OUTPATIENT TREATMENT - Woodlands Behavioral Healthcare
advertisement
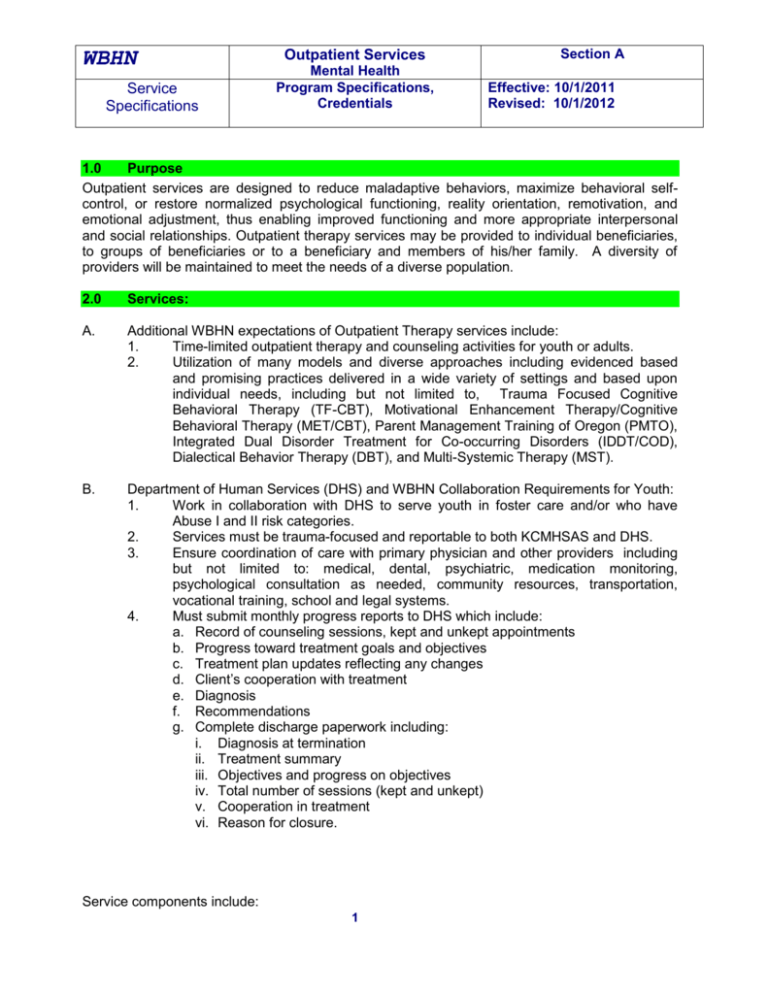
WBHN Service Specifications Outpatient Services Mental Health Program Specifications, Credentials Section A Effective: 10/1/2011 Revised: 10/1/2012 1.0 Purpose Outpatient services are designed to reduce maladaptive behaviors, maximize behavioral selfcontrol, or restore normalized psychological functioning, reality orientation, remotivation, and emotional adjustment, thus enabling improved functioning and more appropriate interpersonal and social relationships. Outpatient therapy services may be provided to individual beneficiaries, to groups of beneficiaries or to a beneficiary and members of his/her family. A diversity of providers will be maintained to meet the needs of a diverse population. 2.0 Services: A. Additional WBHN expectations of Outpatient Therapy services include: 1. Time-limited outpatient therapy and counseling activities for youth or adults. 2. Utilization of many models and diverse approaches including evidenced based and promising practices delivered in a wide variety of settings and based upon individual needs, including but not limited to, Trauma Focused Cognitive Behavioral Therapy (TF-CBT), Motivational Enhancement Therapy/Cognitive Behavioral Therapy (MET/CBT), Parent Management Training of Oregon (PMTO), Integrated Dual Disorder Treatment for Co-occurring Disorders (IDDT/COD), Dialectical Behavior Therapy (DBT), and Multi-Systemic Therapy (MST). B. Department of Human Services (DHS) and WBHN Collaboration Requirements for Youth: 1. Work in collaboration with DHS to serve youth in foster care and/or who have Abuse I and II risk categories. 2. Services must be trauma-focused and reportable to both KCMHSAS and DHS. 3. Ensure coordination of care with primary physician and other providers including but not limited to: medical, dental, psychiatric, medication monitoring, psychological consultation as needed, community resources, transportation, vocational training, school and legal systems. 4. Must submit monthly progress reports to DHS which include: a. Record of counseling sessions, kept and unkept appointments b. Progress toward treatment goals and objectives c. Treatment plan updates reflecting any changes d. Client’s cooperation with treatment e. Diagnosis f. Recommendations g. Complete discharge paperwork including: i. Diagnosis at termination ii. Treatment summary iii. Objectives and progress on objectives iv. Total number of sessions (kept and unkept) v. Cooperation in treatment vi. Reason for closure. Service components include: 1 WBHN Service Specifications Outpatient Services Mental Health Program Specifications, Credentials Section A Effective: 10/1/2011 Revised: 10/1/2012 C. General Service Components for Outpatient Services (Mental Health) 1. Initial and on-going Bio-psychosocial assessments of individual and family service needs. a. A Brief Screen, which is a face to face behavioral health screening to determine the need for mental health and/or substance abuse services. b. An Assessment, which is an individual, face-to-face assessment at the licensed provider level for the purpose of identifying functional and service needs to formulate the basis for the Individualized Plan of Services (IPOS) and/or Treatment Plan. 2. Development of an Individualized Treatment Plan or IPOS based on comprehensive bio-psychosocial assessments, diagnostic impressions and consumer characteristics such as age, gender, culture and development. Plans will include problem formulation, treatment goals and measurable treatment objectives. Plans must be reviewed and up-dated. 