Answer key – case study #3 - Southwest Pennsylvania
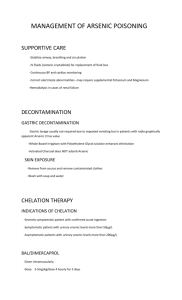
advertisement

SWHP EHP July 20, 2012 Health care tool kit Case #3: Man who wants to be tested for everything 30 yo male comes in for follow-up after being evaluated by your covering physician while you were on vacation. He is concerned that has been exposed to toxins because his neighbor has had a gas well drilled on his property, though not yet “fracked”. After the drilling, the neighbor noticed some transient bubbling and black solids in his well water. The covering physician who evaluated your patient performed a 24 hour urine screen for heavy metals and has informed your patient that his arsenic is elevated. He has noted some intermittent numbness in his right hand and, after some internet searching, believes it is caused by his arsenic poisoning. He wants to be chelated. He also wants to be tested for “everything”. He has stopped drinking and cooking with his well water. He owns his home. Lives alone. Does not smoke and makes a good living as a mason. Would you have tested this patient for arsenic? When considering biomonitoring, it is best to have identified through environmental sampling (air or water, for example) a specific likely hazardous exposure. This patient is concerned about possible exposure from his well water. He identifies no other potential exposures, such as burning old pressure treated wood or any occupational exposure to arsenic. Testing his well water would have been a first appropriate step. It is also important to know something about the toxicokinetics of the hazardous substance, such as how it is excreted and its half-life in the body in order to determine the appropriate medium and timing for testing. Biomonitoring results reflect all the sources of exposure to a substance. SWHP EHP July 20, 2012 Health care tool kit The ½ life of arsenic in blood is in hours. Arsenic is excreted in urine with a halflife of several days, so urine is an appropriate medium. The urine arsenic results were 500 mcg/l, with a laboratory normal of <35 mcg/l. Has your patient experienced a toxic arsenic exposure? The urine arsenic results reflect all sources of arsenic exposure. Individuals are commonly exposed to high levels of non-toxic forms of organic arsenic in seafood. It is recommended that individuals abstain from seafood for > 48 hours prior to a urine collection for arsenic. Alternatively, a urine specimen can be speciated, separating the toxic forms of arsenic from the non-toxic. Your patient mentions that he eats seafood frequently and did not abstain prior to the urine test. Arsenic is naturally occurring in some wells in Pennsylvania. Until the well is tested and the urine test speciated or repeated after abstaining from seafood, you cannot be certain if your patient has been exposed to arsenic. Is your patient’s hand numbness likely to be caused by arsenic exposure? Your patient, who is right handed, has noticed some intermittent numbness in the right hand over the past year. Recently, on several occasions he has awoken at night due to the numbness and has had to shake his hand out before falling back to sleep. He has no numbness in his left hand or in his feet. He is not diabetic and has no history of thyroid disease. He is employed as a mason. He has been working overtime recently building new offices for employees of the gas industry. He uses the internet several hours a day and occasionally plays video games. He has had no recent injuries. His exam is normal, with the exception of a positive Tinel’s test over the median nerve in the R wrist. Although arsenic exposure can cause a peripheral neuropathy, the neuropathy resulting from arsenic exposure typically occurs in a symmetrical, stocking glove SWHP EHP July 20, 2012 Health care tool kit distribution affecting both hands and feet. It involves sensory greater than motor neurons. Although the patient believes his symptoms are attributable to arsenic exposure, your role is to first make an accurate diagnosis, and to then consider whether his potential exposure might have contributed to the diagnosis. Should the patient be chelated? Except in rare cases of acute arsenic poisoning, there is almost no role for chelation therapy in the treatment of arsenic exposure. With regards to chelating individuals concerned about other potential exposures related to unconventional gas extraction, the internet is filled with claims of the benefits of chelation therapy. In addition, after performing a post-chelator challenge urinary metal test showing urine metal levels higher than reference values based on a non-chelated specimen, some practitioners believe that their patients will benefit from chelation therapy. This practice has proved dangerous and even fatal at times. The American College of Medical Toxicologist position statement on post-chelator challenge urinary metal testing concludes that “It is, therefore, the position of the American College of Medical Toxicology that post-challenge urinary metal testing has not been scientifically validated, has no demonstrated benefit, and may be harmful when applied in the assessment and treatment of patients in whom there is concern for metal poisoning.” What about other tests? With modern technology, laboratories can test for almost anything in blood or urine. Rarely are there health based reference ranges to interpret the results. If the lab uses references ranges based on population exposure data, such as the CDC’s Fourth National Report on Human Exposures to Environmental Chemicals the ranges need to be adjusted for gender, age and ethnicity. Even if a value is SWHP EHP July 20, 2012 Health care tool kit above the 95% in a population reference range, it may not tell you anything about the implications for the patient’s health. Since volatile organic compounds such as benzene, toluene, ethylbenzene and xylene are potential exposures of concern from gas drilling activities, practitioners are often interested in testing their patients for exposures to these substances. The CDC and ATSDR generally discourage this testing for reasons as detailed in the “CDC/ATSDR Guidance on the Interpretation and Use of Blood Laboratory Analyses for Volatile Organic Compounds” The two primary reasons they discourage testing are the short half-lives of VOC’s in the body, and the numerous sources of everyday exposures such as gasoline, cigarettes, vehicular exhaust, and solvents, complicating interpretation of the results. When deciding whether or not to test your patients for a specific chemical exposure, it’s important to consider the overall sensitivity and specificity of the potential test. In this case, sensitivity means if your patient was exposed, is the test likely to indicate an exposure. Specificity means, if your patient wasn’t exposed, is the test likely to be negative. When a substance has a short half-life in the body, a test that is not performed immediately after the exposure may be negative, falsely reassuring the patient that there was no exposure. On the other hand, a test for an exposure where there are multiple other contributors to a positive result, may appear to be positive when there was no actual exposure form the source of concern. When deciding whether or not to test your patients for a specific chemical exposure, given that there are often no health based reference ranges, it is important to understand in advance, what advice you are going to give your patients based on the results.