MGH Ebola Clinical Guideline
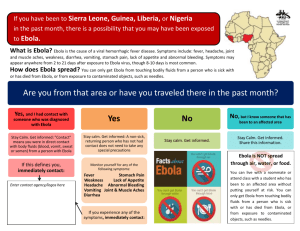
advertisement
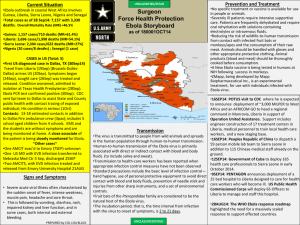
October 1, 2014 To the MGH Care Providers, As you may already know, the U.S. Centers for Disease Control and Prevention (CDC) has confirmed a patient in a Texas hospital tested positive for the Ebola virus disease. This case is the first diagnosed in the United States and the first of this Ebola strain outside of Africa. We understand this occurrence has raised a number of questions and concerns within our hospital community, and we want to assure you that we remain vigilant in our efforts to monitor this situation both nationally and internationally. A dedicated interdisciplinary group made up of hospital leaders from a number of MGH specialties continues to meet regularly to ensure we are prepared to care for patients who may have been exposed to or infected with the virus should the need arise. As always, our focus is the health and safety of our patients, their families and our staff members. We ask that clinicians carefully review the following guideline re: identification and management of suspect Ebola Cases. More detailed guidance is available on the MGH Infection Control Unit website Please note that this information may evolve over time, and therefore, it will be best to refer to the website for the most recent information, rather than a printed copy of this document. SUSPECT CASES AND INITIAL EVALUATION Who should be evaluated as a suspect Ebola case? Clinicians should ask patients presenting with fever about travel within the previous 21 days to West African countries with identified cases of Ebola (Liberia, Sierra Leone, Guinea, Nigeria and Senegal). Consider any patient meeting both of the following clinical and exposure criteria as a suspect Ebola case: 1. Fever > 38.0/100.4°F and one or more of the following symptoms: severe headache, muscle pain, vomiting, diarrhea, abdominal pain, or unexplained hemorrhage 2. Exposure to one or more of the following risk factors within 21 days before onset of symptoms: a. High Risk: Direct contact with blood, other bodily fluids or human remains (e.g., during funeral rites) of a person with suspected or confirmed Ebola without the use of appropriate personal protective equipment. This includes laboratory workers who have processed body fluids from suspected or confirmed Ebola patients without appropriate personal protective equipment or standard biosafety precautions. b. Low Risk: Travel to or residence in an area where Ebola transmission is active (Liberia, Sierra Leone, Guinea, Nigeria and Senegal) AND i. Residence in the same house as an Ebola patient, or ii. Provision of care to an Ebola patient (without known high risk exposure as above) or iii. Had other casual contact with an Ebola patient. Casual contact is defined as being in close proximity (e.g., within 3 feet) for a prolonged period of time while not wearing recommended personal protective equipment or having brief direct contact (e.g., shaking hands) with an Ebola case while not wearing personal protective equipment. Brief interactions, such as walking by a person or moving through a hospital, do not constitute casual contact. Persons who were present in an Ebola outbreak affected country in the past 21 days but with no high or low risk exposures are considered to be at no recognized risk for Ebola at this time. What should I do if a patient meets the criteria for a suspected Ebola case? 1. If a patient meets Ebola suspect case criteria based on symptoms, travel history, exposure risk, contact the ED immediately at 617-724-3890, to discuss the case. 2. While the patient is in your area, place the patient into a private room [Airborne Infection Isolation (AII) room if available] as soon as possible with the door closed. If AII room is used, validate negative airflow. 3. Limit staff contact with the patient. 4. All personnel entering the room must: a. disinfect their hands with alcohol-based hand rub b. put on the following PPE: cone-shaped surgical mask 2 pair of gloves (one under and one over the cuff of the gown) fluid-resistant or impermeable gown full face shield for eye protection 5. Call the Infection Control Unit at 726-2036 or page beeper # 26346 to report the suspect case. 6. If the ED confirms that the patient meets the suspect case definition, clinic will coordinate transport of the patient directly to the ED via wheelchair or stretcher. 7. ED Staff will provide guidance on who will accompany patient from clinic to ED for evaluation. 8. Place a cone-shaped surgical mask on the patient and cover the patient with a clean sheet 9. Page or call Security (6-2121). a. Security personnel must clear the travel route and facilitate transport. b. Security personnel do not require the use of personal protective equipment (PPE) because they will not have direct contact with the patient c. Police and Security will determine the best route to the ED 10. After the patient leaves, close the room and contact ESD (x6-2445); the room will be cleaned and disinfected with hospital-approved, bleach germicidal cleaner per ESD EVD Discharge Cleaning Protocol. 