3. Person Centered/Family Centered Planning which addresses all beneficiary needs in the pertinent domains. Plans must be reviewed and up-dated at least annually or as often as the individual requests. 4. Dual diagnosis service capability provided in a welcoming environment. 5. Service Coordination a. Coordination with the primary care physician and/or physician who prescribes psychiatric medication. b. Coordination of services for medical, psychiatric, medication monitoring, and psychological consultation as needed. c. Coordination with and/or referral to community resources for "wraparound" support services such as child care, transportation, vocational training, school systems, legal systems, and Department of Human Services. 6. Early Intervention services which are any planned intervention that may assist a person to abstain from alcohol and/or drug use. 7. Outpatient Services (individual, family and group psychotherapy) a. Individual therapy, which is 1:1 face-to-face counseling services with the beneficiary. b. Family therapy, which is face-to-face counseling with the beneficiary and his/her significant other and/or traditional or non-traditional family members. c. Group therapy, which is face-to-face counseling with three or more beneficiaries and can include didactic lectures, therapeutic interventions/counseling, and other group-related activities. 8. Ensuring access to language interpreter, translation services and hearing interpreter services. 9. Discharge planning beginning at the on-set of treatment which includes coordination of after care and referral for on-going supports/services. 3.0 Access, Authorization and Discharge: A. Eligibility Individuals served must have a diagnosis of an Axis I condition or developmental disability, and/or Axis I diagnosis reflected in the DSM IV. 2 WBHN Outpatient Services Service Specifications B. Mental Health Program Specifications, Credentials Section A Effective: 10/1/2011 Revised: 10/1/2012 1. Mental Health Services (including co-occurring services) The focus of treatment must be related to the Axis I diagnosis or a concomitant Axis II diagnosis, and; a. Psychiatric signs and symptoms resulting in minimum to moderate disruption in self-care, relationship, employment or school, and other areas of life. b. Suicidal ideation, non-accidental behavior or suicidal gestures that have potential to cause serious injury or threaten life. c. Inappropriate behavior towards others that is threatening or sexually aggressive with potential for harm. d. Adults receiving service must assume responsibility for their own treatment and change. 2. Outpatient Care services should be limited to individuals who will benefit from treatment and have been determined to have the following: a. Demonstrated readiness to change b. Minimal or manageable medical conditions c. Minimal or manageable withdrawal risks d. Level of care suited to emotional, behavioral and cognitive conditions e. Minimal or manageable relapse potential f. Minimally to fully supportive recovery environment Authorization 1. Mental Health Services (Eligibility, Level of Care and Access Center Role) Determination of eligibility and assignment of a level of care is done by the WBHN Access. An integrated assessment tool(s) behavioral health issues is completed. Individuals are provided with informed choice of provider upon determination of level of care required. The WBHN Access staff will forward the initial diagnostic impression, level of care determination and service authorization, including the amount, scope and duration of service, to the provider chosen by the person along with a release of information. a. Initial Authorization. A comprehensive bio-psychosocial assessment is completed which concludes