pubdoc_12_23112_1015
Haemolytic anaemia
Genetic disorders of hemoglobin:
These are inherited diseases caused by reduced or abnormal synthesis of globin chains.
Hemoglobin synthesis :
The main function of hemoglobin is to carry O
2 to the tissue and to return carbon dioxide(CO
2
) from the tissue to the lungs ,in order to achieve this gaseous exchange they contain specialized protein hemoglobin, each molecule of normal adult hemoglobin (Hb
A) consists of four polypeptide chains α
2
β
2
each with its own haem group .Normal adult blood also contain small quantities of two other haemoglobins: Hb F and HbA
2.
These also contain α chains but with γ and δ chain respectively instead of β chains .
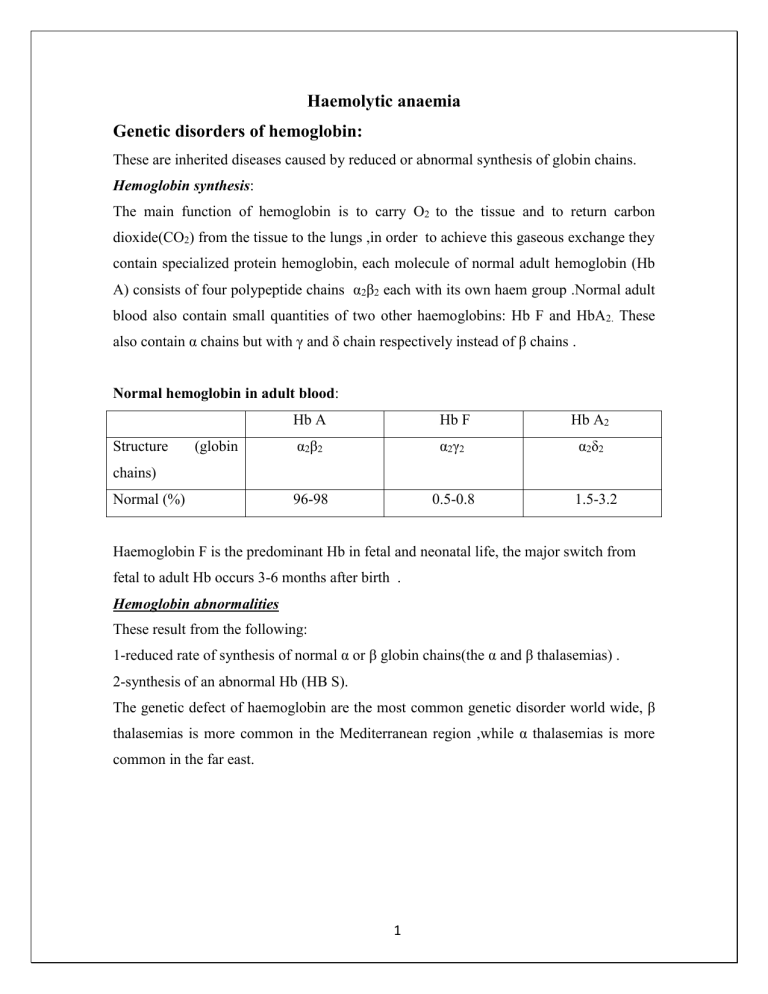
Normal hemoglobin in adult blood :
Structure (globin
Hb A
α
2
β
2 chains)
Normal (%) 96-98
Hb F
α
2
γ
2
0.5-0.8
Hb A
α
2
δ
2
2
1.5-3.2
Haemoglobin F is the predominant Hb in fetal and neonatal life, the major switch from fetal to adult Hb occurs 3-6 months after birth .
Hemoglobin abnormalities
These result from the following:
1-reduced rate of synthesis of normal α or β globin chains(the α and β thalasemias) .
2-synthesis of an abnormal Hb (HB S).
The genetic defect of haemoglobin are the most common genetic disorder world wide, β thalasemias is more common in the Mediterranean region ,while α thalasemias is more common in the far east.
1
Thalassaemias
These are a heterogeneous group of genetic disorders that result from a reduced rate of synthesis of α and β chains.
α thalassemia syndromes : These usually caused by gene deletion. Normally there are four copies of α globin genes ,the clinical severity can be classified according to the number of genes that are missing or inactive:
♦ Loss of all four genes completely suppressed α chains synthesis and because α chains are essential in fetal as well as in adult haemoglobin this is incompatible with life and lead to death in utero( hydrops fetalis) .
♦ Three α genes deletion leads to moderately sever(Hb 7-11g/dl),microcytic hypochromic anaemia with splenomegaly ,this is known as Hb H disease.
♦ The α thalassemia traits are caused by loss of one or two genes and are usually not associated with anaemia.
