Pharmaceutical-Care-Project
advertisement

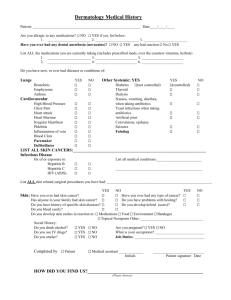
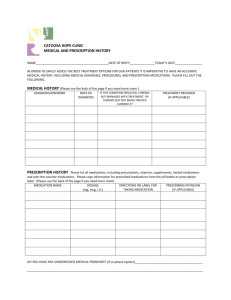
Pharmaceutical Care Project University of Wisconsin-Milwaukee Nursing 707 Kimberly Moriarty Part One: Client Assessment Client expectations and concerns: -Is worried that aspirin caused the blood in his urine -Has taken his medications “for years” and feels comfortable with his pills but is open to a review to make sure they are all appropriate. History of Present Illness: Chief Complaint: “I had blood in my urine two days ago. It went away, but now it’s back and I can’t relieve myself”. History of Present Illness: B.P. is a 73 year old white male who complains of frank hematuria two days ago which resolved later that day. Prior to arrival today, the hematuria returned. He complains of urgency, hesitancy and dribbling along with inability to void. He denies recent trauma, CVA tenderness, and flank pain. Denies previous symptoms of BPH. Had a renal stone about 20 years ago. No recent fevers, weight loss. Does report having the flu 1-2 weeks ago, including diarrhea and vomiting for that time period. Lab values: WBC 17.4 Urinalysis: normal except Sodium 140 RBC 7.0 blood 3+ Potassium 4.2 Hemoglobin 21.1 protein 2+ Chloride 110 Hematocrit 60 RBC >100 Bicarb 17 platelet count 480 Glucose 113 Protime 16 BUN 83 INR 1.6 Creatinine 3.65 PTT 26.1 PSA=2.76 Vital signs include: 150/74, 80bpm, 16, 97.8, 97%RA. Ht=170lbs, Wt=6’0” A recent lipid panel would also be helpful to look at. Past Medical History: -Hypertension, diagnosis date unknown -Hyperlipidemia, diagnosis date unknown -Renal insufficiency, diagnosis date unknown -Benign Prostate Hypertrophy, diagnosis date unknown -Coronary Artery Disease, 1996 -CABG in 1996 -I&D rectal abscess and fistulectomy 1990 Allergies/Adverse reactions: No Known Drug Allergies No Latex, environmental or food allergies Family/Social History: -B.P. is widowed, and retired. Lives in an apartment complex in a one bedroom lower. -He has two sons and one daughter, all live within 15 minutes of him. Children help with cleaning and shopping as needed, but B.P. can take care of his own needs. -His father died of a heart attack, mother of pancreatic cancer. His one brother also has BPH. -B.P. is on Medicare, gets his prescriptions filled at an aurora pharmacy nearby his home. -B.P. used to smoke 1ppd for 25 years, quit in 1981. Denies ever using illicit drugs. Drinks 1-2 mixed drinks per week, prefers whiskey. CAGE negative. -B.P worked in a manufacturing company. Highest level of education was high school with some upper level classes at a community college. -B.P. remains sexually active with a female partner. -B.P. sees his primary care physician annually. Immunizations: -Unknown childhood immunizations, reports having them all -Flu shot 10/1/08 -Pneumonia vaccine 3/14/06 -Tetanus vaccine 2/14/05 Review of Systems/Physical exam: -General: NAD, pleasant, cooperative, good historian -Skin: Negative. No rashes, bruises. Dry and intact -HEENT- Negative. Denies vision changes, wears glasses. Negative for blurred vision, double vision. -RESP: Negative. Denies SOB, cough, sputum. Able to walk 3 flights of stairs without difficulty. -CV: Negative. Denies palpations, syncope, and chest pain. RRR. -GI: Negative. Mildly distended abdomen. Denies recent nausea, vomiting, constipation, diarrhea, abdominal pain. -GU: Positive for urgency, frequency, hematuria, dysuria. -MS: Negative. Normal ROM, NL strength. -CNS: Negative. Denies weakness, numbness, and seizures. -ENDO: Negative. Denies heat/cold intolerance, polyuria, polydipsia -HEM: Negative. Denies bruising, calf pain. Negative for lympadenopathy. -PSYCH: Negative. Denies depression, anxiety. Medication Profile: Lisinopril 5mg by mouth daily Prilosec 20mg by mouth daily Lipitor 20mg by mouth daily Cialis 20mg by mouth as needed Tiazac 180mg by mouth daily Lopressor 50mg by mouth twice a day Dyazide 37.5/25mg by mouth once a day Omega-3 Fatty acids 1200mg by mouth once a day Aspirin 81mg by mouth daily Part Two: Drug Classification and Drug Information Lisinopril (prinivil) MOA: ACE inhibitor. Blocks the conversion of angiotension I to angiotension II, leading to decreased blood pressure, decreased aldosterone secretion. Causes dilation of arterioles and veins, increases renal excretion of sodium and water. Pharm properties: Metabolized in liver, excreted in urine. Onset 1hr, peak 7hr and duration 24hr. Side effects: Headaches, dizziness, insomnia, fatigue, orthostatic hypotension, tachycardia, gastric irritation, nausea, diarrhea, proteinuria, angioedema, cough. Patient denies any of these side effects. Drug interactions: causes decreased hypertensive effects