11. If the patient is off campus, call EMS and indicate that the patient needs to be transported to the MGH ED with concern for EVD so that EMS can use appropriate precautions. What should I do if a patient is at home and meets criteria? If the patient is at home; the patient should call EMS and indicate that he/she has been instructed by their physician to be transported to the MGH ED with concern for Ebola so that EMS can use appropriate precautions What should I do for patients who do not have fever or other clinical symptoms of EVD, but do have high or low risk factors as described above? For individuals with these exposures but who are asymptomatic, please notify ID (617-7262000, pager 16136) to discuss whether they require home quarantine for 21 days since last exposure, with twice daily temperature monitoring and rapid reporting of any symptoms or fever > 100.4°F. Infectious Diseases (ID) and Infection Control (IC) will coordinate this monitoring with the Boston Public Health Commission (for persons living within Boston; 24/7 phone number 617-719-5415) or with the Massachusetts Department of Public Health (for persons living in other cities; 24/7 phone number 617-983-6800). What is the proper initial placement of a suspect case in the hospital setting? Initially, Ebola suspect patients will be placed in a dedicated private, Airborne Isolation rooms within the ED. While the CDC does not recommend use of airborne precautions or N95 masks for Ebola, these precautions are both recommended for aerosol-generating procedures, such as intubation. In addition, Ebola suspect patients may have an alternate or additional infection requiring airborne precautions, such as tuberculosis. Therefore, until the patient can be evaluated by the ED, ID, IC, and Medical Intensive Care Unit (MICU) teams, airborne precautions will remain in effect in addition to Ebola Virus Disease (EVD) Precautions until it is determined that airborne isolation is no longer needed. (EVD Precautions are similar to Contact Precautions with specific PPE requirements- see MGH Infection Control Unit website) What laboratory or radiology testing should I do if the patient meets the suspect case definition? Testing (both to confirm Ebola and non-Ebola diagnostic testing) on suspect cases will only be conducted after consultation with ID who will also discuss options with public health authorities. ID will indicate what samples need to be drawn and the ED staff will work with Laboratory Medicine and transport staff to ensure proper retrieval and handling of specimens, if indicated. Where can I find the most current guidance? The most current guidance from the MGH, CDC, Massachusetts Department of Public Health, and Boston Public Health Commission are available at the links below: MGH Infection Control Unit: http://infectioncontrol.massgeneral.org/icu/ 24/7 Coverage: 617-726-2036 during business hours; after hours 617-726-2000 pager 26346 Centers for Disease Control and Prevention Ebola Homepage: http://www.cdc.gov/vhf/ebola/index.html 24/7 Contact: 800-232-4636 Massachusetts Department of Public Health Biological Threats: http://www.mass.gov/eohhs/gov/departments/dph/programs/emergencyprep/threats/biological/ 24/7 Coverage: 617-983-6800 Boston Public Health Commission: http://www.bphc.org/Pages/default.aspx 24/7 Coverage: 617-719-5415 What is MGH doing to monitor the international response? The MGH Center for Global Health is monitoring the situation in Africa carefully, and working diligently with risk management and other officials at Partners and Harvard University to provide appropriate guidance regarding travel abroad and about the repatriation needs of staff. They are also working closely with our governmental and non-governmental partners regarding the global response issues that are evolving. If you have concerns or questions regarding staff traveling abroad or international response efforts, we ask that you please contact Dr. Hilarie Cranmer who is leading the international coordination effort for MGH (617724-1306). Although there are many complex issues at play in this outbreak, we have worked hard to prepare MGH for its potential response, both globally and domestically. We are, as always, proud of the tremendous dedication and expertise of all of our colleagues within the hospital. We are grateful to everyone who has contributed to the response efforts so far, although thankfully we have not yet needed to use our plans. Please feel free to contact one of us if you have questions or need assistance. Sincerely, Paul Biddinger, MD MGH Medical Director for Emergency Preparedness Stephen B. Calderwood, MD Chief, MGH Division of Infectious Diseases Hilarie Cranmer, MD MPH MGH Center for Global Health, Director of Global Disaster Response David C. Hooper, MD Chief, MGH Infection Control Unit