β thalassemia syndromes
β thalassemia major
:
Pathogenesis: this condition occur in one in four offspring if both parents are carrier of the β thalassemia trait. Either no β chains or small amounts are synthesized ,two important conditions contribute to the pathogenesis of anaemia in thalassemia :
●red cells haemolysis results from unbalanced rates of β globin and α globin chain synthesis, unpaired α chain form insoluble aggregates that precipitates within the red cells and cause membrane damage, these cells are removed by the spleen (extravasculer haemolysis)
●ineffective erythropoiesis which is destruction of red cells precursor inside the bone marrow ,result from α chain precipitation in the erythroblast.
Anaemia results from above mechanisms cause tissue hypoxia which stimulate erythropoietin which cause erythroid hyperplasia and marrow expansion responsible for skeletal changes. Repeated blood transfusion together with ineffective erythropoisis leads to systemic iron over-load.
2
β thalassemia unlike α thalassemia ,the majority of genetic lesions are point mutation rather than gene deletions.
Clinical features :
1 -Sever anaemia becomes apparent at 3-6 months after birth when the switch from γ to β chains production should take place.
2 -Enlargment of the liver and spleen occurs as the result of excessive red cells destruction
,extramedullary haemopoisis, and because of iron overload.
3 -Expantion of the bones caused by intense marrow hyperplasia leads to thalassemic facies and to thinning of the cortex of many bones with a tendency to fracture and bossing of the skull with a(hair-on-end )appearance on x-ray.
4 -The patient can be sustained by blood transfusion but iron overload caused by repeated transfusion is inevitable unless chelating therapy is given.
Iron damages the liver and endocrine organs with failure of the growth, delayed or absent puberty ,diabetes mellitus, hypothyroidisms and hypoparayhyroidism.
Skin pigmentations as a result of excess melanin and haemosidrin gives a gray appearance at an early stages of iron overload.
Most importantly iron damages the heart and in the absence of intensive iron chelating thereby, death occurs in the second or third decade usually from congestive heart failure or cardiac arrhythmia.
5 -infection can occur in thalassemic patient for a variety of reasons:
●In infancy anemic child is prone to bacterial infection.
●If splenectomy has been carried out and prophylactic penicillin is not given
,pneumococcal ,haemophilus and meningococcal infection are likely to occur.
●Yesinia entercolitica occur in iron-loded patient being treated with deferoxamine and it may cause sever gastroenteritis.
● Transmission of viruses(such HIV virus) by blood transfusion, may happened in some patients.
6- osteoporosis may occur ,it is more common in diabetic patient with endocrine abnormalities.
3
Laboratory finding:
1-Hypochromic microcytic anaemia due to reduced the synthesis of normal Hb A with reticulocytosis, nucleated red cells and target cells in peripheral blood film .
2-Haemoglobin electrophoresis reveals complete absence of Hb A and almost all the circulating hemoglobin being Hb F.
3- DNA analysis to identify the genetic defects.
4- Assessment of iron status :these tests can be performed to assess iron over load and include:
♦ serum ferritin which is the most widely used.
♦ serum iron and total iron binding capacity.
♦ bone marrow biopsy.
♦ liver biopsy.
♦ deferoxamine induced iron excretion test.
5- Assessment of tissue damage by iron over-load:
♦ cardiac function assessed by :clinical examination, ECG, chest x-ray and echocardiograghy.
♦ liver function assessed by :liver function tests, liver biopsy ,CT scan and MRI.
♦ endocrine function assessed by: clinical examination (growth and sexual development),glucose tolerance test, thyroid and parathyroid and adrenal function, growth hormone assay and radiology for bone age.
Treatment:
1-Reguler blood transfusions is needed to maintain Hb level above 10 g/dl at all times, this usually require transfusion of 2-3 units every 4-6 weeks.
2-Reguler folic acid is given(5 mg /day).
3-Iron chelating thereby is used to treat the iron over-load, the most established drug is aDeferoxamine which is inactive orally and it is given by separate infusion bag 1-2 g with each unit of blood transfused or can be given by continuous subcutaneous infusion 40 mg/Kg over 8-12 hour,5-7 days weekly. The drug indicated in infants after transfusion of 10-15 units of blood. Deferoxamine may have side effects include: high tone deafness, retinal damage, bone abnormalities and growth retardation.
4
bDeferiprone, is an orally active iron chelator. It may be used alone or in combination with deferoxamine and it is more effective than deferoxamine in removing cardiac iron. Its side effects include arthropathy, agranulocytosis, neutropenia, and gastrointestinal disturbances. cDeferasirox, is the newest orally iron chelator. It is given once daily. Its side effects include skin rash and transient changes in liver enzymes.
4- Vitamin C ( 200 mg/ day), increases excretion of iron produced by deferoxamine.
5- Splenectomy, may be needed to reduce blood requirement which should be delayed until the patient is over 6 years old because of the high risk of dangerous infections post splenectomy.
6- Endocrine therapy: is given either as replacement because of end organ failure or to stimulate the pituitary if puberty is delayed. Diabetes will require insulin therapy.
7- Immunization against hepatitis B.
8- Allogeneic Bone Marrow transplantation.
