rvh_idea_work_sheet
advertisement

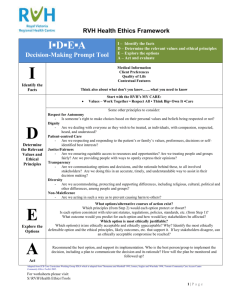
RVH Health Ethics Framework IDEA Decision Making Worksheet C O N F I D E N T I A L when completed I▪D▪E▪A Decision-Making Worksheet I – Identify the facts D – Determine the relevant values and ethical principles E – Explore the options A – Act and evaluate Date Contacted by Contact information I – identify the facts Medical and/or other information Preferences of the patient or other individual involved. The problem and its history. Goals of treatment or intervention. Are there reasonable grounds to question capacity? Probabilities of success. Likely benefits of a good outcome. Potential harms. Can the potential harm be minimized? What preferences have been stated? How or where? Is individual capable now or were they when stating these preferences? In not, how are we understanding likely preferences? Who is legal substitute decision maker? Quality of life Contextual features What is the patient’s view of their quality of life? If they are not capable, what do others say? Consider the impact of emotions, values, experience in order to understand these views. Significant relationships (friends/family/other)? Current care plan? Clinical, legal, economic, organizational, systemic factors? (CLEOS) Cultural, privacy, religious, values? Provider or other conflict of interest? Research or teaching issues? * Adapted from JCB Core Curriculum Working Group IDEA which is adapted from Thomasma and Marshall 1995; Jonsen, Seigler and Winslade 1998; Toronto Community Care Access Centre Community Ethics Toolkit 2005. S:\RVH\Health Ethics\Tools Created: 08/26/14 Page 1 of 4 IDEA Decision Making Worksheet - C O N F I D E N T I A L when completed D – determine the relevant values and principles Identify the relevant values and corresponding ethical principles. Which, if any, principles are: Unclear? Being overlooked? Apparently in conflict? Values and corresponding Application to case/issue? Note apparent conflict(s) with other principles. ethical principles Note which principles each key stakeholder is trying to uphold. Some principles to consider: Respect for Autonomy: Is someone’s right to make choices based on their personal values and beliefs being respected or not? Dignity: Are we dealing with everyone as they wish to be treated, as individuals, with compassion, respected, heard, and understood? Patient-centred Care: Are we respecting and responding to the patient’s or family’s values, preferences, decisions or self-identified best interests? Justice/Fairness: Are we ensuring equitable access to resources and opportunities? Are we treating people and groups fairly? Are we providing people with ways to openly express their opinions? Transparency: Are we communicating options and decisions, and the rationale behind these, to all involved stakeholders? Are we doing this in an accurate, timely, and understandable way to assist in their decision making? Diversity: Are we accommodating, protecting and supporting differences, including religious, cultural, political and other differences, among people and groups? Non-maleficence: Are we acting in such a way as to prevent causing harm to others? S:\RVH\Health Ethics\Tools Created: 08/26/14 Page 2 of 4 IDEA Decision Making Worksheet - C O N F I D E N T I A L when completed E – explore the options What options/alternative courses of action exist? Which principles (from Step 2) would each option protect or thwart? Is each option consistent with relevant statutes, regulations, policies, standards, etc. (from Step 1)? What outcome would you predict for each option and how would key stakeholders be affected? Option Strengths Limitations Which option is most ethically justifiable? Which option(s) is/are ethically acceptable and ethically unacceptable? Why? Identify the most ethically defensible option and the ethical principles, likely outcomes, etc. that support it. If key stakeholders disagree, can an ethically acceptable compromise be reached? S:\RVH\Health Ethics\Tools Created: 08/26/14 Page 3 of 4 IDEA Decision Making Worksheet - C O N F I D E N T I A L when completed A – act, monitor and evaluate (a) Help develop an action plan for the option chosen in Step 3: Recommend the best option, and support its implementation. Who is the best person/group to implement the decision, including a plan to communicate the decision and its rationale? How will the plan be monitored and followed up? (b) If an ethically defensible option cannot be agreed upon/has not been selected, the following steps will be taken: S:\RVH\Health Ethics\Tools Created: 08/26/14 Page 4 of 4