if taken with indomethacin, exacerbation of cough if used with capsacin. No relevant drug interactions for this patient. Prilosec (omaprazole) MOA: Proton pump inhibitor. Supresses gastric acid secretion by inhibition of the hydrogen/potassium system at the secretory surface of the gastric cells. It blocks the final step of acid production. Pharm properties: Meatbolized in liver, excreted in urine and bile. Onset varies, peak is 0.5-3.5 hours. Side Effects: Headaches, dizziness, diarrhea, abdominal pain, nausea, vomiting, cough. Pateint denies any ill effects from this drug. Drug interactions: Will increase levels of wafarin, benzos. Decareses absorption with sucralfate. Not applicable to this patient. Lipitor (atorvastatin) MOA: Antihyperlipidemic. Inhibits HMG co-enzyme A (first step in cholesterol synthesis), decreases serum cholesterol, serum LDL, increases serum HDL, lowers TGs. Pharm Properties: Hepatic and cellular metabolism, excreted in bile. Onset slow, peaks in 1-2 hours. Side Effects: Headaches, flatulence, abdominal pain, nausea, constipation. Pt does report increased flatulence. Drug interactions: Increases dig levels if taken together, Myopathy if used with other coenzyme A inhibitors, antifungals, niacin, or erythromycin. Not applicable to this patient. Cialis (tadalafil) MOA: PDE5 inhibitor. Relaxation of penile arterial and trabecular smooth muscle brought on by accumulation of cGMP. Pharm Properties: Metabolized by liver, excretion in feces. Peaks in 0.5-6 hours. Side Effects: headaches, dyspepsia, back pain, hypotension. Denies any effects after taking this drug. Drug interactions: Not to be used with nitrates or alpha blockers (excluding flomax). Not applicable to this patient. Tiazac (diltiazem) MOA: Calcium Channel Blocker. Inhibits movement of calcium ions across muscle cells which results in depression of the electrical impulse, which slows the velocity of conduction, decreases myocardial contractility and dilate coronary arteries. This leads to decreased cardiac workload and increase of oxygen to myocardial cells. Pharm Properties: Metabolized in liver, excreted in urine. Come in oral and IV forms. Onset orally is 30-60 min, peaks in 2-3 hours. IV has immediate onset, peaks in 2-3 minutes. Side Effects: Dizziness, lightheadedness, headache, edema, bradycardia, flushing, nausea. Patient denies above side effects. Drug interactions: Increases level of cyclosporine, used with caution in those taking beta blockers (may depress AV conduction). Pt currently on a beta blocker. Last EKG normal. Lopressor (metoprolol) MOA: beta blocker. Blocks beta receptor on the heart causing decreased cardiac output, lowering blood pressure. Pharm Properties: metabolized in liver, excreted in urine. Oral and IV forms available. Oral onset is 15min, peaks in 90min and lasts 15-19 hours. IV doses onset immediately, peak in 60-90 minutes and last 15-19 hours. Side Effects: Congestive heart failure, arrhythmias, gastric pain, constipation, diarrhea, nausea, vomiting, impotence. Pt denies these side effects. Drug interactions: Do not use with verapamil, hydralizine, lidocaine, prazosin, NSAIDs, epinephrine. Patient not currently on any of these drugs. Dyazide (hydrochlorothiazide and triamterene) MOA: Diuretic. HCTZ blocks reabsorption of sodium and chloride in early segment of distal convoluted tubule thereby increasing urine production. Triamterene inhibits sodium reabsorption in the renal distal tubule, causing loss of sodium and water and retention of potassium. Pharm Properties: Metabolized in liver, excreted in urine. Onset is 2-4 hours, peaks in 68, lasts 12-16. Side Effects: headaches, nausea, dehydration, hyperglycemia. Pt denies these ill effects. Drug interactions: Increased risk of dig toxicity. Not applicable to this patient. Aspirin MOA: NSAID. Inhibits synthesis of prostaglandins. Inhibits platelet aggregation. Pharm Properties: Metabolized by the liver, excreted in the urine. Onset of 5-30 minutes, peaks in 2 hours and lasts 3-6 hours. Side Effects: nausea, dyspepsia, occult blood loss, dizziness. Patient reports blood in the urine. Believes aspirin to be the cause. Drug interactions: increased bleeding with anticoagulants, Decreased antihypertensive effects with beta blockers. Patient currently is hypertensive. Omega 3 Fatty Acids MOA: Not fully understood. Pharm Properties: Unknown Side Effects: May lead to bleeding if taken in large amounts. Patient denies taking in large amounts. Drug interactions: May increase statin effects. Part Three: Pharmaceutical Care Plan Client teaching plan This patient is primarily in need of reinforced teaching and education about his current drug regimen. His plan includes reinforcement of