that the individual does not meet criteria to be served under the 20-outpatient visit benefit of a Medicaid Mental Health Plan. Scope and duration of service is determined consistent with clinical criteria for the diagnosis and treatment modality to be employed, typically 4-20 sessions. On average, the Individual should be seen for outpatient services at least two times a month. b. Ongoing Authorization. Services may be re-authorized based on extensive clinical justification of continued progress or change in treatment modality. of continued progress or change in treatment modality. C. Discharge Individuals shall be discharged, and transitioned from outpatient services when: 1. The individual no longer meets the severity of illness criteria and has demonstrated the ability to meet all major role functions for a period of time sufficient to 3 WBHN Outpatient Services Service Specifications Mental Health Program Specifications, Credentials Section A Effective: 10/1/2011 Revised: 10/1/2012 demonstrate clinical stability. If an individual requests transition to other service(s) because they believe they have received maximum benefit, consideration for the transition must be reviewed during the person-centered planning (PCP) process. If clinical evidence supports the individual’s desire to transition, this evidence and the transition plan must be detailed in a revised Individual Plan of Service developed through the PCP process. The plan must identify what supports and services will be made available. 2. 3. 4. 5. 6. 4.0 Engagement of the individual in outpatient services is not possible, and the individual is unwilling to participate in treatment. The individual has moved outside of the geographic area and contact continues until services have been established in the new location. Referral to a more intensive treatment modality is justified by assessment. Individual no longer meets medical necessity criteria. Medical necessity criteria can employ various methods to determine the amount, scope, duration of services, including prior authorization for certain services, concurrent utilization reviews, centralized assessment and referral, gate keeping arrangements, protocols and guidelines. Other factors influencing discharge: a. The individual does not demonstrate capacity to benefit from outpatient services. b. There is a significant change in the individual’s psychiatric illness, and the individual would be more appropriately served by another treatment modality. c. An individual is incarcerated in long term treatment or criminal justice facility. Credentials: Staff qualification requirements for MDCH and Medicaid services are noted in the documents referenced in Section 5.0, References. 5.0 References: Services and provider credentials must be consistent with the requirements of the following documents as applicable: Medicaid Provider Manual – Mental Health and Substance Abuse Services Section 3 Individual/Group Therapy Southwest Michigan Affiliation (SMA) Policies Section 2.0 Provider Network Management Section 6 Customer Services Section 23 Grievance and Appeals Section 24 Rights of Recipients Section 25 Rights Complaints and Dispute Resolution Section 30 Utilization Management and Access Section 31 Clinical Practices Section 32 Intake and Assessment 4 WBHN Service Specifications Outpatient Services Mental Health Program Specifications, Credentials Section 33 Consumer Planning Section 34 Transition, Discharge and Follow-up Section 40 Services Coordination Section 42 Children and Adolescents Children’s Administrative Rules Section 330.2125 PIHP- MHSP Provider Qualifications for Medicaid Services 5 Section A Effective: 10/1/2011 Revised: 10/1/2012