Extrasystoles and Ventricular Tachycardia (Gaya)
advertisement

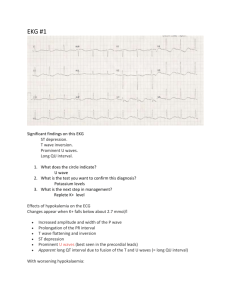
Extrasystoles and Ventricular Tachycardia (Gaya) ‘Extrasystole’ aka ‘ectopic’ aka ‘premature contraction’ An early contraction of the heart independent of its normal rhythm and that arises in response to an impulse in some part of the heart other than the SA node. The extrasystole is followed by a ‘compensatory’ pause, the contraction following the pause is usually more forceful than normal (felt as palpitations) Types of extrasystoles Supraventricular extrasystoles Atrial extrasystole Arising from stimuli discharged in atrial wall ectopic to atrial pacemaker Atrioventricular extrasystole aka nodal extrasystole aka junctional extrasystole One in which the stimulus is thought to arise in the atrioventricular node Ventricular extrasystole One in which either a pacemaker or a re-entry site is in the ventricular structure. Rather common and usually insignificant. However, if present early in the T wave of a preceding beat they can induce ventricular fibrillations and are thus potentially dangerous. Little bit of pathophys 1. Re-entrant signalling (an electrical impulse recurrently travels in a tight circle within the heart, rather than moving from one end of the heart to the other and then stopping, occurs when conduction is abnormally part of the impulse will arrive late and potentially be treated as a new impulse.) By analogy, imagine a room full of people all given these instructions: "If you see anyone starting to stand up, then stand up for three seconds and sit back down." If people are quick enough to respond, the first person to stand will trigger a single wave which will then die out; but if there are stragglers on one side of the room, people who have already sat down will see them and start a second wave, and so on. 2. Enhanced automaticity in some ectopic focus (excitable group of cells outside the SA node). Management Isolated PVCs require no treatment and in healthy individuals be resolved by restoring the balance of magnesium, calcium and potassium within the body. The most effective treatment is the elimination of triggers (particularly the cessation of the abuse of substances such as caffeine, and illegal drugs.) Pharmacological agents o Beta blockers o Calcium channel blockers Electrolytes replacement (Mg and K supplements) Radiofrequency catheter ablation treatment Lifestyle modification o Frequently stressed individuals should consider therapy/support groups. o Heart attacks can increase the likelihood of having PVCs, so exercise and a healthy diet will decrease PVCs by reducing the risk of heart attacks. P wave present but abnormally shaped Normal QRS shape Atrial extrasystole T wave right way up Next P wave has a late arrival 'resets' itself Absent P wave or one very close either side of QRS complex (excitation to both atria and ventricles) Supraventricular systole Early (extra) QRS AV extrasystole Abnormal QRS shape(very wide) T wave inverted SA node unaffected Next P wave on time Ventricular systole AV Ventricular Tachycardia A focus in the ventricular muscle depolarizes with high frequency causing in effect rapid ventricular extrasystoles. 2 classifications Monomorphic ventricular tachycardia means that the appearance of all the beats match each other in each lead of a surface ECG Polymorphic ventricular tachycardia, has beat-to-beat variations in morphology. This most commonly appears as a cyclical progressive change in cardiac axis, previously referred to by its French name torsades de pointes ("twisting of the points"). Pathophysiology The morphology of the tachycardia depends on its cause. In monomorphic ventricular tachycardia, all the beats look the same because the impulse is either being generated from increased automaticity of a single point in either the left or right ventricle, or due to a reentry circuit within the ventricle. Polymorphic ventricular tachycardia, on the other hand, is most commonly caused by abnormalities of ventricular muscle repolarisation. The predisposition to this problem usually manifests on the ECG as a prolongation of the QT interval. Treatment Electrical Cardioversion / Defibrillation A patient with pulseless VT or VF will be unconscious and given high energy (360J with a monophasic defibrillator, or 200J with a biphasic defibrillator) unsynchronised cardioversion. Patients with a stable VT are given cardioversion if the tachycardia exceeds 150bpm. The shock may be delivered to the outside of the chest using an external defibrillator, or internally to the heart by an implantable cardioverter-defibrillator (ICD) if one has previously been inserted. Antiarrhythmic drug therapy Drugs such as amiodarone or procainamide may be used in addition to defibrillation to terminate VT while the underlying cause of the VT can be determined. As hypomagnesia is a common cause of VT, stat dose magnesium sulphate can be given for torsades or if hypomagnesemia is found/suspected. Long term anti-arrhythmic therapy may be indicated to prevent recurrence of VT- Beta-blockers and a number of class III anti-arrhythmics (especially lidocaine) are used For some of the rare congenital syndromes of VT, other drugs, and sometimes even catheter ablation therapy may be useful.




![Cardio Review 4 Quince [CAPT],Joan,Juliet](http://s2.studylib.net/store/data/005719604_1-e21fbd83f7c61c5668353826e4debbb3-300x300.png)