Endometriosis Endometriosis is a disorder that occurs when tissue
advertisement

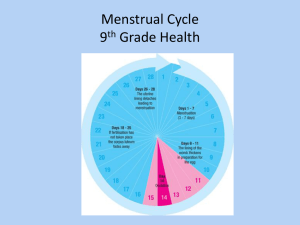
Endometriosis Endometriosis is a disorder that occurs when tissue that normally lines the inside of your uterus (womb) grows outside your uterus. Women with endometriosis usually have tissue (endometrial implants) on the ovaries, bowel, rectum, bladder and on the lining of the pelvis. When you have endometriosis displaced edometrial tissue continues to act as it normally would, it thickens, breaks down and sometimes bleeds with each menstrual cycle. The difference is that this displaced tissue, unlike the endometrial tissue in your uterus, has no way to leave your body and, becomes trapped. It then grows again until your next period. This ongoing process can result in the surrounding tissue becoming irritated and developing scar tissue and adhesions or abnormal tissue, which binds organs together. Endometriosis can often result in pain, irregular bleeding and difficulty getting pregnant or fertility problems. Symptoms The primary symptom of endometriosis is pain in the pelvic area, which is frequently associated with a woman's period. Many women with endometriosis indicate that the pain is severe, and report that menstrual pain is much worse than usual. Symptoms of endometriosis may also include the following: Painful periods Pain in the lower abdomen before and during menstruation Pain with bowel movements or urination Pelvic or low back pain that may occur at any time during the menstrual cycle Pain with intercourse Cramps for a week or two before menstruation and during menstruation, cramps may be steady ranging from dull to severe Excessive bleeding Infertility ( problems getting pregnant) Additional symptoms are fatigue, constipation, diarrhea, bloating or nausea during menstrual periods. Some women experience no pain or other symptoms. Causes The exact cause of endometriosis is not known. There is some evidence that endometriosis occurs when endometrial cells shed, during your menstrual period, and travel backwards through the fallopian tubes to the pelvis, where they implant and grow. This is called retrograde menstruation. While many women experience this backward menstrual flow, scientists believe that the immune system is different in women with endometriosis. Risk factors There are several factors that put women at a greater risk for endometriosis including the following: Starting your period at a young age Never giving birth One or more relatives (mother, sister or aunt) with endometriosis History of pelvic infection Having frequent periods or they last 7 or more days Any medical condition that prevents or blocks the normal menstrual flow out of the body (e.g. closed hymen) Uterine abnormalities Typically, endometriosis develops several years after the onset of menstruation (menarche). The symptoms of endometriosis cease temporarily with pregnancy and end permanently with menopause, unless you are taking hormones. Diagnosis Diagnosing endometriosis usually occurs using the following tests: Pelvic exam. Your doctor will perform a pelvic exam to feel for abnormalities in your pelvis such as scars behind your uterus or cysts on your reproductive organs. Frequently it is not possible to feel small areas of endometriosis unless they have produced a cyst. Ultrasound. The images created by the ultrasound will provide a view of your reproductive organs. These images will not give your doctor definite evidence of endometriosis, but it can identify cysts associated with endometriosis, called endometriomas. Laparoscopy. Your doctor willl ususlly attempt medical management of your endometriosis, but he may also refer you to a surgeon who will look inside your abdomen for signs of endometriosis using a surgical procedure called a laparoscopy. Laparoscopy, which may involve samples of tissue (biopsy) can locate endometrial tissue outside the uterus and provide information about the location, extent and size of endometrial implants. This information will help your doctor to determine the best treatment options. Treatments Treatments for endometriosis usually involve medications or surgery. Your doctor will select methods to treat your endometriosis depending on the severity of your symptoms, and whether you want to become pregnant. Doctors usually use conervative treatment approaches initially, and save surgery as the last resort. Your doctor may choose to treat your endometriosis with the following: Pain medications. Over-the-counter pain relievers, such as nonsteroidal antiinflammatory drugs (NSAIDs), ibuprofen (Advil, Motrin IB, and others) or naproxen (Aleve and others) may be prescribed to help ease painful menstrual cramps. Hormone therapy. Your doctor may prescribe supplemental hormones, which are sometimes effective in reducing or eliminating the pain of endometriosis. Hormone therapy may also prevent or slow the growth of new endometrial implants. Conservative surgery. Conservative surgery may be a treatment method if you have endometriosis and are trying to become pregnant. This means the surgeon will remove as much endometriosis as possible while preserving your uterus and ovaries to increase the chance of you becoming pregnant. When the pain is severe from endometriosis surgery may also provide some benefits, but the pain and endometriosis may return. Assisted reproductive technologies. Various assisted reproductive technologies, such as in vitro fertilization, may be recommended by your doctor to help you become pregnant if you have endometriosis, instead of conservative surgery. Hysterectomy. Surgery to remove the uterus and cervix (total hysterectomy) as well as both ovaries is considered the best treatment option in some severe cases of endometriosis. Hysterectomy alone is not effective because your ovaries will produce estrogen that can stimulate any remaining endometriosis and cause pain to continue. Hysterectomy is usually considered as a last resort, especially for women who are still in their reproductive years, since you cannot get pregnant after a hysterectomy. It is important to see a doctor if you have the symptoms of endometriosis, for the purpose of diagnosing, managing and treating your condition. References "Endometriosis." Mayo Clinic. April 2, 2013. "Endometriosis." National Institutes of Health. May 20, 2013.