β thalassemia minor:
This is a common usually a symptomatic characterized by hypochomic microcytic blood picture and mild anemia, a raised Hb A2 ( > 3.5%) confirms the diagnosis
Thalassemia Intermedia:
Are cases of thalassemia of moderate severity who don’t need regular transfusions and this is a clinical syndrome which may be caused by a variety of genetic defects. The patients may show bone deformity, hepatoslenomegaly, extramedullary haemopoiesis and features of iron over load caused by increased iron absorption.
Sickle cell anemia
Etiology and pathogenesis:
Sickle cell disease is a group of hemoglobin disorder in which the sickle β globin gene is inherited. Sickle β globin gene result from single base substitution at position number
6,this leads to an amino acids changes from glutamic acid to valine in the β chain.
Hb S (Hb α
2
β
2 s
) is insoluble and form crystals when exposed to low oxygen tension, deoxygenated sickle Hb polymerized into long fibers and red cells become sickle-like which may block different areas of microcirculations or large vessels causing infarct of various organs.
5
Clinical features :
Sever hemolytic anemia associated with crises, the symptoms of anemia are usually mild in relation to the severity of anemia, this because Hb S gives up oxygen to the tissue easily compared with Hb A. The crises may be vaso-occlusive, visceral, a plastic or hemolytic.
1-Painful vaso-occlusive crises: these are the most frequent and precipitated by many factors such as infection, dehydration, acidosis and deoxygenated states like high altitude, operation ,exposure to cold and obstetric delivery.
Infarct can occur in a variety of organs including the bones, the lungs and the spleen,the most serious vaso-occlusive crises is of the brain which cause a stroke. Hand-foot syndrome (painful dactylitis caused by infarcts in small bones) is frequently the first presentation of the disease and may lead to digits of varying lengths.
2- Visceral sequestration crises: these are caused by sickling within organs and pooling of the blood, often with a sever exacerbation of anaemia. The acute chest syndrome is serious complication and the most common cause of death after puberty ,it present with dyspnea and chest pain ,treatment by analgesia, oxygen and exchange transfusion .
Splenic sequestration present with splenomegaly, falling Hemoglobin and abdominal pain
,it is typically seen in infants and treatment is with blood transfusion ,attacks may be recurrent and splenectomy is often needed.
3-Aplastic crises: these occur as a result of infection with parvovirus or from folate deficiency and characterized by fall in hemoglobin as well as reticulocytes.
4- Hemolytic crisis: characterized by an increased rate of haemolysis with a fall in hemoglobin and a rise in reticulocytes.
5-Other clinical features:
Ulcer of lower legs as a result of vascular stasis and local ischemia.
Enlarged spleen in infancy and early childhood but later is often reduced in size as a result of infarction ( Autosplenectomy).
Pulmonary hypertension.
Proliferative retinopathy.
Chronic damage to the liver due to micro infarct.
6
Pigment gall stones.
Osteomylitis.
Laboratory finding:
1The hemoglobin is usually 6-9 g/ dl, low in comparison to symptoms of anemia.
2Sickle cells and target cells . Features of splenic atrophy ( Howell-Jolly bodies).
3Screening tests for sickling are positive when the blood is deoxygenated.
4Hemoglobin electrophoresis: in HbSS, no Hb A is detected, Hb F is usually 5-
15%.
Treatment:
1Prophylactic: avoid factors known to precipitate crisis, especially dehydration, anoxia, infections, stasis of circulation and cooling of the skin surface.
2Folic acid, (5 mg once weekly).
3Good general nutrition and hygiene.
4Pneumococcal, Haemophilus and Meningococcal vaccination. Hepatitis B vaccination is also given as transfusion may be needed.
5Regular oral penicillin should start at diagnosis and continue at least until puberty.
6Crisis treatment: rest, warmth, rehydration and antibiotics if infection is present.
Analgesia ( paracetamol, non-steroidal anti- inflammatory agent and opiate). Blood transfusion if there is sever anemia with symptoms. Exchange transfusion may be needed if there is neurological damage, visceral sequestration crisis or repeated painful crisis. This is aimed to achieve an Hb S percentage of less than 30 in sever cases and after a stroke is continued for at least 2 years.
7Careful anesthetic and recovery technique to avoid hypoxemia or acidosis.
8Routine transfusions throughout pregnancy are given to those with a poor obstetric history or a history of frequent crises .
9Transfusions: sometimes given repeatedly as prophylaxis to patients having frequent crises or who have had major organ damage (e.g. of the brain). The aim is to suppress Hb S production over a period of several months or even years. Iron overload which may need chelation therapy is common problem.
7
10Hydroxyurea ( 15-20 mg/ kg) can increase Hb F and improve clinical course of patients who are having three or painful crises each year. It should not be used during pregnancy.
11Stem cell transfusion can cure the disease.
12Researches on Butyrates which enhance Hb F synthesis and increase solubility of
Hb S.
13Researches on Gene- therapy.
Sickle cell trait
This is a benign condition in which there is inheritance of normal hemoglobin and sickle hemoglobin ,there is no anemia and normal appearance of red cells in blood film. Haematuria is the common symptom and caused by minor infarcts to the renal papillae.
8