F3_-_T_cell_condensed
advertisement

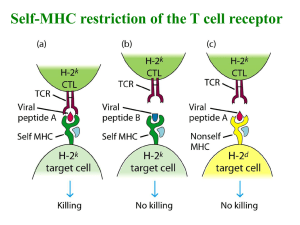
T cell related (Fleischmann) Helper T cells recognize antigenic peptides presented by APCs to their T cell receptors (TCRs). TCRs are heterodimers. o αβ dimer TCRs are very specific to Ag (similar to Ig molecules on B cells). Ag is presented by MHC, adaptive immune response is activated and Ag killed by granulysin & perforin. Membrane bound d/t transmembrane cytoplasmic tail region. While a T cell can produce 2 of these, it is unlikely that 2 would become self-restricted T cells and leave the thymus. α chain (similar to Ig L chain) is encoded by V, J & C gene segments β chain (similar to Ig H chain) is encoded by V, D, J & C gene segments = more variability o o o o Mechanism of TCR rearrangement: pre-T cell has RAG-1 & RAG-2 expressed that will recognize conserved RSSs nicks one strand of TCR DNA DNA loops out each rearranged DNA sequence will encode a single type of TCR. TCRs have variability because of the different combinations of V, D, J regions that create different Ag-binding specificities as well alternative joining of D gene sequences. P and N nucleotide additions also contributes. There is no maturation of affinity here b/c it could be potentially harmful if a TCR changed then no longer recognized self. δ dimer TCRs recognize groups of pathogens (similar to Toll receptors of innate immunity – pattern recognition). Direct interaction w/ Ag. Recognizes regions on M. tuberculosis, other bacteria & parasites. Part of chronic autoimmune diseases (lupus, MS). Produce cytokines that can recruit αβ an can present Ag. CD3 is associated w/ TCR and is composed of 3 dimers (ζζ most imp) that aggregate near the TCR, include a region, ITAM (immunoreceptor tyrosine-based activation motif) that is important for signal transduction across the membrane. CD4 binds to Class II Ag & signal transduction molecule p56Ick that will form a bridge that binds to ζζ. CD8 binds to Class I Ag, held together by disulfide bond. Both of these co-receptors add to the binding affinity between TCR & MHC/peptide complex. These T cells are alloreactive to molecules other than to their cognate MHC (will react to MHCs other than their own d/t genetic differences). Direct allorecognition occurs when MHCs are recognized as foreign antigens +/- being bound to a foreign protein. Indirect allorecognition is when an MHC is internalized, processed & presented to immune system bound to self-MHC. Other co-receptors that add to binding affinity: CD2B7; LFA-1 ICAM-1; CD28 B7; CD45R CD22 MHC (major histocompatibility) molecules are important for Ag recognition & presentation to the immune system (at the T Cell Receptor). There are >100 genes in MHC gene complex divided into Class I, Class II & Class III. Class I & II also have subclasses of gene loci, giving rise to polymorphism. Polymorphism provides uniqueness and recognition of non-self. The TCR will only recognize Ag that is bound to their own MHC with cognate Ag = self-MHC restriction. o MHC class I presents Ag to CD8+ T cytotoxic cells that will be activated (w/ correct co-stimulatory molecules & cytokine production) to kill cells expressing the Ag. This is on most nucleated cells. When expressed on cell surface, they associate w/ β₂microglobulin (1 peptide). Binding cleft is closed at both ends, binds peptides that are 810 aa in length and anchors them at both ends. o MHC class II presents Ag to CD4+ T helper cells that will be activated (w/ correct co-stimulatory molecules & cytokine production) to either activate B cells to mature to Ab-producing plasma cells OR to activate more CD8+ cytotoxic T cells to kill. On APCs. When expressed on cell surface the gene locus encodes 2 peptides, α subunit & β subunit. Binding cleft is open at both ends, binds peptides 13-22 aas in length and are anchored along the length of the peptide. o MHC class III genes aren’t involved in Ag presentation. They include complement proteins & TNF-α and TNF-β, HSPs Polymorphism affects ability to make immune response, response to infectious disease & susceptibility to autoimmune diseases & allergies (ex: if you have HLA-B27, you are more likely to get ankylosing spondylitis, HLA-DR2 narcolepsy, HLA-A3/B14 hemochromatosis). Most of the differences are seen in the cleft region (antigenic peptide binding site). There are 6 different MCH I & 12 different MHC II molecules that arise from different combinations of α and β subunits. Since this is nowhere near the number of potential Ags that can bind, a weaker association is made when Ag binds to the peptide binding clefts. Loci for Class I & II are inherited as a two haplotypes (cassette from each parent) and