November - Angela Kempen
advertisement

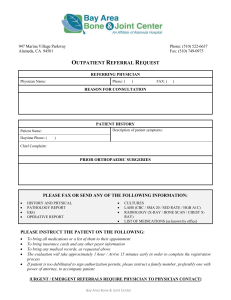
Angela Kempen November Case Study November 27, 2012 Intensity Modulated Radiation Therapy for Right Petroclival Meningioma of the Brain History of Present Illness: KP is a 52 year-old woman who presented with approximately a 3year history of diplopia. A physician saw the patient at the end of July and examination revealed third and sixth nerve palsy with pupillary asymmetry. Magnetic resonance imaging (MRI) was performed which showed a large enhancing mass in the right petroclival region consistent with a meningioma. There was encasement of the carotid artery and displacement of the brainstem. There was extensive involvement of the cavernous sinus and the sella. The mass measured approximately 4 centimeters (cm) in size. The patient was referred to the University of Wisconsin Hospital and Clinic and met with a physician from their skull based team. The patient was recommended to undergo a 2-stage procedure. She underwent a right orbital zygomatic approach for the lesion on August 31, 2012, with debulking of the tumor. This showed a meningioma without any features of atypia or anaplasia. The patient was allowed to recover from that procedure and subsequently was taken back to the operating room for the second procedure which was a right retro-sigmoid craniotomy and subtotal resection of a portion of the petroclival part of the tumor. Again, she had a good recovery. She still has significant diplopia. She has had no change in her vision. She has no focal muscular weakness. She has decreased sensation on the right side of her face to light touch. She was having sensory seizures prior to starting Keppra. Her seizures were sensory in nature. She states she would have odd smells or tastes, and at times, seemed to hear things. She is having minimal headaches. She takes occasional oxycodone primarily at night to help with pain. She has no problems with balance or coordination. She indicates her cognitive function is stable. She has been asked to be seen for the consideration of postoperative radiotherapy to address the residual tumor that was unresectable. She has no previous history of malignancy. She has no previous history of radiotherapy. Past Medical History: The patient has hypertension. She also has anxiety and depression, which may be related to her diagnosis. 2 Diagnostic Imaging Studies: A preoperative MRI was performed which showed a large enhancing mass in the right petroclival region consistent with a meningioma. There was encasement of the carotid artery and displacement of the brainstem. There was extensive involvement of the cavernous sinus and the sella. The mass measured approximately 4 centimeters (cm) in size. A biopsy and excision was done on the right cavernous sinus, revealing a World Health Organization (WHO) grade I meningioma. A postoperative MRI was done and reviewed. This showed a subtotal resection, but not significant debulking of the right petroclival meningioma. The mass effect on the brainstem was improved. Family History: The patient’s mother and father are both deceased due to illnesses related to smoking. She has three brothers who are alive and well. Social History: The patient is married and resides with her husband. She is a former one pack a day smoker, but quit in 2007. She rarely drinks alcohol. Medications: The patient uses the following medications: acetaminophen, benzonatate, cholecalciferol, citalopram, gluco sulfate NaCl-Chond, Levetiracetam, metoprolol, oxycodone and psyllium. Recommendations: The radiation oncologist recommended that the patient receive postoperative radiotherapy to the area of the tumor with margins for this low-grade meningioma. The goals of therapy, along with the risks of treatment were discussed with the patient and her husband. The Plan (Prescription): The plan is for the patient to receive a total dose of 50.4 Gy in 28 fractions using intensity modulated radiation therapy (IMRT). Patient Setup/Immobilization: The patient was simulated in the supine position, with an Aquaplast mask used for immobilization of her head and neck region. A treatment planning computed tomography (TPCT) was completed with 2.5 millimeter (mm) slices through her head and upper neck region. Anatomical Contouring: The TPCT was fused with an MRI scan, on MIM, for the physician to contour his planning target volume (PTV). The physician contoured the right petroclival mass 3 PTV, in addition to the optic chiasm and optic nerves. I contoured the brain, brainstem, eyes, and lens and created a 1 cm ring around the right petroclival mass PTV, in addition to a normal tissue volume. Beam Isocenter/Arrangement: The patient was treated on a Varian 21EX linear accelerator with 6 MV photon energies. The isocenter was placed in the middle of the right petroclival mass PTV. I used an IMRT beam arrangement, consisting of five beams. I began on the right side of the patient and set the first beam with a gantry angle of 200 degrees. I than placed four more beams at gantry angles of 265, 295, 80 and 125 degrees around the patient. Treatment Planning: The Varian Eclipse treatment planning system was used for this plan. The physician provided a list of what he would like to achieve with this plan. His objectives included at least 95% of the right petroclival mass PTV to receive 50.4 Gy in 28 fractions. He wanted to keep the optic nerves less than 105% of the prescription dose, and the optic chiasm less than 53 Gy. The brain and brainstem were to receive no more than 54 Gy. The eyes were to be kept below 30 Gy and the lens below 7 Gy. I entered the above objectives into the optimization parameters. I started to run the optimization and after the first trial, the right lens, right optic nerve and brain were too hot. There were also significant hot spots outside of the PTV. I entered additional parameters and increased the priority on those structures. In addition, I increased the priority on the normal tissue volume to try and eliminate the hot spots outside the PTV. It took a few more trials until I achieved a plan that met the physician’s objectives. The plan was prescribed to the 99.8% isodose line and approved by the physician. The isodose lines can be viewed in Figure 1 and Figure 2. Figure 3 shows the dose volume histogram for this plan. 4 Figure 1: Axial, Sagittal, and Coronal slices 5 Figure 2: Isodose distribution through axial slices Monitor Unit Check: Independent monitor unit checks are not done at my facility for IMRT treatment planning. These values are taken from the Mapcheck QA done on the linear accelerator. Quality Assurance Check: Mapcheck®, which is a Sun Nuclear diode array, was used in order to verify the dose distribution of the plan. To calculate the measured output, the plan was run on a MapCheck phantom on the linear accelerator where the output per field was taken. The fluence of the IMRT plan is then computed onto a phantom in the Eclipse treatment planning system. The treatment planning computer MU values are compared to the measured output obtained at 5cm depth from MapCheck. This value was then compared to the expected MU values, ensuring that the plan is safe for treatment. Conclusion: I chose this case study because it was the first brain IMRT case I have completed. In the past, I created plans using volumetric intensity radiation therapy (VMAT) for brain cases. However, with this patient, both VMAT and IMRT plans were calculated and the IMRT plan 6 was superior. The main reason was integral brain dose. The brain dose was kept lower with the IMRT plan, which the physician preferred. It was a great learning experience for me to be able to plan this case using both techniques. Figure 3: Dose Volume Histogram