his medications purpose, and maintaining a routine for administration. He is very independent and manages his care and needs well on his own. This patient does not have any immediate disorders of physical function. He uses glasses for reading only. His physical and cognitive state does not render him in need of any direct assistance with his medication management. He uses a pill dispenser made out for a month in advance. It stays in his kitchen, next to his toaster. He usual morning routine involves corn flakes and toast, taking his meds with breakfast. He denies ever skipping a dose. Since the majority of his meds are taken once a day, his evening dose of lopressor is taken with his dinner. He denies needing a reminder, but a simple watch could be set to alarm twice a day as a reminder. If he forgets a dose, he must make up that dose when he remembers. Lopressor may prove more difficult, as spacing should be 12 hours apart. Maybe switching to an extended release may help to eliminate the need to take it twice. The patient is able to state what his meds do, but not the actual names or dosages. Further education is required. The patient would benefit from a medication identification card that he could carry with information relating to dosage, drug name and purpose. The patient fills his own medication tray each month; perhaps his children would be able to be a double check of dosages and medications. He insists on remaining as independent as possible, but agrees a double check couldn’t hurt. Cognitively, this patient is able to manage his conditions easily. The patient is also unable to verbalize potential side effects of his medications. As stated earlier, he denies any side effects of his medications. A quick reminder of things to be aware of (dizziness, headaches etc) proves valuable to this patient. Prices for the drugs vary according to where they are purchased. The patient reports upward of $800 per month on prescriptions, covered almost entirely by his Medicare. His co pay is minimal, reports about $15. So as of now, medication cost would not impact compliance. Part Four: Evaluation of Drug Efficacy and Pharmaceutical Care Planning Drug Therapy Assessment Correlation between Drug therapy and Medical problems: Dyazide: used to treat hypertension, patient with previously diagnosed hypertension Lopressor: used to treat hypertension, patient with previously diagnosed hypertension Tiazac: used to treat hypertension/angina, patient with previously diagnosed hypertension Lipitor: used to treat hyperlipidemia, patient with previously diagnosed hyperlipidemia Prilosec: used to treat acid reflux. Not in current past medical history. Lisinopril: used to treat hypertension, patient with previously diagnosed hypertension All of the above medications (except prilosec) are indicated because of the patient’s past medical history. He has a significant cardiac history. At a glance all of these medications are indicated. However, a conversation or old records from his cardiologist would prove useful in determining if the patient still requires all of the medications. Furthermore, a lipid panel would also prove useful to determine the efficacy of his Lipitor. Although more information is needed for a determination, it appears this patient is being treated appropriately. Appropriate drug selection: This topic is more difficult to address without knowing more information. The relative safety of the medications is great. These drugs have all been on the market for a significant amount of time. It also appears the therapy has been tailored to the client. He is on a array of different drug to treat his hypertension. It could be assumed that the patient failed therapy on just one or two classes. The prescribing authority must have tailored this therapy to his best interest; although it is impossible to know unless we have more information. All in all, there are no immediate concerns in regards to appropriate drug selection, but more information is needed. Drug Regimen: The prescribed doses of these medications are appropriate and within the normal therapeutic range for each drug. The route is oral, which provides the most safe, convenient, and cost effective. Doses are also scheduled to maximize therapeutic effect and compliance. He does take all his medications at the same time, which proves significant in making an interaction possible, but as of now the patient has not experienced any. The length of therapy is appropriate, as this patient must remain on his antihypertensives to remain therapeutic. His course of prilosec begs more information. The current drug regime does not indicate an intervention. Therapeutic Duplication: There are no therapeutic duplications