we have codominant expression of each allele. Recombination is rare between Class I & II because they are so closely linked. o Syngeneic: having same gene alleles in your 2 haplotypes as someone else, usually only seen with identical twins. Congenic: differ only in 1 locus. This is important for transplants. Ags that are products of phagocytosis are expressed on MHC II & Ags that are intracellular protein products are expressed on MHC I Antigen-Presenting Cells (APCs) process Ag for presentation to T cells. o Dendritic cells are the most effective APC b/c they the express MHC II & B7 (required costimulatory molecule). Low levels of MHC II are expressed in peripheral tissue, dendritic cell at immature phase mature phase occurs in lymphoid tissue where high levels are expressed. They present peptides, viral Ags & allergens. o B cells are next best since they express MHC II but need to be activated (by Ag binding to Ab) in order to express co-stim molecules. Present soluble Ags, toxins & viruses. o Macrophages are the slowest b/c need to be activated (by phagocytosis of bacteria & by cytokines) to express both. Present intracellular & extracellular pathogens. Antigen processing & presentation occurs via 2 different pathways depending on where the Ag came from. The cytosolic pathway is for Ag presentation on MHC I of endogenous Ag while the endocytic pathway is for MHC II of exogenous Ag brought in by phagocytosis. o Some of the endogenous proteins degraded by the cytosolic pathway are called DRiPs, defective ribosomal products that arise from incorrect synthesis. Virus infected cells have a distinct 20S proteasome induced by IFN- & TNF-α. Degradation of misfolded proteins occurs through the 20S proteasome while those that are intact are tagged with Ubiquitin go through a 26S proteasome (20S + 19S regulatory component). The 20S has 28 polypeptide subunits in 4 rings – outside 2 are α subunits and inside 2 are 7 kinds of β subunits. Enzymatic cleavage or proteins happens in central tube. The 20S immunoproteasome has IFN- within the β subunits which makes it more likely to cleave by hydrophobic aas giving greater binding affinity to TAP. o TAP is a transporter protein heterocomplex that transports peptides from cyto RER for synthesis of MHC I. TAP1 & TAP2 dimerize and allow peptide to move through RER to lumen side where it can then attach to MHC I. TAP prefers peptides 8-16 aa long, which is good b/c 9 aa is ideal for Class I binding. ERAP1 (ER aminopeptidase) helps trim them down. Class I also wants to bind to peptides that have specific aas that are imp in binding to the peptide cleft (carboxyterminal anchor is hydrophobic as well as another hydrophobic anchor 2-3 aa away from aminoterminus). If they are too small or if they can’t be used by MHC, ERAP2 degrades them. o Assembly of MHC Class I molecule (KNOW all the steps in this diagram!) α-chain made. Calnexin gets up next to the α subunit and stabilizes. β₂ microglobulin added & calnexin goes away. Tapasin is adaptor, binds to class I Ag & to TAP. Calreticulin opens groove, allowing for ERp57 to protect = ‘cap’. Once peptide can bind, calreticulin goes away. o TAP deficiency pts can’t express Class I molecules or antigentic peptides, can’t fight bacteria, have overactive NK cells necrotizing granulomatous lesions on skin of face & extremities. o The endocytic pathway processes exogenous antigens that are internalized by phagocytosis from MOS & dendritic cells & receptor-mediated endocytosis by B cells. Ab bound Ag is internalized in early endosomes late endosomes lysosomes where Ag is degraded to 13-18 aa oligopeptides which are then bound to MHC class II molecules and transported to surface. During this time, Ab releases Ag and is recycled to membrane. Invariant chain combines with MHC Class II after they are made in the RER. This helps the class II α and β chains fold, keeps other things from binding in the peptide’s spot, helps transport from RER Golgi cytoplasmic vesicles. During this mvmt, the invariant chain is slowly degraded until all that is left is CLIP, a small fragment. HLA-DM catalyzes exchange of CLIP & antigenic peptide that will bind very strongly now. (HLA-DM is regulated by HLA-DO which is expressed only on B cells and in thymus, is NOT induced by IFN-, and wont bind to HLA-DM under acidic conditions) Abnormalities: o Cross-presentation of exogenous Ag occurs when an APC presents exogenous Ag to Class I (normally its to Class II), we think at the lumen of the RER. Could allow dendritic cells to phagocytose viruses & present viral Ags w/ Class I = Tc cells activated to kill virus-infected cells before the infection spreads. o Nonpeptide Ags can be presented by CD1. CD1 can present Glycolipids & mycolic acid from the Mycobacterium species. They present to Tc cells w/ δ TCR and NK cells. T cells leave the bone marrow with CD44 that directs them to the thymus where they will mature. While they are maturing they are named thymocytes and undergo positive & negative selection. Notch protein, expressed by thymic stromal cells, must be present for T cells to mature. 