caregiver; communication of vital elements of the care plan; medication reconciliation; patient transport; completion of follow-up care with a practitioner, diagnostic imaging or laboratory testing, and the availability of advance care directives across settings.
Inter-hospital transfer of care
Inter-hospital patient transfer involves the movement of a patient from one hospital to another; it also involves the transfer of information and professional responsibility and accountability for patient care between individuals and teams within the overall system of care (Victorian Quality Council 2008a). Poor patient transfer processes are associated with delayed or loss of continuity of care, duplication of services, increased costs and adverse events including patient death ( these questions for only those department/clinical units who transfer patients to other facilities ).
1 Coleman EA, Boult CE. (2003.) Improving the Quality of Transitional Care for Persons with Complex Care Needs. Journal of the American Geriatrics Society, 51(4):556-
557.