of drugs in this patient’s regime. He is on different classes of drugs with different mechanisms to manage his hypertension. No problem exists. Drug Allergy or Intolerance: The patient is not intolerant or allergic to any of his medications. No problem exists. Adverse Drug Events: The patient is currently taking aspirin every day. He is now experiencing hematuria. Due to this, he should stop taking it, although it would not be considered an adverse drug event. Discontinuation is in the patient’s best interest until the source is determined. A problem does exist, discontinue aspirin. Interactions: His beta blocker and calcium channel blocker have been shown to depress AV conduction. This does bear some significance with the patient given his cardiac history. This must be monitored on a regular basis. A problem may exist at some point, can be managed with routine checkups. Social or recreational drug use: No problem exists. Not applicable to this patient. Failure to Receive Therapy: A potential problem exists here. Although the patient is highly functional and independent, he may at some point miss a dose of his medication. Further education, family involvement and follow ups are needed to make sure the patient is adherent to his medications. Financial Impact: As of now, no problem exists. The patient is able to get his medications without being financially in trouble. This should be regularly addressed as well to assure the patient is able to afford his medications. Patient Knowledge of Drug Therapy: A problem exists. This patient is deficit in his knowledge of the purpose of his medications, dosages and names. He needs further education to help him understand his regime. A medication card with name, dosage and purpose would greatly benefit this patient. Goals of Drug Therapy The main goal of this client’s drug therapy is preventing complications of a disease. Although more information is needed, his hyperlipidemia and hypertension have damaged his heart. His medications are primarily used to maintain existing function, and prevent the disease from progressing further. All of his prescribed medication fit into this category. The client needs his medications to maintain and prolong his current quality of life. Interventions Interventions for this client include; education about medications names, purpose, dose and frequency. Additional information would include; what to do if doses are missed, potential side effects, and any other helpful hints with each medication. The patient could also benefit from a laminated medication list that he could carry. It would also include current provider’s phone number and pharmacy numbers as well. This further education will help maintain his independence and make him more knowledgeable about his medications. He will be then be more aware of the importance of adherence and remain therapeutic in his treatment. He should also stop taking aspirin until diagnosed and treated by a healthcare professional. The hematuria will only be aggravated by taking aspirin. He also should have his cardiologist and primary care practitioner meet and discuss his medications. If both providers are on the same page, perhaps a new regime could be initiated with fewer medications. The rationale for this is reducing the risk of too many medications, possible drug interactions, and reducing the cost to the client. Monitoring Plan This patient needs to be monitored by his primary care practitioner on a regular basis, about once a year, unless an acute care need arises. At each check up, the patient needs routine labs (CBC, BMP), EKG, vitals and follow up with his current state of health. His blood pressure should be less than 120/80 (JNC 7). In addition, a lipid panel should be drawn to make sure his LDL is less than 100. This outlines some of the goals of treatment as well. The patient could also begin an exercise plan and be evaluated for his nutritional levels. Collaborative Practice This patient would definitely benefit from a multi-disciplinary team looking after his care. His primary care physician would be the main leader, making sure all other players are on the same page. Involving a case manager and nurse practitioner in addition to the regular pharmacy of the client’s choice would complete the coverage. Involving numerous disciplines adds benefit to the patient’s care. By adding a case manager, the patient could have a community asset to help him plan for unexpected needs, financially or even physically. Furthermore, having the client decide a POA would finish off his management. Having more people involved who know him streamlines his care. It would also benefit him, as he could stay active and involved in his care.