3 week process of maturation: CD4- CD8- CD4+ CD8+ CD4+ OR CD8+ mature o Positive selection allows T cells to survive if they recognize self-MHC molecules. Negative selection eliminates T cells that over-respond to self (or self + peptide) allowing self-tolerant T cells to be produced = CENTRAL TOLERANCE. About 2% of thymocytes actually mature. T cell activation occurs from binding of one TCR w/ Ag. (and in Th cells, also need signal from CD28 on T cell interacting w/ B7 on APC, this induces CTLA-4 expression which can later be bound by B7 to slow down). Clonal anergy occurs where there is no costimulatory signal present; T cell is worthless. o Many genes are activated by Ag binding. Immediate Early Genes w/in 30 min, encode transcription factors: c-Fos, c-Myc, c-Jun, NFAT & NF-κB. Early genes w/in 1-2 hrs, encode IL-2, IL2R, IL-3, IL-6, IFN-. Late genes 2 days later, encode adhesion molecules. P56Lck phosphorylates ITAMs on ζ chains, creating docking site for ZAP-70 which phosphorylates adaptor molecules that activate other enzymes PLPC activation causes breakdown of PIP₂ to IP₃ & DAG / GEF is also activated leading to the Ras/ MAP Kinase pathway. Small G proteins active. IP₃ causes rapid release of Ca from ER, opens Ca channels in cell membrane & activates transcription factor NFAT needed for making IL-2 & IL-4. DAG activates PKc which phosphorylates lots of things & activates transcription factor NF-κB that will help make IL-2. Ras/MAP Kinase pathway activates Fos/Jun/AP-1 which activates a number of genes involved in cell division. o Superantigens bind to both MHC & TCR but aren’t in antigen groove of MHC and stimulate a nonspecific reaction causing a lot of T cells to be activated and overinduction of cytokines. This can lead to toxic shock. Staph and strep. T cells are naïve when they leave the thymus. They circulate: blood lymph lymphoid tissues blood in 12-24 hours. This circulation is needed to provide adequate exposure possibilities between T cell and Ag. Primary response is initiated when TCR binds Ag: 24 hrs later T cell blast cell that divides. IL-2 synthesis is increased by IL-2 mRNA synthesis & stabilization, IL-2 binding to the IL-2 receptor also activates proliferation clone of T cells. After proliferation, effector (not memory) T cells undergo apoptosis either by FasL (2-4 hrs) or MHCAg (8-10 hrs) o Effector T cells can be induced from naïve T cells or from memory T cells when exposed to Ag, they are short lived can be either CD4+ Th (Th1 secretes IL-2, IFN-, TNF-β and stimulates cell mediated immunity; Th2 secretes IL-4, IL-5, IL-6, IL-10 and stimulates humoral (Ab mediated) immunity) or CD8+ Tc. o Memory T cells can be induced from naïve T cells or from effector T cells after antigenic activation & differentiation. Long lived & can be reactivated by re-exposure to Ag to become effector cells (secondary response). Can be activated by all APCs. o Regulatory T cells (Tregs) regulate the immune response (CD4+Cd25+FoxP3+ subpopulation) o Stages of T cell maturation: --DN1 cells enter thymus. CD44 is needed for localization to thymus. c-Kit is a receptor for stem cell factor & needed for initiation of growth in thymic environment. DN1 cells start to proliferate & express CD25. --DN2 cells have turned on synthesis of CD25. Turn on RAG1 & 2 and start rearranging TCR δ, , β. Cells that will express TCR δ diverge from other T cells w/ transition from DN2 to DN3 and leave thymus. --DN3 cells have turned off c-kit & CD44. TCR β is rearranged & combines w/ pre-Tα chain which will associate w/ CD3 group of molecules to form preTCR. --Now, activation signal is transduced across membrane, further proliferation & maturation is induced, further rearrangement of TCRβ is suppressed, TCRα can be rearranged, progression to CD4+CD8+ T cell is induced. (The delay of rearranging the TCRα allows increased diversity in T cells). --DN4 turns off expression of CD25. Expression of CD4 & CD8 is turned on. The double positive cells undergo rapid proliferation, creating clones w/ same β chain. Then α chain is synthesized. Now that the TCR is functional the T cell can undergo positive and negative selection. The double positive cell then loses one if its positive markers & the single positive undergoes further negative selection.